Gwendolen Lorch
Immune-Mediated Skin Diseases
The identification and management of immune-mediated dermatoses is based on understanding the disease pathogenesis. The immune system is focused on host defense and is composed of specific cellular and protein components that develop and function in a highly specific and complex manner to neutralize or destroy dangerous nonself agents while preserving elements of self. However, when the defense system malfunctions or misinterprets signals, the resulting immune response may prove inadequate or even detrimental, leading to a targeted attack on any layer of the skin (epidermis, dermis, hypodermis), adnexa, or cutaneous vasculature. The mechanism of tissue damage includes types I to IV hypersensitivity reactions. Although they do arise in the horse, immune-mediated diseases are relatively uncommon.
Pemphigus Foliaceus
Pemphigus foliaceus (PF) is the most common generalized immune-mediated disease in the horse. The incidence of equine PF has been calculated at 10 per 1000 cases per 10 years. The clinical pathology is the result of antibody production to desmosomal proteins that are crucial to the integrity of squamous epithelial cell–cell adhesion. The antigen–antibody complexes trigger release of proteases that lead to loss of intercellular cohesion and freed nucleated keratinocytes (acantholysis). Provocation sources for PF are thought to be drugs (vaccines, anthelmintics, antimicrobials, and supplements), seasonal allergens, insect bites, stress, systemic disease, and ultraviolet light.
Recognizing Pemphigus Foliaceus
Age at the onset of PF has been reported as early as 2 months to as late as 25.5 years. Pemphigus foliaceus is recognized in ponies, horses, and donkeys, and to date, no breed or sex predilections have been found. Various temporal presentations of PF can occur such that the disease intensifies or recurs on a seasonal basis, in which instance it is thought that warm, humid, sunny weather exacerbates the skin lesions. Pemphigus foliaceus is characterized as a superficial, pustular, crusting, scaling, exfoliative dermatitis that typically waxes and wanes (Table 133-1; Figures 133-1 and 133-2). It should be considered as a differential diagnosis for all skin diseases that have crusting and scaling, with or without exudation.
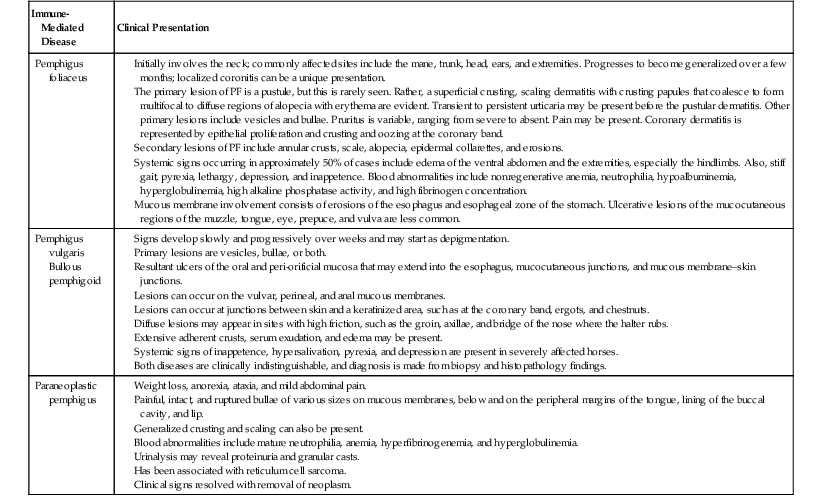
TABLE 133-1
Clinical Signs of Pemphigus
| Immune-Mediated Disease | Clinical Presentation |
| Pemphigus foliaceus | |
| Pemphigus vulgaris Bullous pemphigoid | |
| Paraneoplastic pemphigus | Weight loss, anorexia, ataxia, and mild abdominal pain. Generalized crusting and scaling can also be present. Blood abnormalities include mature neutrophilia, anemia, hyperfibrinogenemia, and hyperglobulinemia. Urinalysis may reveal proteinuria and granular casts. Has been associated with reticulum cell sarcoma. |
Diagnostic Confirmation
The definitive diagnosis of PF is made by a corroborative history and clinical signs in addition to suggestive cytologic and histologic findings. The diagnosis should be confirmed by ruling out other differential diagnoses as well as by finding negative bacterial and fungal cultures. Diagnostic cytology is best obtained from lesions such as an intact pustule or exudate on the undersurface of a crust. Direct impression smears from pustules, undercrusts, or very recent erosions provide one reliable method from which the cell types suggestive of PF are most likely to be found. To collect interpretable specimens for cytology, a pustule should be gently lifted toward the glass slide to enhance sample collection. The glass microscope slide is then pressed onto the site or pulled gently from one end to the other over the lesion. To obtain a cellular sample, it is important to apply pressure directly over the target lesion. Using digital pressure from the index finger or thumb easily accomplishes this while minimizing the chance of breaking the glass slide during the impression smear. Enough pressure has been applied if there is an impression of cell debris on the unstained slide. In addition, crusts can be lifted to reveal the moist undersurface. Collect the moist exudate by gently pressing the undersurface of the crusts several times onto the slide. Alternatively, in a cooperative patient, a 25-gauge needle can be used to gently “lift the lid off” a pustule to expel its contents, allowing an impression smear to be made from the suppurative exudate. The slide is then stained with a commercially available cytology stain (e.g., modified Wright stain such as Diff Quick), and then gently rinsed with water.
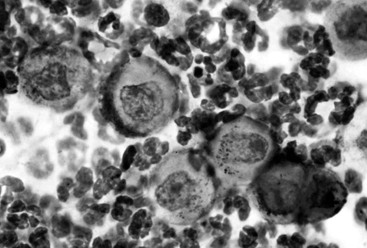
The low-power (10×) microscopic objective is used to scan the slide to select an ideal area for closer examination; the site examined should include neutrophils. Often at low power, individualized, rounded, free-floating nucleated epidermal cells called acanthocytes are seen in the cellular admixture of somewhat smaller appearing neutrophils and occasional to rare eosinophils that may encircle or cling to the acantholytic cells (Figure 133-3). At high power (40× objective, or preferably 100× objective with oil immersion), neutrophils can be seen to be nondegenerate. The absence of bacteria on a cytologic preparation increases the probability of a diagnosis of PF; however, secondary pyoderma can be present in horses with PF. Although acanthocytes are most commonly associated with PF because of the autoantibodies against a cellular adhesion molecule, other causes of acantholysis include dermatoses, such as in Trichophyton equinum dermatophytosis and bacterial folliculitis, in which proteolytic enzymes are released by neutrophils.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




