Matthew Annear
Immune-Mediated Keratitis
Immune-mediated keratitis (IMMK), a recently described group of corneal diseases in the horse, is attracting increasing attention in both the United States and the United Kingdom. Although it is not considered a new or emergent disease, it is the object of several recent review papers and is currently the target of research efforts to determine its underlying etiopathogenesis.
Immune-mediated keratitis is characterized by chronic corneal opacity in the absence of corneal ulceration or significant uveitis. The corneal opacity reflects a lymphoplasmacytic cellular infiltrate, with variable degrees of corneal neovascularization, edema, and fibrosis. These clinical findings are consistent with an immune reaction against corneal autoantigens or unidentified microorganisms. This is further evidenced by a favorable response to immunosuppressive medications and by the histologic characterization of the corneal cellular infiltrate.
Distinguishing IMMK from other causes of keratitis is considered essential, particularly discriminating it from the more common and potentially devastating infectious keratitis (bacterial or fungal). Unlike infectious keratitis, horses with IMMK have minimal ocular discomfort, but this sign cannot be solely relied on for diagnosis, and cytology and culture should be performed to help rule out infectious agents. Immune-mediated keratitis is also distinguished clinically from eosinophilic keratitis. Although some features of IMMK are similar to those of eosinophilic keratitis, the latter generally has a shorter and often self-limited course. Eosinophilic keratitis typically manifests as a plaque on the corneal surface, revealing a preponderance of eosinophils on cytologic analysis. This chapter focuses on the clinical signs, diagnosis, and treatment of IMMK in the horse.
Clinical Signs
Immune-mediated keratitis typically manifests as a unilateral ocular disease in middle-aged horses, although bilateral ocular involvement is also reported, and the ages of affected horses can vary widely. The classic clinical findings include a lymphocytic-plasmacytic corneal cellular infiltrate, often accompanied by corneal neovascularization, edema, and fibrosis. The specific location of the cellular infiltrate varies between cases, and this feature has been used to divide the disease into subtypes that have different clinical manifestations and prognostic recommendations. In the United States, IMMK has been classified into four subtypes: superficial stromal, midstromal, endothelial, and epithelial IMMK.
Superficial stromal keratitis is the most common type of IMMK, often manifesting as a corneal opacity in the ventral or central aspect of the cornea. It is characterized by a lymphoplasmacytic cellular infiltrate in the superficial layers of the corneal stroma, encroached on by superficial corneal neovascularization and associated mild corneal edema. The corneal infiltrate often increases in size and density and then declines, in a recurring fashion, while sparing the deeper corneal stroma.
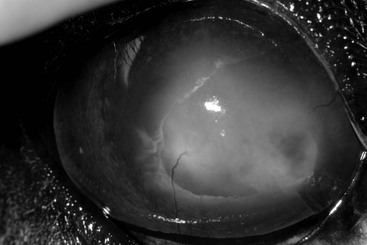
Midstromal IMMK usually presents as a more densely opaque region of the cornea, typically at the lateral, ventral, or central aspect of the cornea (Figure 146-1). The corneal cellular infiltrate is often more marked and focused at the middle depth of the corneal stroma. Corneal neovascularization is at a similar stromal depth, and consequently less branching in appearance, and there may be a mild degree of corneal edema associated with the lesion. Similar to superficial IMMK, the size and the degree of inflammation associated with the lesion typically wax and wane over time.
Endothelial IMMK appears clinically as a slowly progressive area of corneal opacification that often begins ventrally or laterally and may progress to cover a large area of the cornea (Figure 146-2). The opacity is largely a consequence of corneal edema that follows the development of a less obvious cellular infiltrate, appreciable at the level of the corneal endothelium. The corneal edema thus appears to reflect corneal endothelial dysfunction, and the corneal neovascularization in these cases is typically quite mild. Because of the progressive corneal edema, secondary ulcerative bullous keratopathy can be a manifestation of endothelial IMMK. Should ulceration develop, ocular discomfort can be anticipated, although pain is otherwise minimal to absent.
A fourth subtype, epithelial IMMK, has also been described. Epithelial IMMK is characterized by multifocal punctate epithelial opacities that are free of corneal neovascularization. When included in the spectrum of IMMK subtypes, it is the least common manifestation and must be distinguished from equine herpesvirus keratitis.
Geographic differences in the clinical signs and therapeutic response of IMMK are well documented. In the United Kingdom, IMMK is categorized into four subtypes: chronic superficial keratitis, chronic recurrent keratitis, endotheliitis, and epithelial keratopathy. Of these, chronic superficial keratitis and endotheliitis are clinically similar to the superficial and endothelial types of IMMK described in the United States, but both are reported to respond more readily to topical treatments. Chronic recurrent keratitis manifests as periodic and self-limited deep corneal stromal edema, neovascularization, and fibrosis. As with other subtypes of IMMK, pain is not an obvious feature of chronic recurrent keratitis unless secondary ulceration develops. Epithelial keratopathy manifests as avascular central areas of corneal epithelial thickening that reportedly respond rapidly to treatment.