14 Idiopathic chronic gingivostomatitis with extraction leading to cure
ORAL EXAMINATION – CONSCIOUS
The cat would not allow conscious examination of the face or oral cavity.
ORAL EXAMINATION – UNDER GENERAL ANAESTHETIC
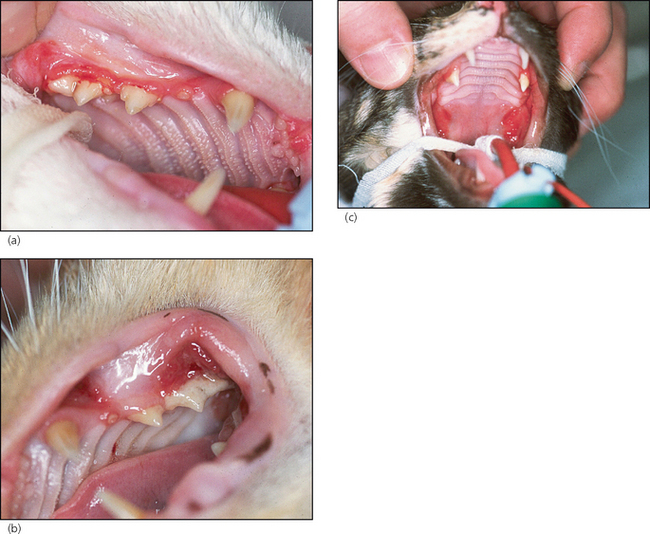
In summary, examination under general anaesthesia identified a severe generalized oral inflammation. The gingivae as well as the buccal mucosa and the glossopalatine folds were intensely inflamed (Fig. 14.1a–c). Moderate amounts of plaque and calculus were present on the buccal aspects of the upper premolars. All teeth were present and showed no evidence of periodontitis.
RADIOGRAPHIC FINDINGS
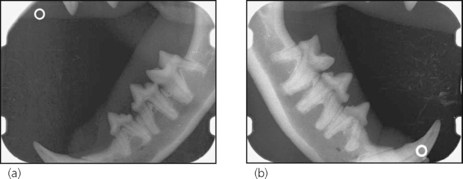
No obvious pathology (Fig. 14.2a, b) could be identified on any of the 10 views.