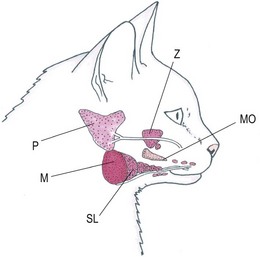
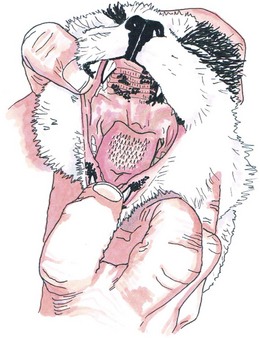
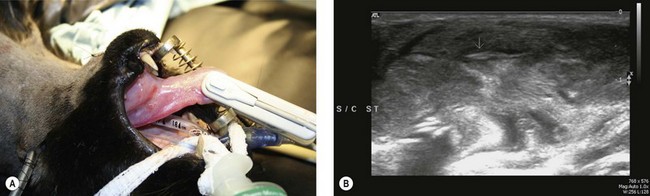
Chapter 49 A variety of conditions affect the feline head, some of which are common. If disease is located in an area that is readily visible to the owner (e.g., neoplasms or inflammatory conditions of the skin) then early recognition and prompt treatment is possible. However, other conditions that are located in regions that are not easily visible (e.g., inside the mouth) are often only detected at a later stage when the cat becomes clinically affected: late diagnosis and the invasive nature of some conditions of the head can influence the prognosis. In this chapter some general information will be given about head examination, imaging, and some of the common diseases, with more specific sections on the tongue, tonsils, salivary glands, chin, cheeks, and lips. The reader is referred to other chapters in this part (Chapters 50 to 58) for detailed information on other organs or parts of the head. The lips in the cat are small and relatively immobile compared to the dog. They form a large rima oris, with the upper and lower lips meeting at the commissure caudally. The lips consist of skin, muscle, and mucosa and contain numerous small scattered salivary glands. The cheeks form the buccal vestibule, which receives salivary secretions from the parotid, molar, and zygomatic salivary glands. The hard palate separates the oral and nasal cavities and is formed from the incisive, maxillary, and palatine bones. The oral aspect of the hard palate is covered by thick mucosa with transverse folds (rugae) that are continuous with the gingiva rostrally, laterally, and the soft palate caudally. The floor of the oral cavity is supported by paired mylohyoideus muscles passing between the mandibular bodies. The ventral oral mucosa has two protuberances to either side of the lingual frenulum known as sublingual caruncles, marking the opening of the mandibular and sublingual salivary ducts.1 The intrinsic muscles of the tongue consist of longitudinal, transverse, and perpendicular fibres. The extrinsic muscles have an osseous origin and radiate into the tongue, and they include the styloglossal, hypoglossal, and genioglossal muscles.2 The mylohyoid muscle suspends the tongue between the mandibular bodies and is important for the induction of deglutition. The vascular supply to the tongue is primarily from the paired lingual artery, supplemented by the paired sublingual artery, and both of these arteries arise from the linguofacial trunk. The innervation of the tongue is from the lingual branch of the mandibular nerve, the chorda tympanii of the intermediofacial nerve, the glossopharyngeal nerve, and the vagal nerve.2 These nerves are individually responsible for sensations such as pain, heat, and taste. The hypoglossal nerve is responsible for motor function, and damage to this nerve will result in paralysis of the tongue.2 The two palatine tonsils are located in the lateral pharyngeal walls and they consist of multiple subepithelial lymph nodules. They have efferent lymphatics only and their function is to provide an immunologic barrier to protect the respiratory and alimentary systems. They are located in a fossa, the medial wall of which is formed by a falciform fold from the soft palate, the tonsilar fold.2 Cats have five major salivary glands (parotid, mandibular, sublingual, molar, and zygomatic) (Fig. 49-1); the molar gland is absent in the dog and humans. The mandibular and sublingual glands empty by separate duct systems, which may exit to a common papilla (sublingual caruncle) just lateral to the frenulum of the tongue. Figure 49-1 Diagram showing the salivary glands of the cat. M, mandibular; Mo, molar; P, parotid; SL, sublingual; Z,zygomatic. The parotid gland is the largest salivary gland. It lies ventral to the ear canal and it slightly overlaps the masseter muscle. The posterior facial vein enters its ventral border. The parotid duct leaves cranioventrally, passes over the masseter muscle, and enters the mouth in a small papilla opposite the most prominent cusp of the last premolar tooth. Some accessory parotid gland tissue can be seen at the cranial end of the duct just in front of the zygomatic gland.1 The mandibular gland lies caudal to the masseter muscle and ventral to the parotid. The posterior facial vein crosses over the mandibular gland. The mandibular duct leaves the gland medially and runs craniomedially in close association with the sublingual gland. It passes between the extrinsic muscles of the tongue and then continues craniad against the oral mucosa, running parallel to the mandible to open at the apex of the sublingual papilla, accompanied by the sublingual duct.1 The sublingual gland is closely associated with the mandibular gland caudally. It extends cranially with the sublingual duct, running in close association with the mandibular duct.1 Cats that have undergone trauma rather than those presenting for chronic or non-traumatic disease may have other life-threatening injuries that require immediate attention and it is therefore important that the reader is familiar with the preoperative assessment of these cases (see Chapter 1). For example, a cat with an avulsed chin may also have concurrent mandibular or maxillary fractures or brain injury. Once the animal is stable, further examination of the head injuries can be undertaken. For uncooperative cats this may need to be performed under sedation or general anesthesia. A thorough examination of the head should involve a visual inspection looking for asymmetry, swellings, ulceration, and trauma. The mandibular salivary glands and the submandibular lymph nodes should be palpated just caudal to the skull. Injury to the chin and lips will usually be obvious to the observer, except perhaps in long-haired cats. The inside of the mouth can be inspected in amenable animals by placing the first finger on the lower incisors and pulling the chin distally, keeping the thumb and middle finger of the other hand on the lips just caudal to the canine teeth (Fig. 49-2). The hard palate should be inspected for signs of trauma or bruising. The dental arcades should be evaluated for tartar and broken or missing teeth. Trauma or disease of the rostral tongue should be easy to identify, but conditions affecting the caudal portion can be missed. To aid visualization of the caudal part of the mouth it is useful to place a finger on the tongue to depress it. Normally, the tonsils in a cat are not visible; however, with certain diseases the tonsils may protrude from the crypt and show a change in size and appearance. Salivary gland conditions can result in ranulas (Fig. 49-3). A finger can be used to press dorsally in the intermandibular space causing displacement of the tongue so that the subglossal area can be inspected. A common location of squamous cell carcinomas is in the sublingual area near to the frenulum of the tongue. Figure 49-2 Examination of the cat’s mouth is facilitated by holding the head steady with one hand and using the first finger of the other hand to open the lower jaw. Figure 49-3 An 18-year-old cat presented with a three week history of progressive increase in difficulty eating and a mild pyrexia. There was a firm intermandibular swelling and purulent material was aspirated from this mass. (A) On oral examination there was sublingual swelling and a ranula. (B) Ultrasound evaluation revealed a structure suspected to be a foreign body (arrow). (C) A needle was placed preoperatively with the tip adjacent to the suspected foreign body to aid surgical exploration. (D) A grass seed was removed at surgery. (E) The ranula was marsupialized in an attempt to decrease its size. An esophagostomy tube was placed for postoperative feeding until the cat was able to prehend orally again. A condition known as feline orofacial pain syndrome (FOPS) has been described in one study.3 This is a pain disorder of cats relating to behavioral signs of oral discomfort and tongue mutilation. The condition primarily affects Burmese cats and is characterized by an episodic, typically unilateral discomfort with pain-free intervals. The discomfort is apparently triggered, in many cases, by mouth movements. The majority of cases in this study had a history of mild oral lesions and a small number of cases experienced their first sign of discomfort during eruption of their permanent teeth. The degree of pain these cats express seems to be unrelated to the severity of oral lesions and is therefore thought to be a neuropathic or anxiety-related condition. In cases of suspected neoplasia, a baseline check for metastases should be performed and include three-view thoracic radiographs (see Chapter 9). Survey radiographs of the affected area of the head can provide useful information about whether underlying bone is involved and radiographs will be necessary in trauma cases to assess for the presence of fractures. Intraoral and oblique radiographs can be particularly useful as they avoid superimposition of bony structures. More advanced imaging such as computed tomography or magnetic resonance imaging may be indicated in certain situations such as cases with neoplasia, prior to surgical planning or radiation therapy. Ultrasonography can be useful for investigation of soft tissue inflammation of the tongue and detection of foreign bodies (Fig. 49-3B) and it has been used in one study to help delineate soft tissue margins of lingual squamous cell carcinoma.4 If sedation is required to obtain the aspirate, it is also recommended to consider taking a biopsy. A biopsy is crucial for obtaining a sample for histopathologic examination to enable an accurate diagnosis and plan appropriate treatment; biopsy of masses should be undertaken prior to attempting surgical resection. It is important to obtain a deep sample as oral lesions are frequently infected, necrotic, or inflamed. Large samples that include healthy tissue at the edge and also include deeper areas of the lesion will increase the diagnostic yield. Lesions such as feline oral squamous cell carcinoma should never be biopsied through the skin but rather through an intraoral incision. An intraoral biopsy prevents seeding of the tumor into the surrounding normal external tissues. These tissues may be required for local reconstruction after oral tumor excision and, thus, need to be preserved without tumor contamination. For more details on different biopsy procedures see Chapter 14. Many conditions around the head will not be confined to a single organ or area. Neoplasia, for example, may primarily appear to affect the chin or lips but closer inspection and further imaging may reveal invasion into the bone of the mandible or maxilla. For further information on diseases of the different parts of the head the reader is referred to Chapters 50 to 58. Oral neoplasia overall is common in cats, accounting for 3–12% of all feline neoplasms.4 Differential diagnoses in cats with oral masses include dental disease, malignant tumors, benign abnormalities (e.g., ranulas), and infections.5–8 Neoplasias affecting the mandible and maxilla are discussed in detail in Chapter 55. In feline cases of oral pharyngeal neoplasia the tongue is the most frequent tumor site, followed by the gingiva.6 In a survey of 340 cats with cutaneous neoplasia, the head was the most common site for basal cell tumors, mast cell tumors, and squamous cell carcinomas.9 The general characteristics of skin tumors are discussed in detail in Chapter 20. Oral squamous cell carcinoma is a malignant tumor that may occur anywhere within the oral cavity. It is locally invasive, infrequently metastasizes to ipsilateral regional lymph nodes, and rarely spreads to distant sites. Given the local invasiveness the prognosis for this fast-growing, invasive tumor in cats is grave, so it is vital to identify and treat the condition early. The average reported duration of survival after diagnosis of this tumor has been reported as two months.8 There is no sex or breed predisposition, although entire male cats were more commonly affected in one study.8 The gingiva, tongue, and sublingual region are the most commonly reported sites of squamous cell carcinoma.6,8 Mucosal ulceration, necrosis, and severe suppurative inflammation are commonly associated with oral squamous cell carcinoma. There may also be mucosal swelling in the absence of ulceration, or animals may be presented solely for chin enlargement. Gingival squamous cell carcinoma often invades the underlying mandible or maxilla, leading to severe and extensive tumor involvement of the bone in that area and marked osteolysis on radiographs. In addition to osteolysis, there is commonly periosteal new bone formation and osseous metaplasia of tumor stroma detected on radiography and computed tomography (CT) evaluation.8 Although several environmental risk factors have been recognized, the cause of feline oral squamous cell carcinoma remains poorly defined. Various potential contributing factors have been suggested (Box 49-1).7 To date, no therapies or combinations of therapy have shown great success in treating this tumor. Local and regional disease control is the treatment goal. Surgery such as mandibulectomy (see Chapter 55), radiation therapy (see Chapter 15), or radiation therapy combined with chemotherapy (see Chapter 16) are the principal treatment modalities used. The one-year survival rate is generally less than 10%, with a median survival time of approximately three months for most therapies. The overall poor survival times in cats with oral squamous cell carcinoma may reflect the tumor’s location and aggressive behavior, as sublingual and maxillary tumors are rarely resectable, and also the fact that this tumor is often diagnosed late in the course of the disease. Assessing an individual patient’s tumor stage and location is critical in advising an owner regarding possible treatment options and likely outcome. Early diagnosis followed by aggressive local treatment and appropriate supportive care is the best way to improve survival times. Recurrence despite aggressive surgical resection is common, thus multimodality therapy appears to be indicated. Feline fibrosarcoma is one of the most common subcutaneous neoplasms in cats and the second most common feline oral neoplasm in one survey of 371 cases.5 It is a locally aggressive tumor with a moderate metastatic rate and high recurrence rates.10 Oral fibrosarcoma affects cats of a wide age range, but with a median age of 10 years.5 The tumor is usually located in the gingiva or palate, arising from the submucosal stroma. It is locally infiltrative and causes local destruction of bone and muscle.5 Aggressive surgical excision is the treatment of choice, but unfortunately recurrence rate is high due to poor local disease control. The eosinophilic granuloma complex was reported in 17 related Norwegian forest cats and the high prevalence of the disease in this population is suggestive of a genetic background.11 There may also be a viral etiology. The lesions of acute feline calicivirus infection can appear similar; they are of a transient vesiculo-ulcerative nature and involve, to varying degrees, the palate, tongue, gingiva, lips, nasal philtrum, and oral fauces. Chronic ulceroproliferative faucitis is a specific but uncommon sequela to persistent feline calicivirus oral carriage.12 Abscesses around the head are common sequelae to cat fight or bite injuries. The normal flora of the cat’s mouth includes strains of hemolytic staphylococci, β-hemolytic streptococci, Pasteurella multocida, Escherichia coli, and fusiforms13 so abscesses are often associated with these bacteria. Affected animals may present with depression, difficulty eating, pyrexia, and obvious swelling. In early cases, careful inspection may be required to find a puncture hole or small scab. Treatment is usually successful by provision for ventral drainage and parenteral antibiotics. In more severe cases, in animals that are also systemically unwell (e.g., with pyrexia, dehydration, etc.), more intensive treatment would be recommended with intravenous fluids, drainage, and flushing the abscess cavity in combination with systemic intravenous antibiosis. Skin necrosis may occur secondarily to a large abscess that has formed rapidly causing local ischemia of the skin: the dead skin will slough or can be debrided as part of the management (Fig. 49-4). These lesions are also very painful so analgesics should be administered. Unless contraindicated, non-steroidal anti-inflammatory drugs are recommended in these cases. Alternatively, opioids can be administered to hospitalized patients. The tongue is prone to injury in the cat either as a result of self-inflicted injury as the cat bites its own tongue during a traumatic incident (Fig. 49-5) or from a foreign body such as a fishing hook or needle and thread. Small lesions can be left to heal by second intention. More severe lacerations should be repaired using simple interrupted sutures of absorbable suture material such as 2M poliglecaprone or polyglyconate. If a proportion of the tongue is lost due to necrosis or trauma then intravenous fluids and provision for feeding via a tube may be required in some cases until the cat is able to prehend food on its own. In dogs, resection of up to 50% of the tongue can be performed without major complications; however, conclusive evidence regarding the success of glossectomy in cats is unavailable. Cats are generally less tolerant than dogs of procedures that affect their ability to eat (e.g., mandibulectomies and maxillectomies) so therefore their postoperative recovery from large glossectomies (up to 50%) is less predictable. In addition to difficulties in eating, the ability to groom, which is an important aspect of their behavior, will also be severely compromised. Figure 49-5 A five-year-old male domestic short-haired cat that presented after a suspected road traffic accident. There was a full thickness central wound on the tongue suspected to be secondary to the cat biting through the tongue. The lateral margins of the tongue were intact and no specific treatment was required aside from placement of a feeding tube to bypass the mouth while the laceration healed. Gastrointestinal foreign bodies are relatively common in cats. Fastidious grooming habits and the anatomy of the tongue with its backward facing barbs makes expulsion of sticky foreign material difficult in the cat. Thread and sewing needles are common gastrointestinal foreign bodies and the thread is most commonly anchored at either the tongue or the pylorus – a thorough examination of the mouth, including the sublingual area, is necessary for the thread or a needle.14 In a review of 24 cats with gastrointestinal linear foreign bodies, 13 had the linear foreign bodies wrapped around either the base of the tongue or in the sublingual area at presentation, but in six of these cats this was missed at first inspection.15 Cutting and the release of the foreign body may be successful in some cats and can avoid the need for intestinal surgery if clinical signs do not warrant immediate surgical intervention.15 When considering conservative management it is important to hospitalize the cat and monitor it clinically, radiographically, and hematalogically for any changes that may indicate the need for subsequent surgical intervention15 (see Chapter 29).
Head
Surgical anatomy
Lips, cheeks and mouth
Tongue
Tonsils
Salivary glands
General considerations
Clinical examination and signs

Feline orofacial pain syndrome
Diagnostic imaging
Biopsy
Surgical diseases of the head
Neoplasia of the head
Squamous cell carcinoma
Fibrosarcoma
Inflammatory disorders of the head
Abscessation
Surgical diseases of the tongue
Tongue trauma

Foreign bodies
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine

