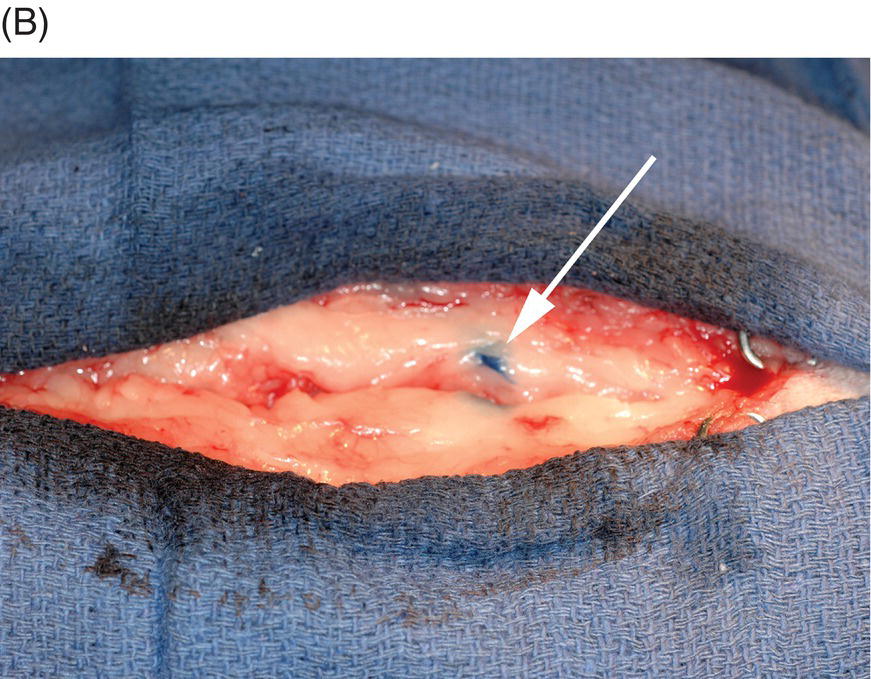
29 James M. Fingeroth and Brigitte A. Brisson As outlined in Chapters 15 and 28, the fundamental purpose of therapeutic surgery is alleviation of compression and mechanical distortion of the spinal cord and nerve roots. Spinal cord compression results in varying degrees of neurologic deficits at and distal to the site of the lesion, while nerve root compression (especially dorsal root and ganglion compression) is felt to underlie much of the discomfort associated with intervertebral disc herniation (IVDH). To achieve these goals, the surgeon should have adequate clinical and imaging data that demonstrate the vertebral level of the lesion and whether there is lateralization to one side or the other. Armed with these data, the surgeon can select what he or she feels is the best bone removal approach that will provide sufficient access for removal of the extruded disc, with minimal iatrogenic trauma to the spinal cord. A good rule of thumb when doing spinal disc surgery is to try to avoid any direct contact with or manipulation of the dural tube and contained spinal cord. While not always achievable in clinical practice, this guiding philosophy should always be forefront in the mind of the spinal surgeon, and every effort should be made to minimize such contact/manipulation if it cannot be avoided outright. The normal spinal cord is sensitive to contact/manipulation and can become injured (with corresponding neurologic deficits) as a consequence [1, 2]. This sensitivity/vulnerability is only accentuated in an already compromised spinal cord that has sustained the effects of concussion and compression from a herniated disc. The reader is referred to other surgical texts and atlases for more detailed descriptions of the various techniques used to access the vertebral canal for removal of herniated disc material. It is of course imperative that the proper spinal location be approached. In ventral approaches to the cervical spine, common landmarks for counting intervertebral disc spaces include palpation of the midline ridge on the ventral arch of the atlas and the larger transverse processes of the C6 vertebrae. For dorsal approaches to the cervical vertebrae, the distinct spinous process of the axis (C2) and the much taller spinous process of T1 (compared with C7 or spinous processes more cranially) are reliable landmarks. In the thoracolumbar spine, palpation of the ribs and transverse processes can be used, but this can require larger incisions and may be difficult in obese patients. An alternative is to radiographically identify vertebrae using a hypodermic needle. The needle (20–25 gauge, depending on patient size) is usually placed aseptically into a dorsal spinous process close to the anticipated surgical site after the initial clip and prep for surgery and then radiographed with the patient in lateral recumbency to identify the precise vertebra in which the needle is located. Either the needle can be drilled securely into the spinous process, the needle hub can be aseptically cut off with the balance of the needle left below the skin (to be found by palpation in the operating room and then guiding the incision), or else a small aliquot of dye (e.g., methylene blue) can be injected into the dorsal aspect of the spinous process and identified visually after incising the skin (Figure 29.1). The needle or dye need not be at the precise proper level of the disc herniation; once one knows the location of the needle or dye, the vertebrae can be counted cranial or caudal as needed to identify the proper location for dissection. When MRI has been used for diagnostic imaging, these radiographs also serve to verify the vertebral and costal formula for the particular patient, as some dogs may have more or fewer lumbar vertebrae or ribs than standard. Although this can be assessed using various MRI sequences (the dorsal view is often best for this), some surgeons prefer radiographic images for this purpose. Figure 29.1 (A) Lateral radiograph depicting a hypodermic placed percutaneously into a dorsal spinous process (in this example, at T4). The needle is placed approximately at the location where the approach to the vertebral canal is planned, based on palpation, and then the needle hub aseptically cut off. The radiograph then serves to identify the precise location of the needle, which can then be used during the surgical dissection to assure that the proper site for laminectomy is being approached. As long as the needle is placed within the dimensions of the surgical incision, it need not be placed exactly at the intended level. Care should be taken to secure the needle’s tip securely into the bone and to avoid dislodging it during the balance of patient preparation and transport to the operating room or during draping and dissection. (B) As an alternative or adjunct to leaving the hypodermic needle in situ after confirming its location radiographically, a small aliquot of sterile methylene blue, USP, can be injected into the dorsal spinous process, and the needle removed if desired. During dissection, the dye can be observed as shown here and used to determine the correct location for the laminectomy. The advantage of leaving the needle in place is that it provides both tactile and visual cues during draping, incision, and dissection. The disadvantage is that the needle can become dislodged, and though usually found in close proximity to the radiographed spinous process, some uncertainty is introduced. The use of dye mitigates this problem. Source: Photos courtesy of Dr. William Thomas.
General Principles of Spinal Surgery for Intervertebral Disc Herniation
Goals
Procedures

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


