Kim A. Sprayberry
Gastroduodenal Ulcer Syndrome in Foals
Gastric emptying is delayed when the outflow tract is functionally or mechanically obstructed. Functional obstruction develops when ileus or hypersecretion of fluid and distension in the proximal small intestine prevent peristalsis and aborad movement of luminal contents, and mechanical obstruction arises when the pylorus or duodenum is blocked by narrowing or a luminal mass (uncommon). Obstruction of gastric emptying in equine species is most frequently observed in foals and is most often a result of duodenal stricture that has developed in association with gastroduodenal ulcer syndrome (GDUS). Systemic illness of any kind may predispose foals to development of ulcers, but inflammatory disease of the intestinal tract, such as enteritis or enterocolitis, increases the likelihood of foals developing gastric and duodenal ulcers of a severity that can lead to life-threatening complications.
Veterinarians’ knowledge about the prevalence and pathogenesis of ulcers in horses has increased with increasing availability of equipment and tools for evaluating gastric physiology, and current thought regarding the genesis of ulcers acknowledges that the process is multifactorial and more complicated than simple injury of cells by excess gastric acid. For instance, the disease conditions that predispose to ulceration in the squamous portion of the stomach differ from those that cause ulcers in the glandular portion, and foals, in particular, can develop severe ulcers even while being treated prophylactically with effective antiulcer medications. Moreover, ulcerative disease in neonatal foals is likely a different condition from that in older foals. Administration of proton pump inhibitors, which effectively raise gastric pH, is known to predispose humans, at least, to colonization of the gastrointestinal (GI) tract and the respiratory tract with bacterial pathogens, calling into question the practice of giving foals antiulcer medications prophylactically.
This chapter reviews the clinical signs, pathogenesis, diagnostic findings, and treatment of gastric emptying obstruction developing as a complication of GDUS and its complications in foals.
Gastric Emptying in Health
The flow of both solid and liquid material from the stomach is determined by cycles of gastric peristalsis that create a pressure gradient between the stomach and duodenum. Smooth muscle tone in the proximal part of the stomach causes outflow of fluid contents, and waves of aborad peristaltic contractions in the antrum promote the exit of solid contents. The pylorus retains feedstuffs and regulates the passing of solids out of the gastric lumen. Pyloric tone serves to retain feed in the stomach until mixing and churning have triturated solid ingesta into small particles for maximum surface exposure to acid in the stomach and digestive enzymes in the small intestine. Fluid ingesta such as water and milk are not subject to retention by the pylorus. In health, the pylorus appears to remain open much of the time, permitting backflow of duodenal contents into the stomach. This duodenal reflux, along with swallowed saliva, causes the spontaneous increases in luminal pH seen in fasted horses, which secrete acid in the stomach continuously irrespective of whether feed is being ingested. The bicarbonate-rich duodenal fluid may constitute a protective factor for the gastric mucosa, although gastric fill and antral motility maintain the flow of gastric contents in the aborad direction most of the time.
The passage time of water from the stomach of healthy foals is on the order of 5 minutes, with milk emptying time taking longer at 2 hours or less; times longer than 2 hours should be considered prolonged. Similarly, in adult horses with normal GI tract motility, passage of water is rapid but complete emptying of hay may take as long as 24 hours.
During normal grazing, ingesta does not fill the stomach dorsal to about the level of the cardia. Gastric contents become vertically stratified, with a mat of coarser, newly ingested material floating atop material that grows increasingly granular and dense ventrally. The pH also changes vertically, being highest in the coarser material at the top and lowest ventrally, in the glandular portion of the mucosa where parietal cells in the gastric glands secrete hydrochloric acid. Because ingesta from the lower, acidic strata do not normally have prolonged contact with the region of squamous mucosa above the fill line, the squamous epithelium does not have, and under normal circumstances does not need, protective mechanisms for contact with strong acids. The glandular portion of gastric mucosa, which secretes acid and pepsin, is armored for immersion in acidic fluid by a bicarbonate-rich layer of mucus through which the secreted hydrogen ions can migrate from parietal cell to lumen, but not in the opposite direction.
Pathogenesis
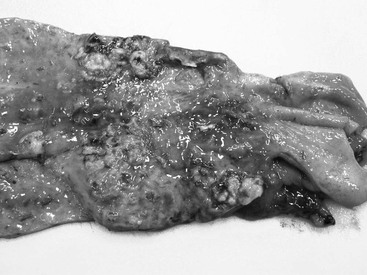
Duodenal ulcers and duodenitis are considered the primary lesion in gastric outflow obstruction (Figure 180-1). Mural inflammation and disrupted motility impair gastric emptying to various degrees, resulting in secondary gastric squamous ulceration and reflux esophagitis. If the inflammation in the duodenal wall progresses to fibrosis and contracture, permanent narrowing or stricture can result. The pathogenic events leading to ulceration of the duodenal mucosa are not known but may involve mucosal contact with gastric acid in the face of systemic illness and hypoperfusion or direct cellular injury by pathogenic viruses or bacteria. In humans, the most frequent causes of duodenal ulcers are Helicobacter pylori infection, low-dose aspirin treatment, and use of other nonsteroidal antiinflammatory drugs (NSAIDs). An interesting difference from a comparative aspect is that chronic and significant bleeding and acute, emergent hemorrhage are the chief morbidities associated with duodenal ulcers in humans; transendoscopic hemostasis by use of hemoclips, injection of procoagulants or vasoconstrictors, thermocoagulation, or application of hemostyptic sprays is a first-line treatment, and in some instances transcatheter arterial embolization of the gastroduodenal artery or one of its tributaries is necessary. Bleeding, including death from exsanguination in one report, has been reported in foals with duodenal ulcers, but perforation or duodenal stenosis and permanently impaired gastric emptying are the chief clinical concerns. Crohn’s disease, a form of human inflammatory bowel disease that affects the mucosa and deeper layers of the bowel wall, can cause duodenal stricture with attendant signs similar to those in foals with outflow obstruction. Pyloric stenosis, duodenal stricture, and gastric outflow obstruction are diagnosed occasionally in adult horses as a complication of severe inflammation involving the proximal portion of the small intestine. Hepatic duct stricture and pancreatic duct stricture have also been reported in association with duodenitis in adult horses.
Foals with enteritis or enterocolitis are chiefly predisposed to developing gastroduodenal ulcers because of dehydration and impairment of mucosal perfusion. Unsupervised or excessive administration of NSAIDs that might be given to manage colic or lethargy in an ill foal can add to the insult by inhibiting cyclooxygenase-1, the arm of the enzyme system that leads to production of prostaglandin E. Prostaglandin E not only maintains vasodilation and perfusion in the GI vasculature, it also directly suppresses HCl production by parietal cells. Decreased mucosal blood flow reduces integrity of the bicarbonate-rich mucus layer that lies in contact with the gastric mucosal cells and normally keeps the pH in the cells’ immediate environment at neutral values; if the hypoperfusion is unmitigated, diminution of the protective layer, back-diffusion of acid, and bacterial translocation occur. If the enteritis is severe enough to cause colic and disrupt nursing activity, the foal is additionally subject to longer periods of time when the stomach is empty of milk and its acid-buffering effects. Colic also leads to longer periods of recumbency, which increases exposure of the squamous epithelium to gastric acid. Infectious agents causing upper GI tract inflammation, such as rotavirus, may have direct effects on duodenal and pyloric enterocytes; spatial and temporal clustering of cases of GDUS on a farm or in a region support such a relationship. However, some foals develop duodenal ulcers without detectable rotaviral infection, and evidence for a relationship between rotavirus and duodenal ulcers remains circumstantial at present.
In the author’s practice area, affected foals very often have been treated with antiulcer medications, including H2 receptor blockers, proton pump inhibitors, and sucralfate, by the time they are presented with signs of gastric outflow obstruction. The apparent failure of a regimen of antiulcer medications to prevent development of severe ulcers in the upper GI tract may reflect an inability of even effective therapeutic agents to work when anatomic stricture restricts the normal removal of acidic contents from the gastric lumen or when illness alters normal blood flow to the gastric and duodenal mucosa. It is also possible that even when hydrochloric acid output is modulated, ulcerogenesis is still mediated by organic acids, such as lactic acid produced by Lactobacillus acidophilus and volatile fatty acids made by other fermentative organisms that can survive in the stomach. The contribution of these acid products to ulcer formation in foals is unknown, but in older foals being fed concentrate-rich diets to encourage growth, these acids may have the same deleterious effects as have been proposed in adult horses upon prolonged contact with the gastric mucosa, especially the squamous portion. Bile acids that enter the stomach in refluxing duodenal fluid are another organic acid that may be a vehicle of injury to gastric cells, although it has been proposed that these acids play a more direct role in causing esophagitis (upon reflux) than gastritis.