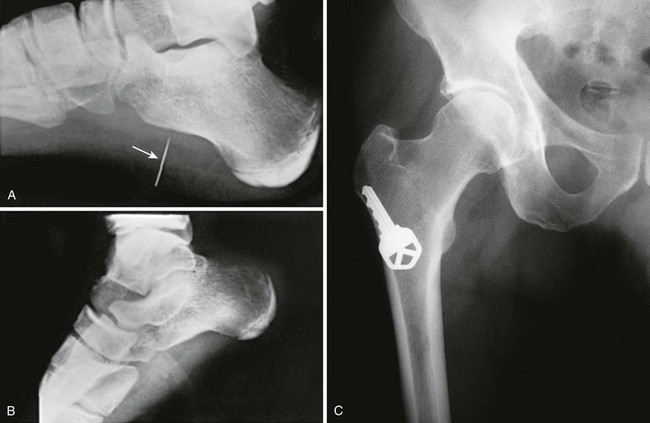
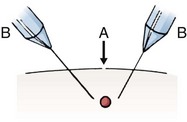
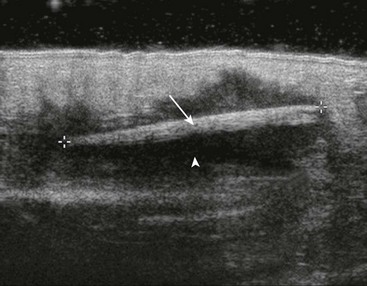
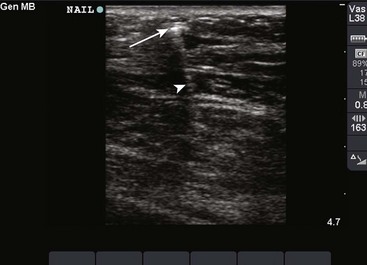
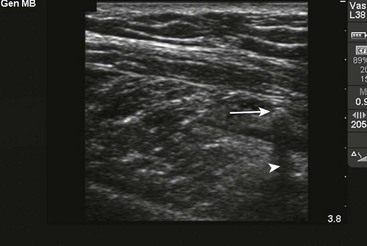
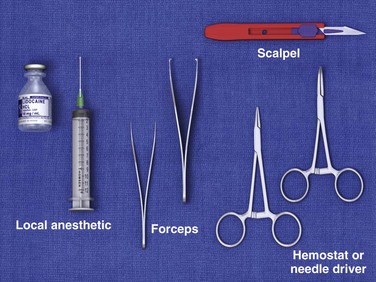
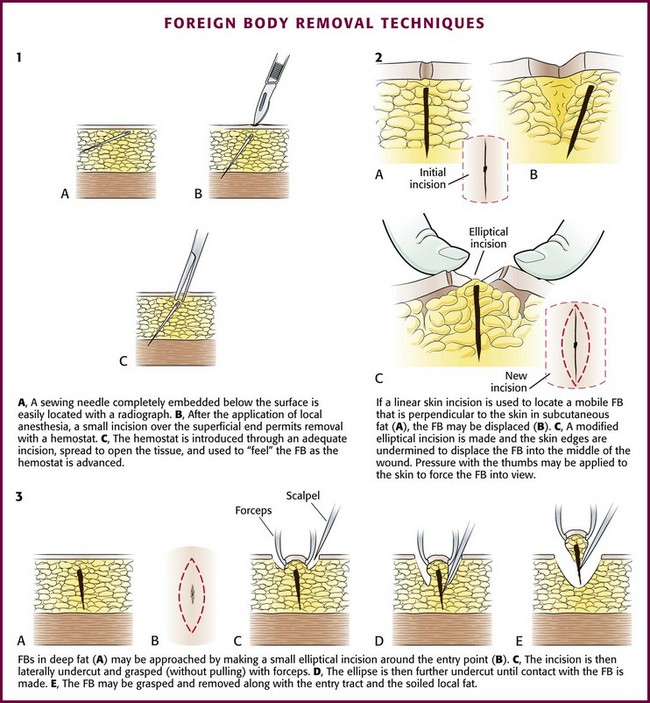
Chapter 36 A foreign body (FB) is any substance that is not naturally part of the body. These cases are common in the clinical setting. An FB should be suspected whenever the skin is broken. A thorough history and physical examination are essential to assess the risk for an FB. During assessment, remember that FBs may not be obvious and that the wound may appear closed, but they should be considered whenever the history is particularly concerning. For example, a patient who is walking without shoes and experiences a sharp, sudden pain in the foot may have a needle, toothpick, or any other similar type of FB, even when a “sprained foot” seems obvious (Fig. 36-1). Certain mechanisms of injury, such as punching or kicking out a window or stepping on an unknown object while walking in a field or stream, are associated with a retained FB. Mechanisms that make FBs less likely include lacerations from metal objects; however, if considerable force was applied during the injury and the object is not available for inspection, radiographic imaging may be warranted since bone may have been encountered and a small section might have splintered off the offending object. The history should also include asking whether the patient perceives or suspects an FB. Steele and associates found that the negative predictive value of patient perception was 89% but that the positive predictive value was just 31%.1 Importantly, the patient’s past medical history should be explored for allergies to local anesthetics, bleeding diatheses, diabetes mellitus, vascular disease, uremia, immunocompromised state, or other diseases that would affect wound healing or management. Exploration is an important part of the bedside evaluation, whether done initially or after further imaging studies (Fig. 36-2). This requires adequate pain control, good lighting, proper equipment, a bloodless field, a cooperative patient, and appropriate positioning to visualize as much of the wound as possible (Figs. 36-3 and 36-4). A metal probe may help identify the FB by feel or sound. Glass, as an example, is difficult to identify by sight in soft tissue, but touching it with metal causes a characteristic grating sound. Probing a wound with a gloved finger to locate or identify an FB is strongly discouraged because of the risk of the FB penetrating the glove and exposing the clinician to human immunodeficiency virus (HIV) and hepatitis (Fig. 36-5). Alternatively, some authors have suggested injecting the entrance wound with methylene blue to outline the track of the FB.2 The blue line of injected dye is followed into the deeper tissues. This technique is of limited value because the track of the FB often closes tightly and does not allow passage of the methylene blue. Figure 36-3 A, This patient has an obvious wooden foreign body on the dorsal aspect of the proximal part of the forearm. B, Manual removal of the object was not difficult. C, However, thorough exploration of the wound cavity via an incision over the entire length of the FB tract revealed multiple small wooden fragments. Proper exploration requires adequate analgesia, good lighting, hemostasis, and a cooperative patient. Use of a metal probe may help identify the foreign object by feel or sound (see Fig. 36-17). Many emergency clinicians mistakenly believe that in the absence of adipose tissue, if the base of the wound can be clearly visualized and explored, an FB can always be ruled out. Orlinsky and Bright found the reliability of exploration to be related to the depth of the wound.3 In their study, only 2 of 133 superficial wounds, deemed adequately explored, had an FB on plain films, but 10 of 130 wounds had FBs beyond the subcutaneous fat despite negative explorations. Anderson and coworkers reported that 37.5% of the foreign bodies were initially missed by the treating physicians.4 In many of these cases, a radiograph of the injured area was not taken. Avner and Baker detected glass with routine radiographs in 11 of 160 wounds (6.9%) that were inspected and believed by the clinician to be free of glass.5 Clinicians evaluating for FBs should maintain a low threshold for ordering or performing imaging studies. Options for imaging include plain radiographs, ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), and fluoroscopy. See Table 36-1 for a summary. TABLE 36-1 A reasonable initial approach for localizing nonvisualized FBs in the ED is to obtain multiple-projection plain radiographs with a soft tissue technique. This technique will visualize the majority of FBs, especially metal and glass. US should be considered for objects known to be radiolucent, such as wood or thorns. The role of CT and MRI for evaluation of FBs in the ED is limited, but they are the definitive imaging tests in confusing cases. For suspected intraorbital or intracranial FBs, CT is recommended. CT or MRI is also warranted when a previously negative explored wound exhibits recurrent infection, poor healing, or persistent pain. CT or MRI may be the appropriate initial test for patients with nonspecific swelling to define FBs and possible alternative diagnoses such as abscesses, masses, or other inflammatory processes.6 Bedside US and fluoroscopy (for radiopaque FBs) may be used to guide difficult FB extractions if initial attempts at removal are unsuccessful and the proper equipment and experienced personnel are available. Plain radiographs are readily available, are easily interpreted, and cost significantly less than CT, formal US, and MRI do.7 The ability of plain films to detect FBs in soft tissue depends on the object’s composition (relative density), configuration, size, and orientation (Fig. 36-6). Detection of FBs on plain films can be enhanced by requesting an underpenetrated soft tissue technique and by obtaining multiple views to prevent FBs from being obscured by superimposed bone or soft tissue folds.8 Plain films are often sufficient; however, digitized radiographs may be manipulated to enhance identification of a suspected FB. Indirect evidence of an FB may include trapped or surrounding air, a radiolucent filling defect, or secondary bony changes such as periosteal elevation, osteolytic or osteoblastic alterations, or pseudotumors of bone.8 Metallic objects are readily visualized on radiographs. Despite a common misconception that glass must contain lead to be visualized on a plain radiograph, almost all glass objects in soft tissue (bottles, windshield glass, lightbulbs, microscope cover slips, laboratory capillary tubes) are at least somewhat radiopaque and can be detected by plain radiographs unless they are obscured by bone or are very small (<1 mm) (Fig. 36-7).7,9,10 The absence of a glass FB on multiple projections is strong, though not absolute evidence that glass is not contained in a wound. Other nonmetallic objects readily visualized include teeth, bone, pencil graphite, asphalt, and gravel.7,11 Aluminum, which has traditionally been deemed radiolucent, can occasionally be visualized on plain films if the object is projected away from the underlying bone. Ellis demonstrated that pure aluminum fragments as small as 0.5 × 0.5 × 1 mm could be identified in a chicken wing model simulating a human hand or foot.12 Ellis cautioned that other aluminum FBs, such as pull tabs from cans, may not be visualized in other parts of the body such as the esophagus or stomach.12 Certain FBs such as vegetative material (thorns, wood, splinters, and cactus spines) are radiolucent and not readily visualized on plain radiographs. These materials absorb body fluids as they sit in situ and become isodense with the surrounding tissue. Because of their varying chemical composition and density, plastics may or may not be visible on plain films.13 Besides simply diagnosing FBs, radiographs can also be used to estimate the general location, depth, and structure of radiopaque FBs. If one strategically attaches a marker (needle or paper clip) to the skin surface at the wound entrance before taking a radiograph, the FB will be seen in relation to the entrance wound (Fig. 36-8). This also helps identify the path that leads to the FB and the relative distance from the surface to the FB.14 Needles at two angles may also be used to aid in localization (Fig. 36-9). Liberal use of plain film radiography makes sound medicolegal practice. A review of 54 wound FB claims against 32 physicians from 22 institutions found glass, a radiopaque substance, to be the most common material. However, in only 35% of the cases involving glass were plain films taken. Cases with a glass FB without a radiograph ordered were associated with unsuccessful defense (60%) and higher indemnity payments.15 US has become the modality of choice for imaging radiolucent FBs such as wood and thorns because most soft tissue FBs are hyperechoic on US. In addition, if in place for more than 24 hours, most FBs will be surrounded by a hypoechoic area corresponding to granulation tissue, edema, or hemorrhage, which may aid in making the diagnosis.16 Metal will leave a linear trail of echoes deep to the FB, referred to as the “comet tail artifact.” A wooden object leaves an acoustic shadow without artifact.17,18 US may be performed at the bedside. To do so, use a high-frequency transducer (at least 7.5 MHz, such as a high-frequency linear vascular probe) since most FBs are small and superficial. A lower frequency may also be necessary if a deeper FB is suspected, but it may miss small FBs.19 A spacer may be needed to adjust the “focal zone”—where the beam is the narrowest and signal intensity is the highest. US may be particularly difficult in the hand or foot, which have many echogenic structures and web spaces that may limit visualization when the FB is adjacent to bone.16,18,20 Keep in mind that the presence of air, scars, calcification, sutures, and sesamoid bones in surrounding tissue may lead to false-positive results.20,21 Advantages of US include low cost, no ionizing radiation, the ability to define the object in three dimensions, and real-time imaging, which may be used during removal.8 Many studies report that US is highly sensitive for the detection of FBs by adequately trained personnel, either radiologists, technicians, or emergency physicians.3 It is difficult to cite a precise sensitivity or specificity because of the wide variation in these studies with regard to FB size, material, and location; operator experience; and the models used in these studies.21–23 CT depends on x-ray absorption; thus, it generally visualizes the same material detected on plain films, but subtle differences in soft tissue densities may help identify FBs not seen on radiographs.7,11 Also, CT produces a better three-dimensional image than plain films do and may visualize objects embedded in or behind bone. However, CT is more costly and exposes the patient to more ionizing radiation than radiography or US does, and its use should therefore be judicious. As an example, wood is unlikely to be visible initially on CT, but after 1 week, the wood absorbs surrounding blood products and may become higher in attenuation than muscle and fat. It may then appear on CT as a linear area of increased attenuation on a wide window setting such as a bone window.6 Although MRI is expensive and not as readily available to emergency clinicians as plain films and CT are, it may be superior to CT in detecting small, nonmetallic, radiolucent FBs such as plastic, particularly in the orbit.24 MRI may not visualize wood, which may appear as a linear signal with associated inflammation and looks hypointense with respect to muscle on T1- and T2-weighted sequences, on which it appears as a signal void.6 Plastic is more easily visualized with MRI than with CT. MRI cannot be used for metallic objects and gravel, which contain various ferromagnetic particles that produce signal artifacts and a theoretical risk of shifting within the magnetic field and causing structural damage.7 This is particularly important when evaluating FBs in the eye, brain, or deep structures of the neck, face, or extremities. FBs may be difficult to differentiate from other low-signal structures on MRI, such as tendon, scar tissue, and calcium.25 More recently, portable, low-power, C-arm fluoroscopy has become available in some emergency departments (EDs), particularly for orthopedic reductions. Its use has also been reported for the removal of BB pellets, metal, glass, and coins from patients.26 Like radiography, fluoroscopy can visualize objects that are radiopaque but not radiolucent such as wood and plastic.26,27 By using correct technique and shielding, radiation scatter to imaging personnel is minute, less than 0.0001 R/hr.28 Fluoroscopy also offers the advantage of real-time bedside imaging.26,28 Fluoroscopic image-intensifying equipment may be used to follow a wound’s entrance, localize the material, grasp the FB, and remove it without making a larger incision. Ariyan described a technique in which two needles are placed in the soft tissue from opposite directions and pointing toward the FB.29 The extremity is rotated while the clinician watches the image under the image intensifier to obtain a three-dimensional effect. An incision is made perpendicular to the plane of the needles, and the object is removed. Although the technique to use fluoroscopy is relatively easy to learn, the lack of instruction and availability is the major limitation to its use in the ED.28–30 When reviewing the decision regarding when and how to remove the FB, the possibility of the FB migrating to involve vital structures, though quite remote, should be discussed with the patient. Cases of reported missile embolization in the vascular system are influenced by missile caliber, impact velocity, physical wound characteristics, point of vessel entrance, body position and movement, and velocity of blood flow.31 Retained bullets usually remain in soft tissue but can rarely make their way into the vascular system. Schurr and colleagues reported a paradoxical bullet embolization from the left external iliac vein to the left iliac artery via a patent foramen ovale.32 When clinicians first examined the patient, a bullet was noted on the chest radiograph, and an isolated chest wound was suspected. However, the bullet had apparently entered the chest, traversed the abdomen to the iliac vein, and then embolized back to the chest and arterial system. Good space and lighting, a comfortable patient and operator position, a standard suture tray, and a scalpel are usually adequate equipment for the removal of most simple FBs (Fig. 36-10). Tissue retractors, special pickups, and loupes may be added if needed. After obtaining appropriate informed consent and following sterile preparation, consider enlarging the entrance wound with an adequate skin incision, which can be advantageous. Numerous techniques are used, depending on the clinical scenario (Fig. 36-11). Attempting to remove an FB through a puncture wound or an inadequate skin incision is a common error that is both frustrating and self-defeating. After a proper skin incision, explore the wound carefully by spreading the soft tissue with a hemostat. Frequently, the FB can be felt with an instrument before it can be seen (see Fig. 36-11, plate 1). After placing a tourniquet on an extremity, follow the track of the FB, although it often cannot be identified when surrounded by muscle or fat. If the FB, such as one that is made of fiberglass or plastic, is difficult to visualize, is located in the superficial soft tissue, or has contaminated the surrounding soft tissue, excising a small block of tissue rather than removing the FB alone may be necessary. Excise the block of tissue only under direct vision and after nerves, tendons, and vessels have been identified and excluded from the excision area. If an FB such as a thorn or needle enters the skin perpendicularly, a linear incision may pass to one side or the other of the FB, and it may be difficult to determine where the FB lies in relation to this incision (see Fig. 36-11, plate 2). For this reason the search must then be extended into the walls of the incision rather than simply through the skin.33 In such cases, excise a small ellipse of skin and undermine the skin for 0.5 to 1.0 cm in all directions. Next, compress the tissue from the sides in the hope that the FB will extrude and can then be grasped with a hemostat. After removal of the FB, it is important to irrigate and cleanse the wounds. If a small incision has been made in a noncosmetic area (such as the bottom of the foot), leave the incision open and bandaged. The area may be periodically soaked in hot water for a few days. A return visit is necessary only if signs of infection develop. If a large incision has been made, the skin may be sutured primarily as long as no other contraindications are present. In cases in which gross contamination has occurred or there is significant tissue injury, do not close the wound on the initial visit. Leave the wound open but packed. Suture the skin after 3 to 5 days if the wound is free of inflammation or infection (known as delayed primary closure; see Chapters 34 and 35 for details). Puncture Wounds in the Sole of the Foot Puncture wounds in the feet from unknown objects and under unknown circumstances present problems to the clinician. In general, puncture wounds in the feet are at risk for retained FBs and infection. It is impossible to adequately explore a puncture wound. In noncosmetic areas, therefore, a puncture wound can be converted to a laceration to adequately explore and clean it (Fig. 36-12). Under most circumstances, delayed primary closure is recommended (see Chapter 34). This topic, including stepping on a nail and puncture wounds in the sole of the foot, are discussed extensively in Chapter 51.
Foreign Body Removal
Evaluation and Diagnosis

Augmenting the Physical Examination: Imaging Techniques
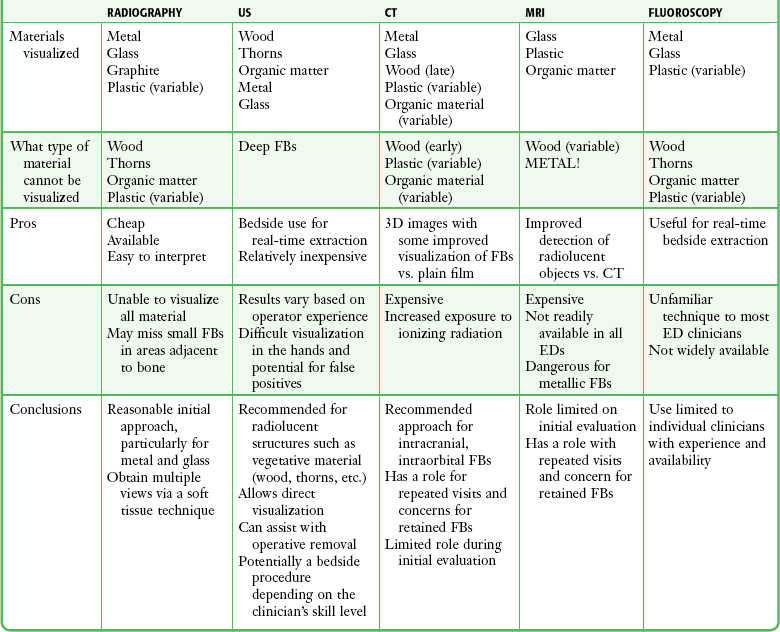
Plain Radiography
US
CT
MRI
Fluoroscopy
FB Removal
Equipment and Preparation
Operative Technique
Special Scenarios and Techniques
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Foreign Body Removal