Chapter 4 FELINE HYPERTHYROIDISM (THYROTOXICOSIS)
The thyroid gland was first described in detail by Vesalius in the sixteenth century. Thomas Wharton (1614-1673) named the gland from the Greek word thyreos, or shield, based on its physical appearance. One of the first described thyroid disorders was an association between iodine deficiency and enlargement of the thyroid (goiter), initially suspected in the 1500s to be a possible cause of cretinism. This description also represents the first mention of thyroid gland enlargement. Endemic cretinism in the region around Salzburg, Austria, was described by the Swiss-German physician Paracelsus (1493-1541).
Hyperthyroidism, caused by autonomous growth and function of the thyroid follicular cells, was initially described in humans by Henry Plummer in 1913. Clinical observations led him to characterize two types of hyperthyroidism: exophthalmic goiter (Graves’ disease) and toxic adenomatous goiter. In Graves’ disease, the hyperthyroidism appeared to be associated with diffuse hyperplasia of the thyroid glands. Toxic adenomatous goiter was associated with either single or multiple nodules and variable histologic patterns. The latter disease involved the slow growth of autonomous functioning follicles. Interestingly, toxic nodule syndrome (toxic adenomatous goiter) is believed to be most similar (homologous) to the disorder seen in most hyperthyroid cats, initially described as a clinical entity in 1979 by Peterson and in 1980 by Holzworth and colleagues.
DEFINITION
Naturally occurring hyperthyroidism (thyrotoxicosis) is a clinical condition that results from excessive production and secretion (and, subsequently, circulating concentrations) of thyroxine (T4) and triiodothyronine (T3) by the thyroid gland. Hyperthyroidism in cats is almost always the result of a primary autonomous condition (i.e., it arises independent of a hypothalamic or pituitary abnormality). Rarely, hyperthyroidism in people may be caused by a hypothalamic or pituitary disorder (Brucker-Davis, 1999). Theoretically, hyperthyroidism may also result from acute destruction of thyroid tissue, causing excessive release of thyroid hormone. Syndromes involving the hypothalamus, the pituitary, or thyroid destruction have not been described in cats. Hyperthyroidism in cats, therefore, is most often due to an intrinsic disease within one or both thyroid lobes.
HISTORY OF HYPERTHYROIDISM
Veterinary clinicians were not aware of feline hyperthyroidism until two clinical reports were published (Peterson et al, 1979; Holzworth et al, 1980). With this information, practitioners began to recognize cats with signs suggestive of hyperthyroidism (thyrotoxicosis). Cats with clinical hyperthyroidism were not recognized at the University of California prior to 1980. Within a 5-year period after the studies published in 1979 and 1980 (1980 through 1985), 125 hyperthyroid cats with clinical disease were identified at our hospital. During a similar period, cats with the disease were being recognized at a rate of three per month at the Animal Medical Center in New York City (Peterson et al, 1983). In a 1993 survey conducted at the Animal Medical Center, approximately 22 cats with hyperthyroidism were recognized each month (Broussard et al, 1995; Peterson, 1995a and 2000). It is not clear whether the incidence of the condition continues to escalate, but there is no doubt that feline hyperthyroidism is now commonly recognized in Great Britain, Europe, and Japan, as well as throughout the United States.
PATHOLOGY
Benign Thyroid Tumors
MULTINODULAR ADENOMATOUS GOITER.
In the 1976 review by Leav and colleagues, multinodular adenomatous tumors were not often associated with enlargement of the thyroid, but experience since then demonstrates that most hyperthyroid cats have a palpably enlarged gland. Multinodular adenomatous goiter is the most common histologically described thyroid lesion in thyrotoxic cats (Carpenter et al, 1987). Similarly affected cats have had thyroid tissue classified as adenomatous hyperplasia, and still others have been described as having adenomas. It will be interesting to learn whether all three conditions are the same and simply identified by a different set of “terms,” or whether the three conditions (multinodular adenomatous tumors, adenomatous hyperplasia, and adenoma) are somehow distinct. It would appear that most cats (approximately 70% to 75%) have this “benign” adenomatous condition involving both thyroid lobes.
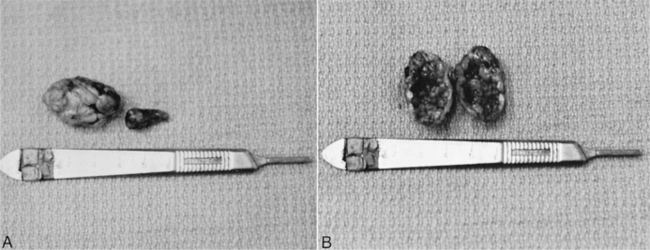
In affected thyroids, multifocal nodules are dispersed throughout the gland. The foci of hyperplastic tissue form nodules that range from less than 1 mm to greater than 3 cm in diameter (Peterson, 2000). The thyroid may have the appearance of a compressed cluster of grapes (Fig. 4-1). Most are solid, but a small percentage may be cystic or “cavitary” and filled with fluid (see Fig. 4-1). The lesions are histologically similar to nodular hyperplasia or multiple adenomatous goiter of humans. The foci are composed of irregularly arranged, colloid-filled follicles that are quite different from normal tissue. Occasionally the surrounding parenchyma is compressed, and in a few cases microfollicular or compact cellular patterns may be observed. Colloid-filled cysts are frequently found adjacent to nodules. The follicular cells are uniform and cuboidal in shape.
ETIOLOGY
Historical Background
INCIDENCE.
There is little doubt that the incidence of hyperthyroidism in cats steadily increased from the time the first reports describing this condition in 1979 and 1980 were published until the early to mid-1990s. Whether the incidence continues to expand is not yet known. Regardless, it is fair to question whether the current “common” status of this condition is due to increased awareness of owners, the diagnostic acuity of veterinarians, the longer life span and increased popularity of cats as pets, or a true increasing incidence of the disease. It is likely that all these explanations have merit, because it is now estimated that the disorder affects as many as 1 in 300 cats (Gerber et al, 1994).
Possible Nutritional and Environmental Causes
GOITROGENS.
Although most commercial cat foods contain relatively large amounts of iodine, studies have failed to demonstrate a correlation between dietary iodine and feline hyperthyroidism. Commercial cat foods and the environment contain a variety of other goitrogens (ingredients that might cause thyroid enlargement or hyperthyroidism, or both), including phthalates, resorcinol, polyphenols, and polychlorinated biphenyls. Most of these hydrocarbons are metabolized via glucuronidation, a process that is unusually slow in cats (Court and Greenblatt, 2000).
SOYBEANS.
Inadvertent inclusion of goitrogenic compounds in diets is plausible. Soybean is a potential dietary goitrogen that is used as a source of high-quality vegetable protein in commercial cat food. Soy isoflavones genistein and daidzein have been implicated due to their inhibitory effect on thyroid peroxidase, an enzyme essential to thyroid hormone synthesis (Divi et al, 1997). Glucuronidation appears to be an important pathway for eliminating soy isoflavones via the liver, a process that is deficient in feline liver. These compounds, therefore, could play an etiologic role in feline thyrotoxicosis. Genistein and daidzein are common constituents of commercial cat foods, and soy isoflavones have been detected in amounts predicted to have a biologic effect (Court and Freeman, 2002). Further research on this subject is anticipated.
EPIDEMIOLOGY.
An early epidemiologic study suggested that feeding of canned cat foods, living strictly indoors, being a non-Siamese breed, and having reported exposure to flea sprays, fertilizers, insecticides, and herbicides increased the risk of developing hyperthyroidism (Scarlett et al, 1988). In another study, two genetically related cat breeds (Siamese and Himalayan) were found to have a diminished risk of developing hyperthyroidism. In addition, there was a twofold to threefold increase in risk of developing hyperthyroidism among cats fed mostly canned cat food. There was also a threefold increase in risk among cats using cat litter (Kass et al, 1999). In a more recent study, there was no breed association with risk for developing hyperthyroidism. Exposure to fertilizers, herbicides, plant pesticides, or flea control products or the presence of a smoker in the home were not significantly associated with an increased risk for developing hyperthyroidism. Cats that preferred fish-flavored or liver and giblets–flavored canned cat food had an increased risk of hyperthyroidism (Martin et al, 2000).
SELENIUM.
The thyroid gland contains more selenium per gram of weight than any other tissue, which suggests an important role for this trace element in homeostasis. Selenium exerts its biologic activity through the expression of selenoproteins, including glutathione peroxidases and thioredoxin reductase, which protect thyrocytes from oxidative damage. Because selenium is also a growth factor, this dietary element may play a role in development of toxic nodular goiter in cats. Cats were studied from two geographic areas with an allegedly high incidence of hyperthyroidism and two regions with a lower incidence. It was found that cats have higher concentrations of selenium in the plasma than do other species but that this does not appear to affect the incidence of hyperthyroidism. However, the authors concluded that high selenium concentrations may affect feline health if they are influenced by the amount included in diets (Foster et al, 2001).
Possible Autocrine or Paracrine Growth Factors
GENERAL.
Growth factors, or peptides that stimulate cell proliferation, may have a role in normal growth and in carcinogenesis. Autocrine activity defines a cell reacting to a growth factor that it produces itself. Paracrine activity defines a cell reacting to growth factors produced by neighboring cells. Cells generally require multiple growth factors for optimal response. Several growth factors have been identified in thyroid cells, including platelet-derived factors, epidermal growth factors, and the insulin-like growth factors. It remains to be determined whether any of these families of growth factors contribute to the development of feline hyperthyroidism (Brown et al, 1992).
G PROTEINS.
The synthesis and secretion of thyroid hormone are regulated by thyroid-stimulating hormone (TSH). TSH binds to a receptor (TSH-R) on the surface of thyroid cells. The receptors are bound to specific proteins that are members of a “superfamily” known as G proteins. Binding of TSH to the TSH-R stimulates growth and differentiation of thyroid cells via a G protein–mediated cyclic adenosine monophosphate (cAMP)-dependent signal transduction pathway. Alterations in the expression of G proteins could be involved in the pathogenesis of feline hyperthyroidism. In an in vitro study of thyroid adenomas obtained from hyperthyroid cats, a decreased amount of one G protein was identified (Hammer et al, 2000). When present, this G protein may inhibit growth and differentiation of thyroid cells. Decreased expression of this G protein from adenomatous thyroid glands, therefore, may reduce the inhibitory effect on the cAMP cascade in thyroid cells, leading to autonomous growth and hypersecretion of thyroxine. An understanding of the molecular mechanisms of hyperthyroidism in cats may lead to better treatment or ultimately to prevention of the disease (Hammer et al, 2000).
Circulating Thyroid Stimulators or Genetic Mutations
Although as yet not demonstrated, it is possible that hyperthyroidism in cats is caused by circulating factors similar to the immunoglobulins that bind to TSH receptors and stimulate thyroid hormone secretion, resulting in Graves’ disease in people (Peterson et al, 1987b). Studies directed at finding mutations in the TSH receptor gene have failed to identify such abnormalities (Pearce et al, 1997). The structure of the feline TSH receptor is similar to that of the human TSH receptor. Serum from humans with Graves’ hyperthyroidism, but not serum from cats with hyperthyroidism, activates feline TSH receptors (Nguyen et al, 2002). However, future studies may yet elucidate “gain in function” mutations or circulating immunoglobulins that play a role in the development of this disease.
CLINICAL FEATURES
Signalment
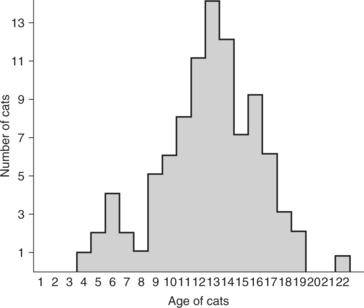
Hyperthyroidism is probably the most common endocrinopathy affecting cats older than 8 years of age. The reported age range is 4 to 22 years, with a mean just under 13 years. A small number of cats younger than 4 years have been diagnosed with hyperthyroidism, although the disorder remains quite uncommon in this age group (Gordon et al, 2003). Fewer than 5% of cats diagnosed with hyperthyroidism are younger than 8 years of age (Fig. 4-2). There has been no breed or gender predilection, although the Siamese and Himalayan, as previously noted, may have a decreased risk of developing hyperthyroidism (Thoday and Mooney, 1992a; Broussard et al, 1995; Peterson, 1995a).
Signs and Their Physiopathology
HUMANS.
Interestingly, the most common clinical signs diagnosed in elderly people (>70 years of age) with hyperthyroidism are quite similar to those observed in hyperthyroid cats: weight loss, thinness, atrial fibrillation, agitation, anxiousness, and muscle weakness and tremor. Less frequent findings (fewer than 50% of humans) have included heat intolerance, confusion, apathy, and diarrhea (Martin et al, 1996). However, another report suggests that the diagnosis of hyperthyroidism in elderly people is a greater challenge than in younger people because the clinical manifestations may be more subtle and often suggest a single-organ condition (Maugeri et al, 1996). Subclinical hyperthyroidism is well documented in humans; it may be defined as abnormal test results in a person without clinical signs or as a condition of subtle clinical signs but normal serum T3 and T4 concentrations (Toft, 2001). Subclinical hyperthyroidism may be diagnosed in about 1% of people over the age of 60. It is not clear whether a comparable condition exists in cats. Most hyperthyroid cats have a variety of clinical signs that reflect multiple organ dysfunction, although some have one clinical sign that predominates (Mooney, 1998a and 1998b).
General overview: factors affecting clinical signs
DELAYED OWNER CONCERN.
Signs of hyperthyroidism are insidiously progressive, which often delays owner recognition of a problem and therefore may allow the disease to progress before veterinary attention is considered. More than half of our hyperthyroid cats had clinical signs for longer than 6 months to 1 year before the owners sought veterinary assistance. The primary reason for this delay in owner action is the sequence of the development of clinical signs. Hyperthyroid cats initially maintain good (sometimes ravenous) appetites and are active (if not overactive) pets. These changes are usually interpreted as evidence of health, not disease. More worrisome signs also begin slowly, are seen infrequently, or remain subtle for prolonged periods (Table 4-1). The owner, therefore, typically observes a pet that “appears healthy” during the initial phases of hyperthyroidism. It is not until weight loss is severe or some of the other, more worrisome clinical signs become frequent or more obvious that an owner realizes his or her cat may be ill. One common owner misconception, once the signs are appreciated, is that the cat is simply “aging” and these changes are to be expected. Sometimes it is only when the signs become intolerable that professional advice is sought. The most common reasons for owners to seek veterinary help are cats with obvious weight loss, polyphagia, polydipsia/polyuria, vomiting, and/or diarrhea.
TABLE 4-1 OWNER OBSERVATIONS (HISTORICAL SIGNS) OF CATS WITH HYPERTHYROIDISM
| Sign | Percent of Cats |
|---|---|
| Weight loss | 92 |
| Polyphagia | 61 |
| Polydipsia/polyuria | 47 |
| Increased activity/restless | 40 |
| Gastrointestinal (diarrhea, increased frequency, increased volume, steatorrhea) | 39 |
| Vomiting | 38 |
| Skin changes (patchy alopecia, matting, dry coat, greasy seborrhea, thin skin) | 36 |
| Respiratory signs (dyspnea, panting, coughing, sneezing) | 23 |
| Decreased appetite/anorexia | 14 |
| Decreased activity/lethargy | 11 |
| Weakness | 10 |
| Tremor/seizures | 7 |
| Seeks cool areas/heat intolerance | 5 |
| Hematuria | 2 |
| Ventroflexion of neck | <1 |
INCREASED VETERINARIAN AWARENESS.
Assays of the serum thyroxine concentration are now a routine component of feline serum biochemistry profiles, which helps clinicians recognize hyperthyroidism before signs become severe. As a result, cats with hyperthyroidism are being diagnosed earlier in the course of the disease, and therefore the clinical signs observed by owners and veterinarians may not be as obvious, severe, or frequent as those described in the 1980s (Broussard et al, 1995; Kintzer, 1995; Mooney, 1998a; Bucknell, 2000) (see Table 4-1). These factors do not diminish the importance of a thorough history and physical examination. On the contrary, these parameters gain value as the clinician attempts to diagnose a condition before serious complications develop.
Weight loss and polyphagia
SIGN.
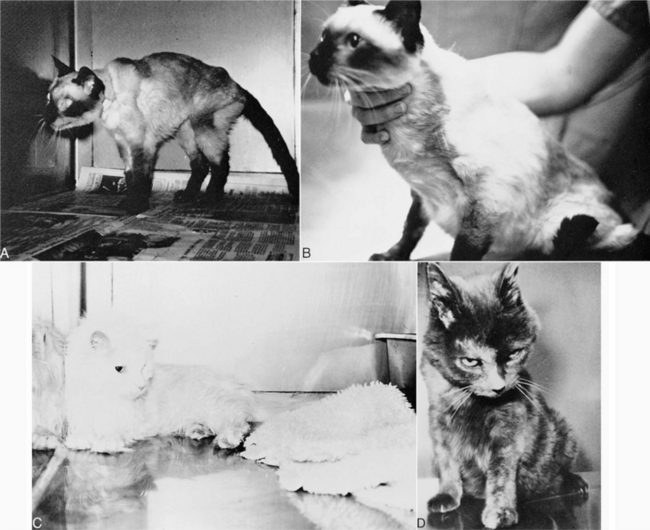
Weight loss and polyphagia are extremely common signs in cats with hyperthyroidism. Approximately 90% of hyperthyroid cats have some weight loss, according to their owners. The weight loss described by owners may be mild to severe, and a small percentage of hyperthyroid cats are severely cachectic (Fig. 4-3). The weight loss typically occurs gradually over a period of months. Owners may comment that the weight loss was not recognized until someone who had not seen the cat for several months noticed the change. It has been suggested that weight loss is usually evident if greater than 10% of body weight has been lost and is often described as emaciation if greater than 20% has been lost (Mooney, 1998b).
An increase in appetite may occur with a variety of disorders. This is an extremely important historical finding, because the combination of polyphagia and weight loss has fewer differential diagnoses than anorexia and weight loss (Mooney, 1998b; Table 4-2). Cats previously thought to be finicky eaters may develop excellent appetites, a change that may not be perceived as a problem by the owner. Other cats are described as “always hungry.” They eat rapidly and then proceed to eat food put out for other household pets. One of our owners resorted to feeding her German Shepherd dog and hyperthyroid cat in separate rooms to avoid having the cat attack the dog for its food. Owners have described previously lazy or docile cats that had to be locked outdoors while the owners ate to avoid having the animal leap on the table and attempt to steal food.
TABLE 4-2 THE DIFFERENTIAL DIAGNOSIS FOR CATS WITH POLYPHAGIA AND WEIGHT LOSS
EXPLANATION.
A major consequence of hyperthyroidism is increased energy expenditure. Physiologic functions and mechanical work are accomplished with reduced efficiency. To counterbalance these changes, increased food intake, utilization of stored energy, and increased oxygen consumption occur. Despite this increased food intake, however, the state of chronic caloric and nutritional inadequacy persists. In humans, both the synthesis and degradation of proteins are increased, the latter to a relatively greater extent than the former, with the result that there is net degradation of tissue protein. The negative nitrogen balance is evidenced by loss of weight, muscle wasting, weakness, and mild hypoalbuminemia. The exact mechanism for the increase in appetite is not known. Approximately 6% of hyperthyroid cats exhibit periods of decreased appetite (see Decreased Appetite [Apathetic Hyperthyroidism], page 160).
Polydipsia and/or polyuria (PD/PU)
SIGN.
As with any sign associated with feline hyperthyroidism, remarkable variation in severity is common. Alterations in the amount of water consumed or urine excreted are highly variable. Although greater than 50% of owners did not notice changes in water intake or urine output (a smaller percentage than in the 1980s), others still report dramatic increases (Broussard et al, 1995). When present, these abnormalities can be quite striking and are an important diagnostic clue for the veterinary clinician. There are myriad causes of weight loss, but only a short list of diseases that result in significant polydipsia and polyuria.
EXPLANATION.
Renal blood flow, the glomerular filtration rate (GFR), and renal tubular resorptive and/or secretory capacities are increased in hyperthyroidism (Peterson and Randolph, 1989; Mackovic-Basic and Kleeman, 1991). No specific renal pathology is attributed to hyperthyroidism, although azotemia is common among these cats. Renal failure represents one cause of PD/PU. However, increases in renal blood flow secondary to hyperthyroidism may delay the clinical and biochemical consequences of renal failure in cats with both thyroid and renal disease (see In-Hospital Diagnostic Evaluation, BUN, and Creatinine, page 166) (Peterson, 1995a). After resolution of hyperthyroidism, regardless of the treatment method, renal perfusion may acutely decrease in some cats, “unmasking” their existing renal failure.
Many hyperthyroid cats have signs of PD/PU without evidence of renal disease. Failure to concentrate urine in these cats is probably due to an increased renal medullary blood flow and resultant decline in the medullary solute concentration gradient (Spaulding and Utiger, 1981). Studies of water balance in thyrotoxic humans usually revealed impaired concentrating ability after water had been restricted to the point of clinical dehydration. Some people have decreases in serum osmolality, indicating a possible primary thirst disorder. Given these individuals’ sensitivity to heat, plus the physical and personality lability seen in hyperthyroidism, primary (psychogenic) polydipsia is possible.
Nervousness, hyperactivity, aggressive behavior, and tremor
SIGNS.
Increased circulating concentrations of thyroid hormone may cause hyperkinetic behavior and agitation, presumably by a direct effect on the nervous system. This is true in people as well as cats. In a recent study on hyperthyroid people, 76% had tremor and 38% had generalized hyperreflexia (Duyff et al, 2000). The “nervousness” of the thyrotoxic cat is characterized by restlessness, irritability, and/or aggressive behavior (see Table 4-1). Many hyperthyroid cats appear to have an intense desire to move about constantly. A smaller percentage have been observed on occasion to “shiver” or have “tremors.” Surprisingly, this behavior is not apparent to many owners, even with careful questioning. Owners may note that their cats wander, pace, sleep for only brief periods, and waken easily. Although rare, focal or generalized seizures have also been described (Joseph and Peterson, 1993). To experienced veterinarians, many hyperthyroid cats appear “anxious.” They often cannot be held for the short time required to complete a physical examination. Some become aggressive if an attempt is made to further restrain them (Joseph and Peterson, 1993).
EXPLANATION.
Emotional lability is a prominent symptom of the thyrotoxic human. These people lose their tempers easily, and hyperkinesia is common. Such patients cannot sit still; they drum their fingers on the table, tap their feet, or shift position frequently. Movements are quick, jerky, exaggerated, and often purposeless (Utiger, 1987). Signs referable to the nervous system may reflect increased adrenergic activity, because some improvement occurs during treatment with adrenergic antagonists. Although the cerebral blood flow of thyrotoxic patients is increased, arteriovenous oxygen difference is diminished and oxygen extraction is unchanged. This correlates well with failure of thyroxine to increase oxygen consumption by brain tissue.
Diarrhea, vomiting, and bulky stool
SIGN.
The most common signs referable to the gastrointestinal tract are polyphagia and weight loss. Stools may be soft and bulky (increased volume) and may be foul smelling. The frequency of defecation may be increased. Vomiting is relatively common, occurring in about 40% of hyperthyroid cats. Anorexia and watery diarrhea are less common but when present are usually seen in cats with severe hyperthyroidism or in those with coexistent primary intestinal problems. Abdominal pain has been noted in some thyrotoxic humans but has not been appreciated in cats. As with many of the signs attributed to hyperthyroidism, those associated with the gastrointestinal tract are noted less frequently than in the 1980s (Broussard et al, 1995). Their significance, however, is just as important.
EXPLANATION.
Vomiting may result from direct action of thyroid hormone on the chemoreceptor trigger zone. Hyperthyroid cats that rapidly eat or overeat, or both, may vomit as a result of acute gastric distention. Vomiting is more common in hyperthyroid cats from multicat households, an environment that may contribute to rapid eating. One of the major gastrointestinal abnormalities is hypermotility with rapid gastric emptying and shortened small and large bowel transit times (Papasouliotis et al, 1993; Schlesinger et al, 1993). These disturbances contribute to both the increased frequency of defecation and the diarrhea.
Hair loss/unkempt coat
SIGNS.
Although an infrequent owner concern, hair coat changes (patchy alopecia, matted hair, lack of grooming behavior that may lead to matting or a seborrheic appearance, excessive grooming behavior with resulting alopecia) are found in a significant number of hyperthyroid cats. Problems of this nature have been identified in almost 40% of hyperthyroid cats (see Table 4-1). Like many signs associated with this disease, these problems are identified less frequently than a few years ago, with some investigators noting a dramatic decrease in incidence (from 50% in 1983 down to 9% in 1993) (Peterson, 1995a; Broussard et al, 1995). Typical bilaterally symmetric, nonpruritic “endocrine” alopecia is not often seen. Many cats have an unkempt, ungroomed hair coat. Some owners have reported seeing their cats pulling out hair in clumps, an unusual sign. Pulling out of hair may be a result of the heat intolerance seen in some cats. Heat intolerance is a classic sign of thyrotoxicosis in humans.
EXPLANATION.
In humans with thyrotoxicosis, skin changes are caused by increased protein synthesis, vasodilation, and increased generation of heat. The heat causes a warm, moist feel to the skin, which results from the vasodilation occurring secondary to the hyperdynamic circulatory state. Thin, fine hair, sometimes with areas of alopecia, are typical of thyrotoxicosis in humans. Warm skin, which is typ-ical of thyrotoxicosis, may be appreciated in the alopecic areas of cats (see Heat and Stress Intolerance, page 161).
Panting and respiratory distress
SIGN.
Open-mouth breathing (panting) is rare in cats and is often associated with significant hyperthermia, congestive heart failure, respiratory disease, pleural effusion, pulmonary edema, or hyperthyroidism. Slightly more than 10% of hyperthyroid cats exhibit panting, dyspnea, or hyperventilation periodically at rest. Respiratory signs are more common (>20% of cats; see Table 4-1) with the stress of traveling, restraint, playing briefly with another cat or, potentially, heart failure.
EXPLANATION.
Abnormalities in respiratory function described in humans with hyperthyroidism include decreased vital capacity, decreased pulmonary compliance, and increased minute ventilation (Ingbar, 1991). These changes are due to a combination of respiratory muscle weakness and increased carbon dioxide (CO2) production. The alveolar and arterial partial pressures of oxygen (PO2) and of carbon dioxide (PCO2) are usually normal. Ventilatory responses to hypoxemia or hypercapnia are increased. Respiratory muscle weakness has been described in a hyperthyroid cat with hypokalemia, which again supports the recommendation that serum potassium concentrations be monitored in ill hyperthyroid cats (Nemzek et al, 1994).
Decreased appetite (apathetic hyperthyroidism)
SIGN.
Although contradictory to the previously mentioned polyphagia, some hyperthyroid cats (about 14%) have been brought to veterinarians because of a diminished appetite (see Table 4-1). Some cats are polyphagic for months before progressing to inappetence or complete anorexia. This deterioration may correspond with the development of severe weight loss, muscle wasting, and weakness. The diminished appetite, therefore, is simply one component of progressive deterioration. Some cats have periods of polyphagia that alternate with periods of inappetence.
EXPLANATION.
Humans with thyrotoxicosis uncommonly develop poor appetites or anorexia. There is a clinical form of human thyrotoxicosis called apathetic hyperthyroidism in which the typical hyperthyroid symptoms are replaced by apathy or extreme depression (Peake, 1986). These people are usually extremely ill, and their weight loss is associated with anorexia. Their condition is due in part to psychological disturbances associated with thyrotoxicosis. Severe cardiovascular disease may also be a common component of this syndrome. Thyrotoxic-induced thiamine deficiency may contribute to depression and anorexia (see Physical Examination, page 161).
Cats with a decreased appetite and profound weakness may have cardiac abnormalities that include arrhythmias or congestive heart failure. However, some other concurrent, severe, nonthyroidal illness may also be a complicating factor. It has been suggested that almost all cats with apathetic hyperthyroidism suffer from renal failure, cardiac disease, or neoplasia (Peterson, 2000). As discussed previously, a small number of these cats have pronounced ventroflexion of the head and neck, a condition that may result from thiamine deficiency, hypokalemia, or simply severe muscle weakness (Fig. 4-3, D) (Mooney, 1998a).
Weakness and lethargy
SIGN.
Decreased activity, weakness, fatigability, and lethargy are variable findings in hyperthyroid cats, occurring in fewer than 15% of cats (see Table 4-1). Some cats are overactive and restless for 6 to 18 months before progressing to listlessness and weakness. With a few hyperthyroid cats, the first problem the owner notices is apparent weakness. Some chronically hyperthyroid cats have episodes of ataxia, whereas others can no longer jump as well or as high. A few cats develop severe cachexia and obvious weakness, requiring hand feeding and, in rare cases, tube feeding.
Weakness and fatigability are frequent complaints in humans with thyrotoxicosis. In a recent study, 67% of hyperthyroid people had complaints of muscle weakness, mainly in the proximal muscles of the legs, and 19% had symmetric distal sensory abnormalities and depressed distal tendon reflexes (Duyff et al, 2000). These patients often want to be active but are hampered by fatigue. They are often tired from “the neck down, rather than from the top of the head down.” In most instances this weakness is not accompanied by objective evidence of local disease in the muscles, save for the generalized wasting seen with weight loss. In the extreme, these individuals may be unable to rise from a sitting or lying position and may be unable to walk.
EXPLANATION.
The biochemical basis of the muscular weakness is uncertain, but the condition may simply be caused by weight loss and the catabolic state. Some hyperthyroid cats may be weak secondary to hypokalemia. Monitoring of serum potassium concentrations in weak hyperthyroid cats is strongly encouraged so that appropriate treatment can be instituted (Nemzek et al, 1994). Muscle weakness may also be related to the impaired ability of muscles in hyperthyroid individuals to phosphorylate creatine. On muscle biopsy, little if any inflammatory change is evident, but atrophy and infiltration by fat cells and lymphocytes have been reported. Electromyography reveals a decreased duration of mean action potentials and an increased percentage of polyphasic potentials. Thiamine deficiency may also explain the muscle weakness seen in some hyperthyroid cats.
Heat and stress intolerance
SIGN.
Heat intolerance is a mild sign but one that may be obvious to some cat owners. The normal cat seems to seek a sunny spot on the floor to sleep, sleeps nestled against a heating register, curls itself within feet of a roaring fire, or lies on the hood of a car that is still warm from use. Cats that reverse heat-seeking behavior and are found sleeping in the bath tub or on cool tile floors are quickly noticed (Fig. 4-3, C). Although such behavior is observed in only 5% of hyperthyroid cats (see Table 4-1), some owners have claimed that their cats had always sought out cool areas.
PHYSICAL EXAMINATION
General
Many of the signs described by an owner are also obvious to the veterinarian. Some changes may be more obvious or worrisome to the owner than to the veterinarian (e.g., weight loss, patchy alopecia/unkempt hair coat; see Table 4-1), and others may be more obvious to the veterinarian (e.g., hyperactivity). Additional abnormalities may also be detected during a thorough physical examination. Some of these changes become obvious with experience, whereas others remain subtle (Table 4-3).
TABLE 4-3 PHYSICAL EXAMINATION FINDINGS ASSOCIATED WITH HYPERTHYROIDISM IN CATS
| Finding | Percent of Cats |
|---|---|
| Palpable thyroid | 91 |
| Thin | 71 |
| Tachycardia (>240 beats/min) | 48 |
| Hyperactive/difficult to examine | 48 |
| Heart murmur | 41 |
| Skin changes (patchy alopecia, matting, dry coat, greasy seborrhea, thin skin) | 36 |
| Small kidneys | 26 |
| Increased rectal temperature | 14 |
| Gallop cardiac rhythm | 12 |
| Easily stressed | 12 |
| Dehydrated/cachectic appearance | 11 |
| Aggressive behavior | 8 |
| Premature cardiac beats | 8 |
| Increase nail growth | 2 |
| Depressed/weak | 2 |
| Ventroflexion of the neck | <1 |
Palpable Cervical Mass (Goiter)
NORMAL VERSUS HYPERTHYROID CATS.
In healthy cats, the thyroid lobes are positioned just below the cricoid cartilage and extend ventrally over the first few tracheal rings; they lie dorsolateral to and on either side of the trachea. The thyroid lobes are not palpable in normal cats. Hyperthyroidism is invariably associated with enlargement of one or both thyroid lobes (goiter), an enlargement that is palpable in about 90% of hyperthyroid cats. Palpation of a cervical mass is not pathognomonic for hyperthyroidism, however, because some cats with palpable thyroids are clinically normal and because some cervical masses are not the thyroids. Nonetheless, because many clinically normal cats with thyroid gland enlargement eventually develop clinical hyperthyroidism, frequent monitoring of these cats is warranted (Graves and Peterson, 1990; 1992).
PALPATION TECHNIQUE.
For the evaluation, the cat’s head should be gently extended. The thumb and index finger of one hand are gently placed on either side of the trachea in the jugular furrows at the thoracic inlet. The area is gently compressed, and the fingers are smoothly slid up to the larynx and back down again to the thoracic inlet. The fingertips should remain within the jugular furrows. Thyroid enlargement is usually felt as a somewhat movable, subcutaneous nodule approximately one half the size of the popliteal lymph node. Thyroid size in most hyperthyroid cats varies from the size of a lentil to the size of a lima bean. Occasion-ally, extremely large masses may be detected, such as one reported to be 4 × 7 × 10 cm), but masses this large are rare (Hofmeister et al, 2001). Thyroid tissue, if present and enlarged, “slips” under the fingertips.
In many instances we have been able to have owners visualize a goiter by having them watch the neck of their cat after we have moistened the area with alcohol, as our fingers slide toward the thoracic inlet, causing the enlarged thyroid to “pop up.” Success in this maneuver depends on not squeezing too hard; the pressure exerted must be gentle enough to allow the abnormal nodule to slide under the fingertips but firm enough to detect the mass. Also, for demonstration purposes, the ventrocervical area can be clipped free of hair and moistened. Occasionally this process allows easy visualization of a cervical mass (Fig. 4-4). Palpation of the neck is performed with greater confidence once a goiter can be seen.
Cardiac Disturbances
TACHYCARDIA, MURMURS, PREMATURE BEATS, AND GALLOP RHYTHM.
Because thin cats have relatively easily heard (loud) heart sounds, the clinician may develop a suspicion of heart disease. Furthermore, tachycardia in cats is a common finding, especially since veterinarians tend to compare the heart rates of cats with those of dogs. Heart rates greater than 240 beats per minute are typical of nervous cats, hyperthyroid cats, and some primary heart diseases. In addition, premature cardiac contractions associated with pulse deficits, gallop rhythms, murmurs, and pleural effusion (causing muffled heart sounds) are suggestive of primary heart disease, but these must also be considered consistent with thyrotoxicosis. Premature contractions are likely the result of myocardial irritation due to poor oxygenation, whereas murmurs may be exacerbated by either dilated or hypertrophic forms of cardiomyopathy associated with chronic thyrotoxicosis. Gallop rhythms may be associated with heart failure due to any cause. Many of the clinical findings suggestive of heart disease are also associated with hyperthyroidism (see Table 4-3). For these reasons, clinicians must maintain a high index of suspicion for hyperthyroidism in an aged cat with cardiac signs. Veterinarians must also be aware that these two diseases may occur concurrently.
Some hyperthyroid cats have predominating signs of cardiovascular or respiratory disease. Clinicians are challenged to remember a complete list of disorders that belong in the differential diagnosis (including hyperthyroidism). In addition to abnormalities directly associated with cardiac disease, other signs such as dyspnea, muffled heart sounds, and ascites may be detected and assumed to result from a primary cardiac disorder rather than from hyperthyroidism. Hyperthyroidism in cats can induce a variety of cardiac-related disturbances, most notably secondary cardiomyopathies. Hypertrophic cardiomyopathies are much more common in these cats than the dilated type. Either form of cardiomyopathy may result in heart failure, with severe failure more common among hyperthyroid cats with the dilated form of cardiomyopathy (Jacobs and Panciera, 1992).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree