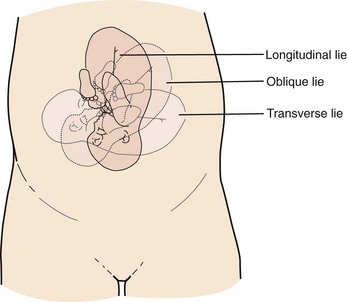
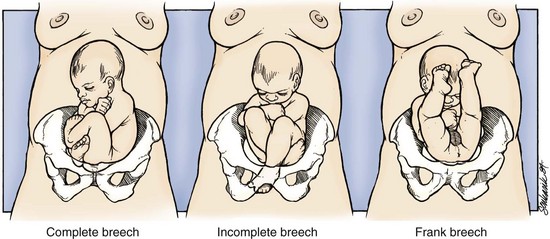
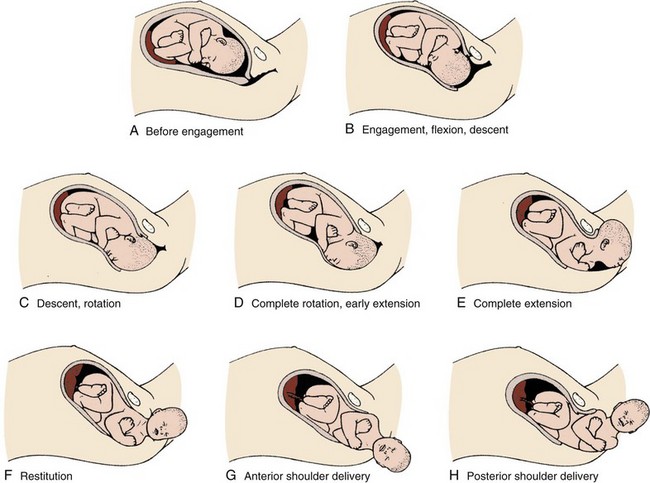
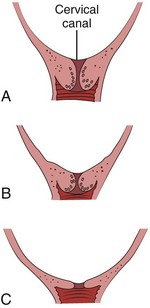
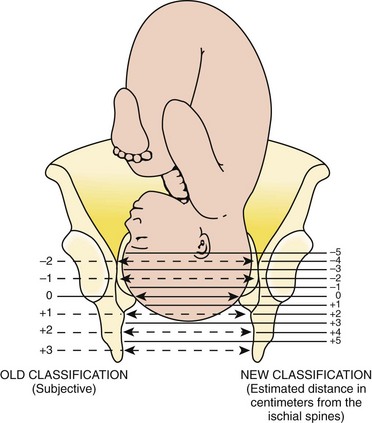
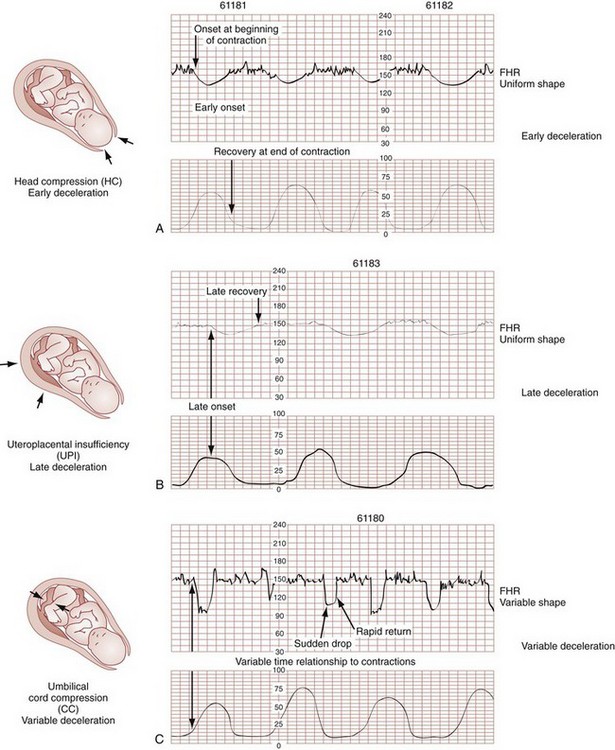
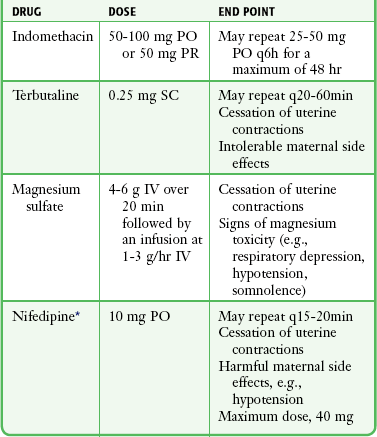
Chapter 56 Of the more than 4.1 million births in the United States in 2009, 99% were delivered in a hospital setting. The percentage of these births that occur in the emergency department (ED) setting is unknown.1 Childbirth is a relatively rare occurrence in the ED and is not identified as a specific diagnosis by the Centers for Disease Control and Prevention. It is instead categorized in the “supplemental classification,” along with other miscellaneous and noncodable diagnoses.2 Emergency delivery of an infant continues to be one of the most challenging and stress-inducing procedures facing emergency physicians (EPs). The clinician needs to assess the mother and fetus, prepare for delivery, and anticipate potential difficulties or complications during and after the birthing process. Labor is the process by which the fetus is expelled from the uterus. It begins with a sequence of regular and effective uterine contractions that result in effacement and dilation of the cervix.3 Identification of true labor versus false labor is best determined in a dedicated obstetric unit, often with external uterine monitoring. Labor can also be divided into phases. The latent phase of labor is the period between its onset and when labor becomes active, which generally requires 80% effacement and cervical dilation of greater than 4 cm.4 Active labor is normally divided into three generally progressive stages. The first stage begins with cervical effacement and dilation and ends when the cervix is completed dilated. In multiparous women this stage of labor typically lasts about 5 to 8 hours, as opposed to 7 to 13 hours in nulliparous women, but with much individual variation.3,4 The second stage of labor begins when dilation of the cervix is complete and ends with delivery of the infant. The duration of this stage is also variable, with a median of 50 to 60 minutes in nulliparas and 15 to 20 minutes in multiparas.3,4 The third stage of labor begins after delivery of the infant and ends with delivery of the placenta. The fourth stage of labor refers to the 1 hour immediately after delivery, the period in which postpartum hemorrhage is most likely to occur.3 It is recommended that maternal blood pressure and pulse be recorded immediately after delivery and every 15 minutes for the first hour to rapidly detect any ongoing hemorrhage.3 Show or bloody show is a sign of approaching labor. The normal mucous plug sealing the cervix discharges as the cervix dilates. Show consists of a small amount of blood-tinged mucus discharged from the vagina and indicates that labor is already in progress or will probably occur during the next several hours to a few days. The coloring of the mucus can become pink or brown tinged as a result of minor bleeding. However, if more than a small amount of blood escapes with the mucous plug, an abnormal cause such as abruption of the placenta or placenta previa should be considered. Digital vaginal examination under these circumstances is generally contraindicated.3 Spontaneous rupture of membranes can occur during the course of active labor, typically evident by a sudden gush or continuous leakage of a variable amount of clear or slightly turbid vaginal fluid. Rupture of membranes before the onset of labor at any stage of gestation is referred to as premature rupture of membranes (PROM). Term PROM, which occurs before the onset of labor, complicates approximately 8% of pregnancies.5 In the majority of cases it is followed by the onset of labor and delivery within 5 hours.5 The most significant maternal risk associated with term PROM is intrauterine infection. Fetal risks associated with PROM include umbilical cord compression and ascending infection.5 The ideal management of PROM should be deferred to the consulting obstetrician.6 Membrane rupture occurring before 37 weeks of gestation is called preterm premature rupture of membranes (pPROM). Birth within 1 week generally occurs regardless of management or the clinical findings. The most significant maternal risk related to pPROM is intrauterine infection. The most significant risks to the fetus are complications related to prematurity. Preterm delivery occurs in approximately 12% of all births in the United States.5 Accurate diagnosis of PROM will be helpful in further management. Suspected PROM should be confirmed by an examination that minimizes the risk of introducing infection. Avoid digital cervical examination unless the patient is in active labor or delivery is imminent.5 A sterile speculum examination can be performed to look for amniotic fluid extruding from the cervical os or pooling in the posterior fornix, as well as to inspect for fetal or umbilical cord prolapse and assess cervical effacement and dilation.3,5 Amniotic fluid may be differentiated from vaginal fluid by testing the pH of the fluid with Nitrazine paper or similar swab devices (Fig. 56-1). The pH of vaginal fluid is generally 4.5 to 6.0, whereas amniotic fluid has a pH of 7.0 to 7.5. The yellow testing paper turns blue-green to deep blue in the presence of amniotic fluid. With vaginal secretions the Nitrazine paper remains yellow.3,5 False-positive results may occur with blood, semen, bacterial vaginosis, or alkaline urine. If rupture of membranes is documented in the ED, notify the patient’s obstetrician and plan for hospital admission or possible transfer. When a woman is initially seen with contractions, the general condition of both the fetus and mother should be assessed quickly. Under the federal Emergency Medical Treatment and Labor Act (EMTALA), hospitals with an ED must conduct an appropriate screening examination to rule out true labor. In addition, under EMTALA, a woman in labor is considered unstable for interhospital transfer unless done so at the direction of the patient or a physician who certifies that the benefits outweigh the risks of transfer.3 A brief obstetric history, including the onset and frequency of contractions, the presence or absence of bleeding, possible loss of amniotic fluid, previous prenatal care, and due date, should be obtained. In the absence of active vaginal bleeding, a sterile vaginal examination should be performed in addition to maternal abdominal palpation to determine the stage of labor, as well as the position, presentation, and lie of the fetus. Monitor fetal well-being by evaluation of the fetal heart rate, particularly immediately after a uterine contraction. In an ED setting, fetal assessment is increasingly done via bedside ultrasonography, which can assess fetal movement and heart rate (Fig. 56-2). The traditional approaches of using external Doppler or auscultation are also acceptable. The normal baseline fetal heart rate is 110 to 160 beats per minute. Lie refers to the relationship of the long axis of the fetus to the long axis of the uterus. It is either longitudinal, transverse, or oblique (Fig. 56-3). Oblique lies are unstable and will convert to a longitudinal or transverse lie during labor. Longitudinal lies occur in more than 99% of pregnancies at term.3 Transverse lies generally cannot be safely delivered vaginally.4 The presentation, or presenting part, refers to the portion of the body of the fetus nearest to or foremost in the birth canal. The presenting part can be felt through the cervix on sterile vaginal examination. In longitudinal lies, the presenting part is the fetal head, the buttocks (breech), or the feet (footling breech). With a transverse lie, the presenting part is the shoulder. The presentation can be cephalic, breech, shoulder, or compound. All presentations except cephalic are considered malpresentations.7 Breech presentations are classified as frank, complete, or incomplete (Fig. 56-4). A fetus presenting with the buttocks and hips flexed and the legs extended is termed a frank breech. Presentation of the buttocks with flexion of the fetal hips and knees results in a complete breech presentation. When one or both of the feet or knees are lowermost in the canal, an incomplete or footling breech results. At or near term, 97% of fetuses will be vertex and 3% will be breech.3 The incidence of breech delivery is approximately 25% at 28 weeks, 17% at 30 weeks, and 11% at 32 weeks.3,8,9 The mechanism of labor in vertex presentations consists of engagement of the presenting part, flexion, descent, internal rotation, extension, external rotation or restitution, and expulsion (Fig. 56-5).3 These are often referred to as cardinal movements. The mechanism of labor is determined by the pelvic dimensions and configuration, the size of the fetus, and the strength of the uterine contractions. Essentially, the fetus will follow the path of least resistance by adaptation of the smallest achievable diameter of the presenting part to the most favorable dimensions and contours of the birth canal. The sequence of movements in vertex presentations is as follows: 1. Engagement refers to the mechanism by which the greatest transverse diameter of the head, the biparietal diameter in occiput presentations, passes through the pelvic inlet. A fetus is engaged when the presenting part is at 0 station. In a primiparous patient, it usually occurs in the last 2 weeks of pregnancy; in a multiparous patient, it can occur at the onset of labor. 2. Flexion of the head is necessary to minimize the presenting cross-sectional diameter of the head during passage through the smallest diameter of the bony pelvis. In most cases, flexion is necessary for both engagement and descent and occurs passively. 3. Descent is the downward passage of the fetal presenting part. It is gradually progressive but is not necessarily continuous. Descent is affected by uterine and abdominal contractions, as well as by straightening and extension of the fetal body. 4. Internal rotation occurs with descent and is necessary for the head or presenting part to traverse the ischial spines. This movement essentially turns the head such that the occiput gradually moves from its original, more transverse position anteriorly toward the symphysis pubis or, less commonly, posteriorly toward the hollow of the sacrum. This is known as occiput anterior or occiput posterior, respectively. 5. Extension occurs as the flexed head reaches the anteriorly directed vaginal introitus. The occiput reaches the inferior aspect of the pubic symphysis. The head is born by further extension as it rotates around the pubic symphysis and the occiput, bregma, forehead, nose, mouth, and finally, the chin pass successively over the anterior margin of the perineum. Immediately after its birth, the head drops downward such that the chin lies over the maternal anal region. 6. External rotation or restitution is return of the head to the correct anatomic position with respect to the fetal torso. It follows delivery of the head as it rotates to the transverse position that it occupied at engagement. This is also a passive movement. 7. Expulsion of the remainder of the fetal body then occurs. The shoulders descend in a path similar to that traced by the head (i.e., rotating anteroposteriorly for delivery). First, the anterior shoulder is delivered beneath the symphysis pubis followed by the posterior shoulder across the perineum. The mechanism of labor for breech presentations varies (see Fig. 56-4). The widest diameter that is engaged is the bitrochanteric diameter. Usually, the hips engage in one of the oblique diameters of the pelvic inlet. As descent occurs, the anterior hip generally descends more rapidly than the posterior hip. Internal rotation occurs as the bitrochanteric diameter assumes the anteroposterior (AP) position. Lateral flexion takes place as the anterior hip catches beneath the symphysis pubis, which allows the posterior hip to be born first. The infant’s body then rotates to allow engagement of the shoulders in an oblique orientation. Gradual descent occurs, with the anterior shoulder rotating to bring the shoulders into the AP diameter of the outlet. The anterior shoulder follows lateral flexion to appear beneath the symphysis, with the posterior shoulder being delivered first as the body is supported. The head tends to engage in the same diameter as the shoulders. Subsequent flexion, descent, and rotation of the head occur to bring the posterior portion of the neck under the symphysis pubis. The head is then born in flexion. Breech delivery is associated with a greater incidence of prematurity, prolapsed cord, and increased perinatal morbidity and mortality.3,10–12 The increased use of cesarean section has greatly decreased the morbidity and mortality associated with breech delivery. Although cesarean is the preferred method of delivery, vaginal delivery may be the method of choice in carefully selected cases.10,13,14 The emergency clinician should be cognizant of the imminent vaginal delivery of a breech infant in any presentation, frank, complete, or footling. However, a breech presentation is always problematic for any clinician, even under the best of circumstances. It is not expected that the EP will always be able to successfully deliver a breech presentation. To perform any vaginal breech delivery, the birth canal must be sufficiently large to allow passage of the fetus without trauma and the cervix must be completely effaced and dilated. If these conditions do not exist, cesarean section is indicated. To ensure full cervical dilation in a footling or complete breech, it is important that the feet, legs, and buttocks advance through the introitus to the level of the fetal umbilicus before the clinician intervenes and further delivery is attempted. The mere appearance of the feet through the vulva is not in itself an indication to proceed with delivery. This may be a footling presentation through a cervix that is not completely dilated. In this case there may be time to transfer the patient to the labor and delivery suite, preferably in the knee-chest position to minimize the risk for cord compression.15 Similarly, if the breech is frank, cervical dilation and outcome are improved if the infant is allowed to deliver to the level of the umbilicus. Before this, as with complete and footling presentations, there may be time to safely transfer the mother to the labor and delivery area. Tocolytics such as subcutaneous terbutaline may be used to inhibit labor until such patients can be safely transferred.15 Cleanse the perineum with an antiseptic and use a sterile lubricant to decrease potential contamination. A sterile vaginal (not speculum) examination is performed to identify the fetal presentation and position and assess the progress of labor, except in cases of suspected bleeding. Take care to avoid the anal region and potential fecal contamination during the digital examination. Assess cervical effacement and dilation, as well as fetal station, presentation, and position.3 The finger should not be withdrawn from the vagina until the examination is complete. The number of vaginal examinations during labor correlates with infectious morbidity, especially in cases of early membrane rupture.3 Cervical effacement refers to the process of cervical thinning that occurs before and during the first stage of labor as the cervical canal shortens from a length of about 2 cm to a circular opening with almost no length remaining (Fig. 56-6). Effacement is expressed as a percentage from 0% (uneffaced and thick) to 100% (completely effaced). Assess the degree of cervical effacement by palpation and determine the palpated length of the cervical canal in comparison to that of an uneffaced, or normal, cervical canal. Station refers to the level of the presenting fetal part in the birth canal relative to the ischial spines, which lie halfway between the pelvic inlet and the pelvic outlet (Fig. 56-7). Zero station is used to denote that the presenting part is at the level of the ischial spines. When the presenting part lies above the spines, the distance, estimated in centimeters ranging from 1 to 5, is stated in negative figures (−5, −4, −3, −2, −1). Below the ischial spines, the presenting fetal part passes +1, +2, +3, +4, and +5 stations to delivery. This measurement is made by simple palpation.3 The ischial spines can be palpated at roughly the 8- and 4-o’clock positions on the vaginal examination. The normal baseline fetal heart rate is 110 to 160 beats/min and varies considerably from a baseline measured for a minimum of 2 minutes in a 10-minute segment of time.16 Rates above or below this range may indicate fetal distress. Accelerations in the fetal heart rate lasting longer than 10 seconds and less than 2 minutes commonly occur during labor and are probably a physiologic response to fetal movement.3,16,17 Persistent fetal tachycardia occurs most frequently in response to maternal fever or amnionitis but may also indicate fetal compromise.3,16 As with brief accelerations in the fetal heart rate, a gradual decrease in the fetal heart rate in association with a uterine contraction with an onset to nadir of 30 seconds or more (with the nadir coinciding with the peak of contraction) is termed an early deceleration. Decelerations are physiologic and probably the result of vagal nerve stimulation secondary to compression of the fetal head. Decelerations that occur independently of uterine contractions, are abrupt, or last between 15 seconds and 2 minutes are known as variable decelerations. Late decelerations are those that are delayed in timing with respect to a contraction, with the nadir of the deceleration occurring after the peak of the contraction. Variable decelerations are relatively common and can be further classified according to their severity. Variable decelerations may be temporarily corrected by maternal repositioning. Late decelerations can be an ominous sign and may represent cord compression and uteroplacental insufficiency.3,16,17 It may necessitate emergency delivery. Changes in the fetal heart rate indicating fetal distress are usually evident immediately after a uterine contraction, and therefore the fetal heart rate is optimally assessed at this time. Formal monitoring of labor should be performed in an obstetrics unit. Fetal monitoring is not performed in the ED, but examples of various fetal heart rate patterns are included for completeness in Figure 56-8.3,16 If fetal distress is suspected on the basis of the resting fetal heart rate or changes after contractions, change the maternal position, typically into the left lateral decubitus position, and reevaluate. Administer supplemental oxygen to the mother to optimize fetal oxygenation. In the absence of bleeding, perform a vaginal examination to rule out the possibility of umbilical cord prolapse.16,18 Cord prolapse usually occurs at the same time as rupture of the membranes and is diagnosed by palpation of the umbilical cord on vaginal examination or by visualization of the cord protruding through the introitus. Cord prolapse is frequently encountered with breech presentations, multiple pregnancies, and prematurity.19–21 Management of cord prolapse is directed at sustaining fetal life until delivery is accomplished. Unless immediate delivery is feasible or the fetus is known to be dead, prepare for an emergency cesarean section. If immediate obstetric services are not available, four temporizing measures can be undertaken. (1) Place the patient in the knee-chest or deep Trendelenburg position, and keep the patient in this position until delivery.18,21,22 (2) Minimize compression of the umbilical cord by inserting a sterile gloved hand and exerting manual pressure in the vagina to lift and maintain the presenting part away from the prolapsed cord. (3) After manual elevation of the presenting part, instill 500 to 700 mL of saline into the bladder to raise the presenting part and maintain cord decompression. Once the bladder is filled, remove the vaginal hand.22,23 (4) Tocolytic therapy can be administered to decrease uterine contractions and improve fetoplacental perfusion.22,23 Unfortunately and realistically speaking, outcomes of true obstetric emergencies managed solely in the ED are often bleak and essentially out of the hands of the EP. Tocolytic therapy is rarely instituted in the ED, and there is no standard mandating its use by the EP. However, under dire circumstances and preferably under obstetric guidance, this intervention may be initiated in the ED. Before instituting pharmacologic tocolytic therapy for either preterm labor or fetal distress, initiate basic maneuvers to improve maternal and fetal status. Because uterine hypoxia may induce uterine contractions, administer supplemental oxygen and infuse 500 mL of crystalloid intravenously. Place the mother in the left lateral decubitus position to improve uterine perfusion.3,18,24 Because uterine, cervical, or urinary tract infections account for 20% to 40% of cases of preterm labor, search for a specific cause and treat infections appropriately.18,25,26 If the contractions persist and cervical changes are documented despite these basic interventions, consider pharmacologic therapy.3,18,24 Although tocolytic agents are commonly used and have been shown to prolong pregnancy by 2 to 7 days, there are few data to suggest that tocolysis improves long-term perinatal or neonatal outcome.3,24,27,28 In addition, none of the commonly used tocolytic medications are approved for use by the U.S. Food and Drug Administration (FDA) as a tocolytic agent. The principal benefit of pharmacologic therapy may be only to prolong pregnancy to allow maternal transfer to a tertiary care facility or to delay delivery sufficiently to improve fetal maturation with corticosteroids.3,24–26,29 General contraindications to tocolytic therapy include severe preeclampsia, placental abruption, intrauterine infection, advanced cervical dilation, and evidence of fetal compromise or placental insufficiency.24 There are no clear “first-line” tocolytic agents to manage preterm labor (Table 56-1). Clinical circumstances and preferences should dictate treatment. Agents such as calcium channel blockers and the prostaglandin inhibitor indomethacin have shown varying efficacy in clinical trials.3,16,24,25,27 The most commonly used tocolytic agents in the United States are the calcium channel blocker nifedipine, magnesium sulfate, and the β2-receptor agonist terbutaline. Calcium channel blockers are the preferred tocolytics by the World Health Organization.30 The most commonly used β2-adrenergic tocolytic agent is terbutaline. The β-mimetic agents react with adrenergic receptors to reduce intracellular ionized calcium levels and prevent the activation of myometrial contractile proteins.3 Although terbutaline stimulates β2-receptors primarily, it has some β1-activity, which is responsible for its cardiovascular side effects. Another β-mimetic agent, ritodrine, was the only agent approved for tocolysis in the United States but has been withdrawn from the market. Terbutaline is commonly used for the treatment of preterm labor.3,25,31 When given subcutaneously, administer terbutaline in a 0.25-mg dose and repeat it every 20 to 60 minutes until contractions cease or intolerable maternal side effects occur.18,24,32,33 In 2011 the FDA required the addition of a Boxed Warning and Contraindication (“black box warning”) against the use of injectable terbutaline for the prevention or prolonged treatment of preterm labor beyond 48 to 72 hours because of adverse effects, including maternal death.34 Use terbutaline with caution in patients with cardiovascular disease, hypertension, hyperthyroidism, diabetes, and seizures and in those taking other sympathomimetic amines.24,35 The general clinical side effects of arrhythmias, myocardial ischemia, and pulmonary edema are related to its inherent activity as a β-mimetic drug. Treatment of the majority of side effects is supportive; severe cardiovascular effects may be treated with β-blocking agents.32,35 Magnesium sulfate (MgSO4) is not approved in the United States for use as a tocolytic agent. Nevertheless, some perinatal centers prefer MgSO4 over the β-mimetic agents because of its lower incidence of side effects.18,36,37 Even though the use of MgSO4 as a tocolytic has fallen out of favor, findings of fetal neuroprotective effects have resulted in its ongoing use.38–41 Although its mechanism of action is not fully understood, magnesium probably decreases myometrial contractility through its role as a calcium antagonist.3 Its fetoprotective effects probably result from noncompetitive antagonism of the N-methyl-d-aspartate receptor or through antiapoptosis and prevention of neuronal cell loss.42 MgSO4 is generally administered at a dose of 4 to 6 g intravenously over a period of 20 to 30 minutes, followed by a maintenance intravenous infusion beginning at 1 to 3 g/hr.24,43 Infusion of MgSO4 often produces sweating, warmth, and flushing. Rapid parenteral administration may cause transient nausea, vomiting, headache, or palpitations.24,25,37 The major side effect of magnesium therapy is impairment of the muscles of respiration with subsequent respiratory arrest, an effect not usually seen until the serum magnesium level exceeds 10 mEq/L. At levels of 12 mEq/L or greater, respiratory arrest may occur.35 The first sign of magnesium toxicity, a decrease in the patellar reflex, typically occurs as serum magnesium levels exceed 4 mEq/L, with loss of the reflex as levels increase further. The dosing and ongoing maintenance of magnesium therapy should be guided by the clinical status of the patient rather than by laboratory values. Monitor the patellar reflex throughout therapy. Because magnesium is almost totally excreted by the kidney, it is contraindicated in the presence of renal failure. Monitor urinary output and renal function throughout therapy. If respiratory depression develops, inject 10 mL of a 10% solution of calcium gluconate or calcium chloride over a 3-minute period as an antidote. For severe respiratory depression or arrest, prompt endotracheal intubation may be lifesaving.3 Calcium antagonists inhibit the influx of calcium ions through the muscle cell membrane and reduce uterine vascular resistance. The decrease in intracellular calcium also results in decreased myometrial activity. Although dosing regimens vary, nifedipine is frequently given as an initial loading dose of 30 mg orally and then 10 to 20 mg every 4 to 6 hours.24,32 When oral nicardipine (Cardene) was compared with MgSO4, less time was required to achieve tocolysis, 3.3 versus 5.3 hours, respectively. Preterm labor also recurred less frequently with nicardipine.44 The calcium channel blocker–induced decreased vascular resistance can lead to maternal hypotension and thus decreased uteroplacental perfusion.
Emergency Childbirth
Background
Anatomy and Physiology
Identification of Labor
Evaluation of Labor
Labor Movements: Vertex
Labor Movements: Breech
Types
Vaginal Examination
Fetal Well-Being
Management of Fetal Distress
Tocolytic Therapy
β2-Receptor Agonists
Magnesium Sulfate
Calcium Channel Blockers
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine