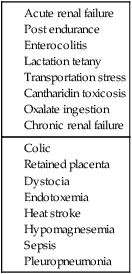
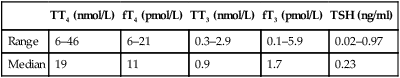
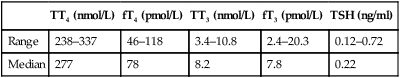
Calcium deficiency in the horse can be acute or chronic and result from a variety of conditions (Table 6.1). Chronic deficiency presents as abnormal cartilage and bone development with or without lameness. Acute deficiencies result in clinical signs associated with neuromuscular excitability. The clinical consequences that are seen are varied and will be discussed individually. • The calculated deficit should ideally be based on the ionized calcium concentration but most laboratories measure total calcium. • When treating hypocalcemia it is important to consider: • Rate of development: treatment is more critical in horses that have developed a rapid deficit. • Ongoing losses: lactating mares, compromised intestinal function. These horses may continue to be hypocalcemic despite aggressive replacement therapy. • Many horses with ionized hypocalcemia may only have mild undectable signs but may progress to develop other signs such as ileus. • Horses with functional kidneys can eliminate large amounts of calcium rapidly and it is rare to induce hypercalcemia from calcium administration but rapid administration could potentially result in cardiovascular complications. Current recommendations for speed of replacement are 1–2 mg/kg/h. • History of diet and clincial signs may be suggestive. Clinical laboratory findings may include hypocalcemia and hyperphosphatemia but this is not consistent and in some cases they may be within normal ranges. Serum intact PTH concentrations are increased. • Dietary manipulation by increasing calcium supplementation can result in rapid improvement in early cases but more advanced cases may require prolonged therapy (9–12 months). Affected animals should receive 100–300 g/day of calcium with the diet overall having a Ca : P ratio of 3 : 1 to 4 : 1. Bound or free forms of T3 or T4 can be measured in readily available assays (see Tables 6.2 and 6.3). It is best to measure levels of free hormone as changes in protein binding can alter the total level. Table 6.2 Baseline concentrations of thyroid hormones in healthy adult horses Table 6.3 Baseline concentrations of thyroid hormones in healthy foals Adapted from Braehus BA, 2009 Thyroid disease. In: Robinson NE, Sprayberry KA (eds) Current Therapy in Equine Medicine, sixth ed., pp. 738–739. WB Saunders, Philadelphia, PA, USA. • High resting concentrations of thyroid hormones. • Administration of exogenous T3 failed to suppress endogenous T4 concentrations. • Due to the relationship with thyroid gland neoplasia further tests to rule in or out a neoplasia would include ultrasound, biopsy or nuclear scintigraphy. • Treatment could involve removal of a portion or all of the thyroid gland followed by supplementation with thyroid hormones.
Disorders of metabolism, nutrition and endocrine diseases
Developmental disorders
Hypocalcemia
Retained placenta
Diagnosis and treatment of hypocalcemia
Hypercalcemic disorders
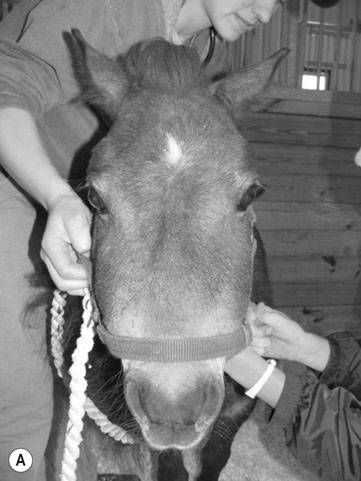
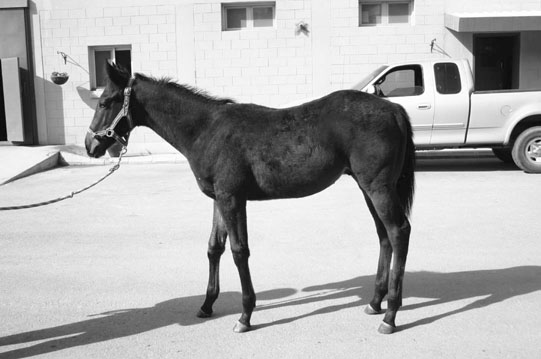
Primary hyperparathyroidism (Figs. 6.1–6.4)



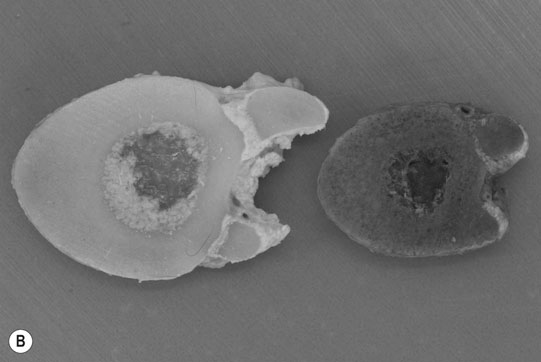
Secondary hyperparathyroidism (Figs. 6.5–6.7)

Differential diagnosis:

Diagnosis and treatment
Thyroid disease
TT4 (nmol/L)
fT4 (pmol/L)
TT3 (nmol/L)
fT3 (pmol/L)
TSH (ng/ml)
Range
6–46
6–21
0.3–2.9
0.1–5.9
0.02–0.97
Median
19
11
0.9
1.7
0.23
TT4 (nmol/L)
fT4 (pmol/L)
TT3 (nmol/L)
fT3 (pmol/L)
TSH (ng/ml)
Range
238–337
46–118
3.4–10.8
2.4–20.3
0.12–0.72
Median
277
78
8.2
7.8
0.22
Hyperthyroidism
Diagnosis and treatment
Disorders of metabolism, nutrition and endocrine diseases