Chapter 74Diseases of the Digital Flexor Tendon Sheath, Palmar Annular Ligament, and Digital Annular Ligaments
Anatomical Considerations
Within the DFTS, the SDFT and DDFT are intimately related. A fibrous ring (the manica flexoria) emanates from the lateral and medial borders of the SDFT and encircles the DDFT completely, from the proximal limit of the DFTS to the proximal aspect of the PSBs. The synovial lining of the DFTS adheres to the palmar surface of the SDFT in the sagittal midline proximal to the PAL, along the dorsal surface of the PAL and along the dorsal surface of the proximal digital annular ligament. The synovial lining of the DFTS also adheres to the palmar surface of the DDFT between the proximal digital annular ligament and the distal digital annular ligament, and along the dorsal surface of the distal digital annular ligament. The sagittal adhesion-like mesotendon between the SDFT and PAL is referred to as the vinculum of the SDFT. The DDFT also has a mesotendon that attaches to its palmar surface at the level of the proximal interphalangeal joint (see Figure 70-2, B). These mesotendon attachments contain vascular branches that contribute to the arterial supply of the intrasynovial part of the tendon.
Diagnostic Techniques
Diagnostic techniques that localize disease to the DFTS include synoviocentesis and synovial fluid analysis and intrathecal or perineural injection of local anesthetic solution. Synoviocentesis of the DFTS can be performed in one of the several recesses of the sheath. Access to the proximal pouch is possible when the sheath is distended with synovial fluid but difficult when it is not. Synoviocentesis can be achieved by introducing a 2.5-cm needle along the dorsal aspect of the DDFT, between the DDFT and the lateral branch of the SL, a few centimeters proximal to the lateral PSB. Easier access can be gained via the distal palmar pouch of the sheath, which extends between the two distal branches of the SDFT and between the two digital annular ligaments, along the palmar surface of the DDFT. One should remember that this pouch is divided sagittally by the mesotendon of the DDFT in its distal part. The needle can be introduced through the skin to one side of the midline and, to avoid iatrogenic damage to the DDFT, gently and slowly advanced at approximately 45 degrees to the skin surface until synovial fluid is seen at the needle hub. To increase distention of the distal palmar recess, it can be useful temporarily to compress the proximal pouch by firm application of an elasticated bandage (see Figure 124-1). Alternatively, the needle can be aimed to access this pouch between the lateral or medial border of the DDFT and the ipsilateral distal branch of the SDFT, which will prevent inadvertent needle penetration of the DDFT, although the palmar pouch of the proximal interphalangeal joint can be entered if the needle is introduced too deeply. The DFTS also can be accessed through its proximal or distal collateral recesses. The proximal collateral recess is situated in the triangular space palmaromedially or palmarolaterally, between the base of a PSB, the proximal insertion of the proximal digital annular ligament, and the dorsal border of the DDFT. The space can be entered 1 cm distal to the base of a PSB and 1 cm palmar or plantar to the neurovascular bundle. The distal collateral recess is located on the lateral (or medial) aspect of the pastern, between the digital flexor tendons and the distal sesamoidean ligaments and between the proximal and distal insertions of the proximal digital annular ligament. A cadaver study showed that synoviocentesis of the DFTS using these techniques was most consistently successful when performed at the level of the proximal lateral recess on a non–weight-bearing limb.2 In addition, a palmar-plantar axial sesamoidean approach was described where the needle was introduced axial to the PSB in the flexed limb. This technique was described as being optimal for synoviocentesis.3 Ten milliliters of local anesthetic solution is injected for adequate analgesia of the DFTS (see Chapter 10). It is important to recognize that intrathecal analgesia of the DFTS is not specific for elimination of pain from the contained structures and can influence pain from the oblique and straight sesamoidean ligaments.5 Moreover, in some horses with DFTS pathology, the response to perineural analgesia is better than to intrathecal analgesia.
Imaging of the Digital Flexor Tendon Sheath
Diagnostic ultrasonography is by far the most commonly used technique for evaluating the DFTS. The DFTS is first encountered at level 3A and continues distally to level P1C and beyond (see Chapter 16).8 The PAL can be demonstrated in normal horses as a thin (1 to 2 mm) echogenic band immediately adjacent to the palmar surface of the SDFT at level 3C. The proximal digital annular ligament and distal digital annular ligament usually cannot be recognized in the palmar midline, unless they are abnormally thickened. The vinculum of the SDFT at the level of the PSB is easily identifiable by ultrasonography, but the distal mesotendon of the DDFT in the phalangeal region is only occasionally visible, usually when distention of the DFTS provides negative contrast (see Figure 70-2, B). A normal synovial reflection or mesotendon joins the lateral and medial borders of the DDFT in the proximal recess of the DFTS, which should not be mistaken for an adhesion (see Figure 70-2, A). The thickness of the DFTS can be assessed at levels 3A and 3B, where the capsule is identifiable as an echogenic band dorsal to the DDFT and the manica flexoria.
Survey radiography of the DFTS is performed to demonstrate evidence of intrathecal air or gas caused by a penetrating wound, the presence of metaplastic mineralization of injured soft tissue structures, or concurrent pathological conditions of the bone. Positive contrast radiography10 may provide the most conclusive evidence of wound communication with the synovial space and may also provide additional information in the diagnosis of synovioceles associated with the DFTS. Although fistulography and filling of the intrathecal space with sterile iodine-based contrast medium is diagnostic of communication between the wound and the DFTS, we prefer to access the DFTS by placing a needle at a site remote from the wound. This minimizes the risk of forcing bacteria or foreign material present in the deeper layers of the wound into the synovial space. Using a remote site further avoids the risk of inadvertently introducing bacteria while passing the needle through an area of cellulitis into the synovial cavity. Infiltration of 10 to 20 mL of sterile contrast medium followed by manipulation of the digit should result in flow of contrast medium from the wound and can be demonstrated radiologically (Figure 74-1).
Tenoscopy is the ultimate imaging modality for evaluating the internal structures of the DFTS.11 An endoscope is introduced routinely in the proximal collateral recess of the sheath, 1 cm distal to the base of the PSB and 1 cm palmar or plantar to the neurovascular bundle, but access to other synovial recesses is also possible (see Chapter 24). This approach allows for a complete examination of the DFTS and its contents, except for the palmar surface of the SDFT, unless substantial thickening of any of the annular ligaments or extensive subcutaneous fibrosis has occurred. Access in ponies and cob-types with very thick skin can also be difficult. The approach also facilitates therapeutic maneuvers within the DFTS, such as PAL desmotomy, adhesiotomy, synovial mass removal, and debridement of fibrillated or torn areas of the digital flexor tendons, manica flexoria, or intersesamoidean ligament.
Diseases of the Digital Flexor Tendon Sheath
Noninfectious Tenosynovitis
Etiopathogenesis
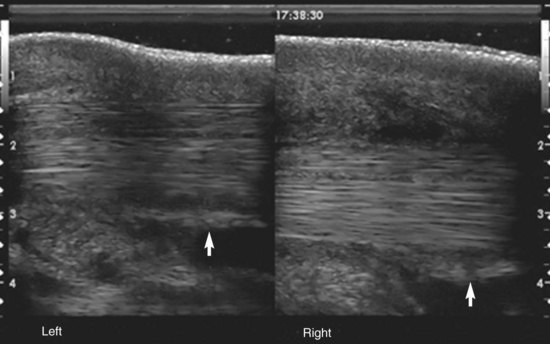
Acute noninfectious tenosynovitis is a traumatic synovitis/capsulitis of the sheath lining. As for joints, a traumatic synovitis/capsulitis can be caused by accumulative low-grade trauma associated with normal exercise, acute trauma associated with direct impact force (e.g., overreach), or an abnormal force outside the normal range of movement of the fetlock region (e.g., hyperextension). Synovitis/capsulitis is more frequently secondary to damage to the internal or supporting structures of the DFTS, such as disruption of the visceral or parietal synovial layers, tearing of the vincula, tearing of the sheath wall with herniation or synoviocele formation, central or marginal damage to the flexor tendons, tearing of the manica flexoria, and spraining of the PAL or proximal digital annular ligament. Each of these complicating conditions is likely to result in continuous irritation of the sheath and cause chronic tenosynovitis. Chronic tenosynovitis may be associated with villonodular thickening of the sheath lining, especially in the proximal recess; adhesion formation between the visceral and parietal synovial lining; and fibrosis with reduced elasticity of the DFTS capsule. When these conditions are present, a self-perpetuating cycle occurs of improvement with rest, followed by repeated inflammation with exercise. This results in increased inflammation and lameness, further fibrosis, and eventually thickening of the PAL and stenosis of the fetlock canal (see the following discussion of PAL syndrome). Complex tenosynovitis has been defined as tenosynovitis with thickening of the PAL, synovial distention, and adhesions or synovial masses, or both (Figure 74-2).12 Windgalls, especially those occurring bilaterally in the hindlimbs, are another form of low-grade chronic tenosynovitis. Although lameness is not usually a feature of windgalls, the synovial effusion is still likely to reflect the presence of low-grade chronic synovitis of the DFTS, caused by the continuous stress of use-induced overloading.
Diagnosis
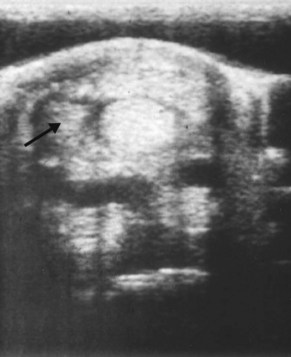
Ultrasonographic examination is essential for identifying any primary pathology responsible for the tenosynovitis, such as adhesions and complicating injuries of the digital flexor tendons (see Figure 69-8, A), the intersesamoidean ligament, or annular ligaments, and to document the staging of the condition.13 DFTS effusion may also accompany injury to the intrathecal part of the SDFT associated with a classic bowed tendon (see Chapter 69). However, intrathecal tendon injuries occur more commonly as focal core lesions in the DDFT (see Chapter 70) or as longitudinal tears of the SDFT, DDFT, or manica flexoria. DDFT tears usually involve the lateral or medial borders of the tendon in the forelimb; hence oblique ultrasonographic views can sometimes identify defects on these borders, although they are easily missed. Oblique images are also required to image the abaxial margins of the SDFT. Manica flexoria tears are more frequently seen in hindlimb tenosynovitis and are also easily missed using transverse ultrasonographic images because the tears are usually incomplete and located at the site of attachment of the manica flexoria to the SDFT. Recently, we have found that a midline longitudinal scan immediately proximal to the PSBs provides the best image for identifying instability and/or thickening of the manica flexoria that accompanies tears (Figure 74-3). However, negative ultrasonographic findings do not preclude a tear in the manica flexoria.