Caroline Hahn
Diseases Associated With Clinical Signs Originating From Cranial Nerves
The nerves emanating from the brainstem (the midbrain, pons, medulla, and cerebellum), whether they are sensory or motor, autonomic or somatic, are called cranial nerves. The brainstem and cranial nerves coordinate and control unconscious sensory, proprioceptive, and motor functions. Disorders of these structures are characterized by one to all of a set of distinctive abnormal neurologic signs.
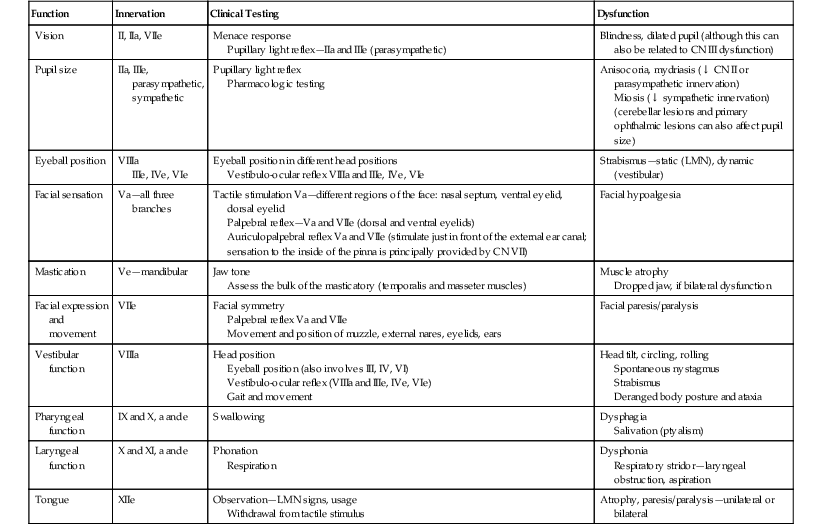
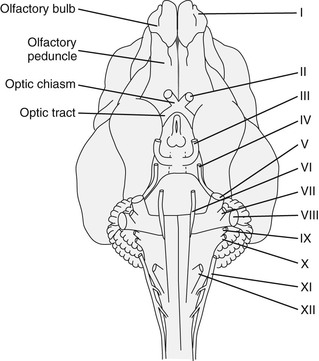
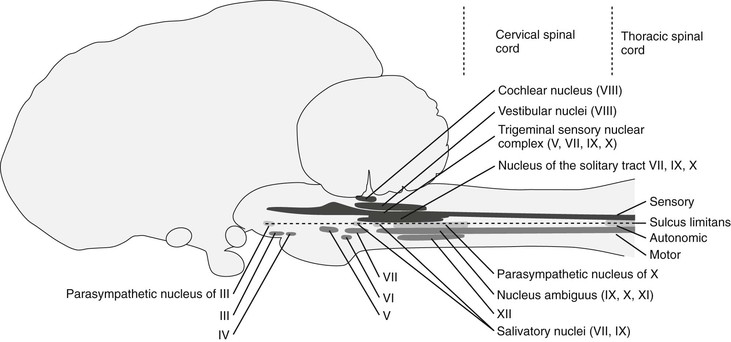
Twelve pairs of cranial nerves innervate the head and extend into the body, and each nerve may carry motor, sensory, or both types of nerve fibers, and may mediate somatic, autonomic, or both types of functions (Table 83-1). Knowledge of the location and action of individual cranial nerves is critical for interpretation of the neurologic examination (see the sixth edition of Current Therapy in Equine Medicine, Chapter 130). Cranial nerves and their central nervous system (CNS) components are numbered sequentially from rostral to caudal on the basis of site of attachment to the brain: cranial nerve I (CN I; olfactory) and CN II (optic) attach to the forebrain; CNs III (oculomotor) and IV (trochlear) are associated with the midbrain (rostral brainstem); CNs V (trigeminal), VI (abducens), VII (facial), VIII (vestibulocochlear), IX (glossopharyngeal), X (vagus), XI (spinal accessory), and XII (hypoglossal) are associated with the mid and caudal portions of the brainstem. All but the optic and olfactory nerves have a peripheral portion that is ensheathed or myelinated by Schwann cells. Cranial nerves I and II are not peripheral “nerves” at all, but are actually extensions of the CNS; early anatomists assumed that these two structures were peripheral nerves, and the nomenclature has persisted. Cranial nerve nuclei can have two names, depending on whether their function is somatic or autonomic (parasympathetic). For example, the oculomotor nucleus of CN III supplies some of the extraocular muscles, whereas the parasympathetic nucleus of CN III innervates smooth muscle of the eye and orbit. Some nuclei contain neurons of multiple cranial nerves, yet all those neurons have a similar function. For example, the nucleus ambiguus, comprising neurons associated with CN IX, X, and XI, innervates the striated muscle of the larynx and pharynx.
An understanding of the relative position of the peripheral portion of the cranial nerves (Figure 83-1), as well as the location of their nuclei (Figure 83-2), is important in establishing whether a particular combination of cranial nerve signs could be caused by a single lesion or has to involve a multifocal disease process. A lesion affecting a particular cranial nerve could be affecting the peripheral nerve or its soma in the brainstem, and a thorough neurologic examination and ancillary tests may be required to establish the exact location—brainstem lesions can be expected to additionally affect other cranial nerves as well as upper motor neuron and proprioceptive tracts and, if the ascending reticular activating system is additionally affected, abnormalities in levels of arousal. Neurons of CNs III to XII are arranged in nuclei in the brainstem.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree