chapter 22 Digital Radiography
Upon completion of this chapter the reader should be able to do the following:
ADC: Analog to digital converter. An electronic device that converts an analog voltage signal to a digital signal.
ALARA: As low as reasonably achievable. This acronym refers to a basic principle of radiation safety—to use the lowest amount of ionizing radiation as possible.
Analog: A voltage waveform that is continuous; at any point in time there is a voltage value.
Bit: A binary digit, either 0 or 1.
Bmp: Bit map. A representation of a graphic image stored in computer memory as rows and columns of dots; each dot is stored in one or more bits of information. Dot density, or resolution, is expressed as dots per inch (dpi). Images displayed on a monitor are converted from bit maps to pixels.
CCD: Charged coupled device. A small flat panel device that is capable of creating images from visible light, used for digital radiography and digital photography.
CD-ROM: Compact disk, read-only memory. A CD-ROM (or CD) is a 5-inch diameter optical storage device with a capacity of approximately 700 megabytes (MB).
Compression: A mathematical reduction in size of digital data so that they are easier (faster) to transmit. Loss-less compression allows perfect decompression of compressed data without loss of information. With lossy compression, a portion of original digital data is lost and cannot be restored. The advantage of lossy compression is that higher compression levels can be attained.
Contrast resolution: The ability to distinguish between two structures of differing x-ray attenuation. The high-contrast resolution of digital radiography is vastly superior to conventional screen-film radiography.
CR: Computed radiography. A type of digital radiography that uses a photostimulable phosphor plate for image acquisition.
DICOM: Digital Imaging and Communications in Medicine. The global standard in the human medical industry for transmission of medical images and related information. A joint committee of the American College of Radiology and the National Electrical Manufacturers’ Association (ACR-NEMA) is responsible for the continuous development of DICOM standards. DICOM is intended to realize the interoperability of multiple medical imaging devices manufactured by different vendors including the display and transmission of images and information.
Digital: To use digits (rather than numbers); data stored, displayed, or represented in numerical digits (binary). Images are converted into electronic bits.
DDR: Direct digital radiography. A digital radiography system in which there is direct conversion of x-ray energy into an electronic (digital) signal. Although DDR offers the best in digital radiography resolution, the technology is currently expensive and not yet commonly used.
DR: Digital radiography. Term used to denote any type of digital radiography including computed radiography, CCD technology, flat panel detectors, and direct radiography units.
DVD: Digital video (versatile) disk. A 5-inch diameter optical disk with approximately 5 gigabyte (GB) storage capacity.
Ethernet: A low-level networking standard used in local area networks. It defines wiring specifics and types of electrical signals transmitted.
Firewall: An electronic “security wall” that connects two or more computer networks yet secures one network from the other.
FTP: File transfer protocol. A high-level protocol designed for reliable transfer of digital files from computer to computer via the Internet. Transmission requires permission of both the sender and the recipient. A variant of FTP, anonymous FTP, allows information to be accessed by logging in a user name of anonymous. A Web database of anonymous FTP sites is termed “Archie.”
HIS: Hospital information system. A computer-based information system necessary to manage a health care facility. Patient information, admission and discharge, billing, scheduling, medical procedures, and pharmacy are items that may be included in an HIS. Ideally, the HIS is integrated into the radiology information system.
HL-7: Health level 7. A nonprofit organization founded in 1987 that develops standards for transmission of electronic clinical, financial, and administrative data among health care computer systems.
HTTP: Hypertext transfer protocol. A high-level Internet protocol that defines the World Wide Web (www). This protocol allows Web browsers to speak to Web servers. Hypertext markup language (HTML) is the language used to transmit information.
Internet: Computers world wide connected by common high-level communication protocols using TCP/IP lower layer communication language.
IP: Internet protocol. A low-level protocol used to assign computer addresses. The addresses consist of 4 numbers between 0 and 255, each separated by a period (e.g., 199.193.45.7)
Jpeg (jpg): Joint Photographic Experts Group. A lossy compression technique and popular image format used to minimize file size and download time. It reduces file size to as low as 5% of the original size, with a loss of image resolution.
Matrix: A grid arrangement of pixels, expressed as numbers representing the amount of horizontal and vertical pixels used (e.g., 256 × 256).
PACS: Picture archiving and communication system. A broad term involving computers and components used to capture, transfer, store, and display medical digital information.
PSP: Photostimulable phosphor.
RAID: Redundant array of inexpensive disks. Multiple inexpensive disk archives are configured such that storage, access, and redundancy of information can be increased more reliably than by use of a single, larger-capacity disk.
RIS: Radiology information system. A computer system that handles all of the information necessary to operate a radiology department. RIS manages patient information, scheduling of imaging procedures, radiology reporting, and a database allowing case search capabilities. HIS, RIS, and PACS systems must communicate effectively.
Scintillation devices: Materials that emit visible or ultraviolet light when exposed to x-rays.
SCP: Service class provider. The DICOM term for a server program.
SCU: Service class user. The DICOM term for a client program.
Server: A computer system that provides information upon request from a client (user).
SMTP: Simple mail transport protocol.
Spatial resolution: The ability to distinguish between two small, separate structures. Loss of spatial resolution renders two closely spaced small objects to appear as one structure. Usually measured as line pairs per millimeter. The best screen-film systems still have better spatial resolution than digital systems, but this is compensated for by the increased contrast resolution that digital radiography offers.
TCP: Transmission control protocol. A protocol for breaking information into smaller packets for data transmission.
TIFF: Tagged image file format. A popular public domain raster file format for image storage. Digital radiographic images stored in TIFF format are not compressed and therefore are large files (megabytes).
WWW: World Wide Web. Internet computers that exchange information via the HTTP protocol.
DIGITAL RADIOGRAPHY: AN OVERVIEW
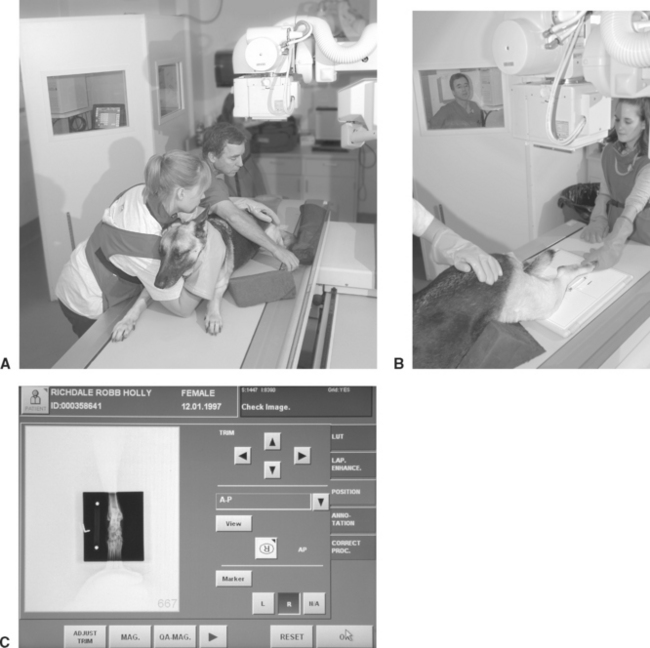
The concept of digital radiography is quite simple. The primary difference between conventional film-based radiology and digital radiology is that radiographic images are electronically captured, recorded, and viewed at a computer terminal, replacing radiographic film and the view box. The conventional screen-film cassette is replaced by a reusable image receptor (detector). The image receptor receives x-rays just as conventional intensifying screens do. Instead of exposing radiographic film, however, intensifying screens or other scintillation devices expose a “digital plate” that transforms emitted light to an electrical latent image. The different ways in which this is accomplished are discussed in detail in the following sections. The x-ray tube, generator, and peripheral x-ray machine hardware are essentially the same for conventional or digital radiography. Indeed, many of the available digital radiography systems use preexisting x-ray equipment (Fig. 22-1).
After the digital radiographic image is made, it is transferred to a dedicated digital radiography computer for “image processing” (Fig. 22-2). Here, the images can be adjusted as needed by the veterinary technologist. In small practices this may be the only computer available to view, but in most instances the processed image is finalized and then sent to another dedicated computer workstation for diagnostic interpretation by the veterinarian (Fig. 22-3). In large hospitals where multiple diagnostic workstations are necessary, the images will be sent to a main centralized computer (called a server) for storage and distribution to other workstation computers or sent off site via the World Wide Web for review.
ADVANTAGES OF DIGITAL RADIOGRAPHY
The Image
Unlike traditional screen-film radiography, kVp has little or no effect on the contrast or latitude of the digital image (this can be endlessly adjusted with software at the digital radiography computer terminal and diagnostic workstation). This flexibility is possible because of the linear relationship of the image receptors used for digital radiography. Simplistically, the number of electrons “trapped” by the digital image receptor during an x-ray exposure is linearly related to the intensity of the x-ray beam. Digital images have more latitude (more shades of gray) than film images and can display high-contrast body parts while simultaneously displaying soft tissues. This high gray-scale (high latitude) resolution is desirable because it allows observation of minor differences in radiation attenuation that may not be visible with film. When compared with conventional screen-film technique charts, digital technique charts do not vary greatly for the body part radiographed or patient thickness.
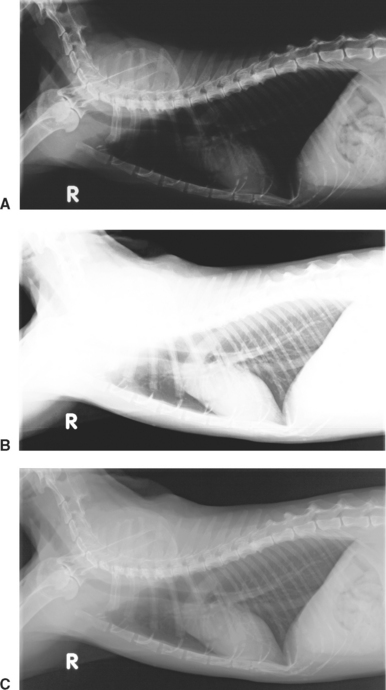
The higher-contrast resolution (or exposure latitude) of digital radiography has several tremendous advantages over conventional screen-film radiography. The need for retakes resulting from overexposure and underexposure is reduced, and for the most part eliminated. Images that are too light or dark that would be discarded on radiographic film can be adjusted with the digital image management software (Fig. 22-4). Marginal radiographic images, which may have previously been deemed acceptable, are a thing of the past.
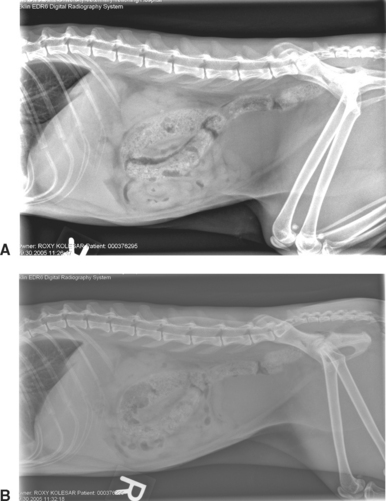
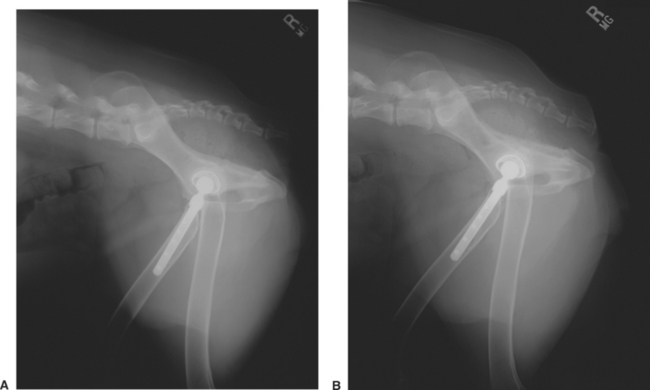
Computer manipulation of the digital image is a phenomenal advantage that digital radiography has over conventional screen-film radiography. Images can be altered for contrast or latitude (Fig. 22-5) and can be zoomed (magnified) (see Fig. 22-3) to scrutinize the image as if using a magnifying glass to view a radiographic film. Digital viewing software packages offer a variety of ways to view digital images including subtraction tools that make it possible to view bone-only or soft-tissue-only images from a single exposure. Digital radiography makes it possible to see both soft tissue and bony detail in a single image. Because of the high exposure latitude, an unprocessed digital image usually does not look the same as a film/screen radiograph. Although digital images can be manipulated to mimic the appearance of conventional radiographs (Fig. 22-6), usually the image is adjusted to take advantage of simultaneous high contrast and high latitude. Curiously, the appearance of digital images is resisted by some veterinarians who are accustomed to viewing high-contrast radiographs. Getting accustomed to viewing digital images is one small initial disadvantage of digital radiography, but quickly overcome.
The spatial resolution of digital images is at best the same, but usually slightly lower than a high-quality radiographic film image. This is not a disadvantage in most instances because there is a limit to how much spatial resolution the human eye can discriminate. As digital technology advances, differences in spatial resolution between conventional and digital radiography have become almost negligible. Human medical studies have shown that digital images are equal to or better than traditional film for evaluating most body parts. This is because there is a point at which spatial resolution yields way to contrast resolution (the ability to separate two structures of different contrast, or x-ray attenuation), the hallmark of what makes digital radiography so diagnostic. Image quality and the ability to detect abnormalities are actually more dependent on postdigital image acquisition processing than on spatial resolution. Digital radiography has been clinically validated for 20 years in various human medical settings including mammography, indicating that its minimally lower spatial resolution is not a clinical limitation.