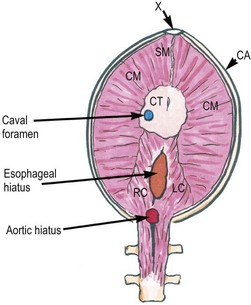
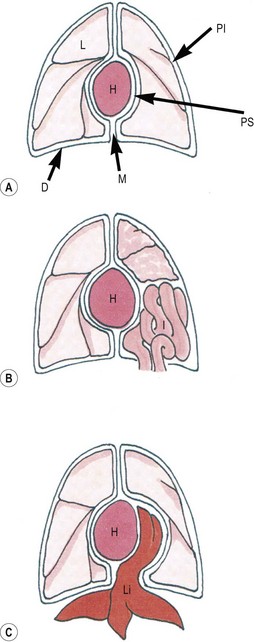
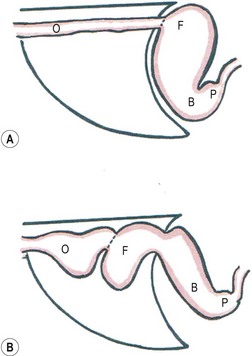
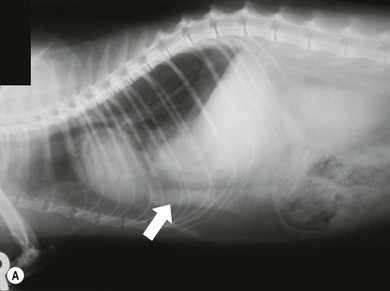
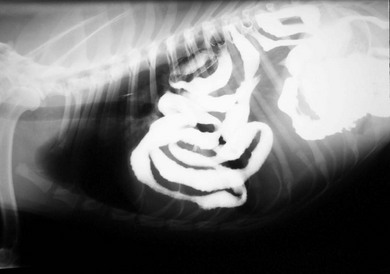
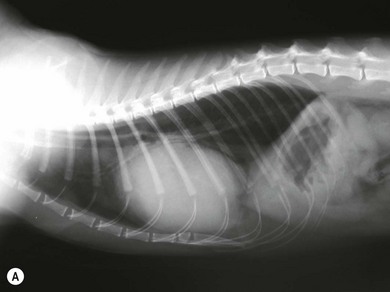
Chapter 45 The diaphragm is a musculotendinous sheet with a strong central tendon anchored to the costal arch and vertebrae by the sternal, costal, and lumbar muscles (Fig. 45-1).1,2 The paired lumbar muscles form the diaphragmatic crura that originate from the ventral aspect of the third and fourth lumbar vertebrae and run forward to form the central portion of the dorsal diaphragm.3 The paired costal and unpaired sternal muscles anchor the central tendon to the costal arch and xiphisternum.1,2 Figure 45-1 Diagram of diaphragmatic anatomy viewed from the abdominal (concave) surface with the animal positioned in dorsal recumbency (mimicking the presentation at surgery). CA, costal arch; CM, costal muscles (left and right); CT, central tendon; LC, left crus; RC, right crus; SM, sternal muscle (unpaired); V, 4th lumbar vertebra; X, xiphisternum. There are three apertures in the diaphragm.1,3 The caval foramen allows passage of the caudal vena cava. It is the most ventral aperture and is located in the central tendon to the right of midline.3 The esophageal hiatus is located on the midline dorsal to the caval foramen. The esophagus and paired vagal nerves pass through it.3 The aortic hiatus is the most dorsal aperture. It is located between the left and right diaphragmatic crura and is bordered dorsally by the lumbar vertebrae. The aorta, the azygous and hemiazygous veins, and the lumbar cistern of the thoracic duct pass through this.3 The splanchnic nerves and sympathetic chain also cross the diaphragm between the lateral part of each crus and the 13th rib.3 The phrenicoabdominal arteries (branches of the abdominal aorta) give rise to the phrenic arteries that divide across the base of the crura, run ventrally down the central tendon and supply the costal and sternal diaphragmatic muscles.4 These vessels anastomose with the intercostal arteries of the costal arch.4 The left and right phrenic nerves supply motor innervation to the diaphragm.2 There are several forms of diaphragmatic defect. Pleuroperitoneal defects are common and usually acquired following trauma. They allow communication of the pleural and peritoneal cavities (Fig. 45-2). Peritoneopericardial hernias (PPDHs) are uncommon congenital defects caused by failure of formation of the diaphragm and pericardium.5 They allow the pericardial and peritoneal spaces to communicate but the pleural cavities remain intact (Fig. 45-2). Sliding hiatal hernias occasionally develop, enabling cranial displacement of the terminal esophagus and gastric fundus through the esophageal hiatus into the mediastinum (Fig. 45-3). The severity of signs associated with these defects varies between individuals but surgery is generally indicated. Figure 45-2 Schematics of pleuroperitoneal and peritoneopericardial hernias (PPDHs). (A) Intact diaphragm and thoracic wall from dorsoventral projection. (B) Pleuroperitoneal hernia with intestinal herniation into the thorax. (C) PPDH with liver herniated into the pericardial sac causing cardiac displacement; note that the pleural cavities are intact. D, diaphragm; H, heart; I, intestine; L, lung; Li, liver; M, mediastinum; Pl, pleural cavity; PS, pericardial sac. Figure 45-3 Schematics of sliding hiatal hernia (lateral projection). (A) before herniation. (B) during herniation. The gastroesophageal junction and proximal fundus slide in and out of the mediastinum through the esophageal hiatus. Dotted line: gastroesophageal junction; B, gastric body; F, gastric fundus; O, esophagus; P, pylorus. A diagnosis of diaphragmatic disease is usually made from plain radiography or abdominal ultrasound but contrast radiography or CT is sometimes necessary. Loss of the diaphragmatic contour is found consistently in most cases but is not specific and can be associated with other pleural diseases such as pleural effusion. The presence of portions of the gastrointestinal tract within the thoracic cavity, recognized by luminal gas, ingesta or barium, is characteristic of the condition. Parenchymatous organs may also be delineated running forward from the abdomen into the thorax.6,7 The cardiac silhouette and lungs are often displaced cranially or dorsally.7,8 Pleural effusions can mask many of the characteristic radiographic features and repeating radiographic studies following thoracocentesis can help to resolve key features enabling a diagnosis to be confirmed.6 Congenital pleuroperitoneal hernias are thought to account for less than 10% of pleuroperitoneal defects in cats.9,10 There are only a handful of confirmed cases that have been classified as congenital because of the presence of a hernial sac11–15 or because of the early onset of signs.16 Congenital defects can affect most areas of the diaphragm with involvement of the central tendon,13,14 the sternal muscle,12 most of the left side of the diaphragm including the left crus16 and the right crus11,15 being reported. Liver and falciform fat are most commonly herniated, although two cases have contained the majority of the abdominal viscera.14,16 Some cats have presented with signs of dyspnea at an early age.11,16 Others have been diagnosed with congenital hernias as incidental findings during the investigation of unrelated diseases12,13,15 or during abdominal surgery14 and the oldest reported age at diagnosis was 11 years.13 In humans, congenital pleuroperitoneal hernias are thought to have a genetic basis.17 An autosomal recessive pattern of inheritance has also been proposed in dogs,18,19 although teratogens can induce diaphragmatic hernia formation in animal models.20 The etiopathogenesis of congenital pleuroperitoneal hernias in the cat is unknown but it is prudent to advise against breeding from affected animals. The majority of pleuroperitoneal defects (over 85%) are acquired traumatic ruptures.3,9 These are usually caused by blunt abdominal trauma and are associated with immediate herniation of abdominal organs because of the sudden increase in intra-abdominal pressure.21,22 Vehicular trauma is the commonest cause, but falls and dog attacks are also reported.23–25 Occasionally, diaphragmatic ruptures are caused by penetrating diaphragmatic injuries.23,24 In these cases, organs may not herniate immediately and the ruptures may only become clinically apparent some time after the initial injury. There is a single case report of an acquired pleuroperitoneal rupture associated with the collagen defect, cutaneous asthenia, in a cat.26 Most traumatic diaphragmatic ruptures are single tears through the sternal and costal muscles.3,27,28 Four percent of cases have multiple ruptures.3 Some ruptures involve the central tendon but the crura are very strong and rarely rupture.3,29 The most common rupture is a unilateral costal muscle tear in the ventral diaphragm below the level of the esophageal hiatus.3,27,28 Sixty percent of tears are circumferential with muscle tearing parallel to the rib or avulsing from it completely.28 Radial tears and combined radial and circumferential tears also occur.28 The liver is the most commonly herniated organ.3,10,28,30 The small intestine, stomach, spleen, omentum, and pancreas also frequently become herniated.3,10,30 Rarely, kidney, colon or cecum are involved.10,30–34 Right-sided hernias tend to contain liver, small intestines, and pancreas and left-sided hernias tend to contain stomach, spleen, and small intestine.28 Pleuroperitoneal defects usually lead to respiratory compromise due to compression of lung by herniated organs and poor diaphragmatic function.21,22,24,27,29 Pleural effusions may develop from transudation following venous congestion of herniated liver lobes and the effusion can contribute to the dyspnea.3,27,29 Ventilation-perfusion mismatches occur in the collapsed areas of lung22,29 and concurrent pulmonary contusion, pneumothorax, fractured ribs or flail chest may also contribute to respiratory compromise.27,29,35 In addition to dyspnea, injury of herniated organs may lead to clinical signs. Displaced, twisted liver lobes become congested, ischemic, and friable3,22 and displaced portions of the gastrointestinal tract may become obstructed or devitalized.29 Displacement or compression of the hepatobiliary tree has been associated with obstructive jaundice.36 Herniation of part or all of the stomach may lead to gastric dilatation and volvulus (GDV).37 This may cause obstructive shock, gastric necrosis, and severe respiratory compromise due to compression of lung by the dilated stomach.30 Rarely, perforation and rupture of organs lead to hemothorax, chylothorax or urothorax.28,31,32,38 Uterine herniation and bile leakage are reported in the dog but have not been reported in the cat to date.30,33,34,39–41 Forty-seven percent of cats diagnosed with diaphragmatic rupture have a history of witnessed trauma and most of the remainder have clinical findings suggestive of recent trauma.24 The diagnosis is usually reached within seven days of the original trauma. Almost one-quarter of patients have concurrent injuries including fractured ribs, fractured limbs or other external abdominal wall ruptures.24 In patients diagnosed within a few days of trauma, the commonest presenting signs are tachypnea and dyspnea.10,21,24,27,28,30 However, approximately 10% of patients have signs of gastrointestinal dysfunction such as vomiting and, in some of these cases, these are the only clinical signs of disease.24,28 Some patients do not develop signs immediately following trauma or have non-specific signs that delay investigation such as anorexia or lethargy.28 Patients in which the diagnosis is made several weeks following trauma are more likely to present with signs of gastrointestinal dysfunction (50% of cases) and dyspnea is less prevalent (38% of cases).42 Additional common clinical findings include muffled lung and heart sounds and hyporesonant thoracic percussion. Often, borborygmi can be heard in the thoracic cavity indicating herniation of portions of the gastrointestinal tract.10 Abdominal palpation may reveal a comparatively empty abdomen or apparent loss of key organs, such as the spleen, that have been displaced. Occasionally, pleuroperitoneal ruptures are identified as incidental findings with no overt clinical signs.42 The diagnosis of pleuroperitoneal rupture is usually confirmed using plain radiography or abdominal ultrasound but contrast radiography or CT is sometimes necessary.6,7,15,43,44 There are several key diagnostic radiographic features (Fig. 45-4). Loss of the diaphragmatic contour is found consistently in most cases but is not specific and can be associated with other pleural diseases such as pleural effusion.6,7 The presence of portions of the gastrointestinal tract within the thoracic cavity, recognized by luminal gas, ingesta or barium, is characteristic of the condition.6,7 Parenchymatous organs may also be delineated running forward from the abdomen into the thorax.6,7 The cardiac silhouette and lungs are often displaced cranially or dorsally.7,8 Pleural effusions can mask many of the characteristic radiographic features and repeating radiographic studies following thoracocentesis can help to resolve key features, enabling a diagnosis to be confirmed.6 Figure 45-4 Thoracic radiographs of cat with a pleuroperitoneal rupture. (A) Lateral view: the ventral diaphragmatic contour is obliterated. A parenchymatous organ (spleen) is seen traversing the diaphragmatic line into the thorax (arrow). (B) Dorsoventral view: the left diaphragmatic contour is obliterated, there is left-sided pleural effusion and the heart is displaced towards the right. (With kind permission of the Image Archives of R(D)SVS, University of Edinburgh.) Indicators of diaphragmatic rupture may also be seen on abdominal radiographs. Cranial displacement of the gastric axis is associated with liver herniation (see Fig. 45-6A).7 Gastrointestinal contrast studies delineate fluid-filled intestinal loops within the thorax although these are usually not required to confirm a diagnosis (Fig. 45-5).6,7 Positive contrast peritoneography is a more definitive test of diaphragmatic integrity (Box 45-1).6,15 Figure 45-5 Thoracic radiograph of a cat with a pleuroperitoneal rupture following an upper gastrointestinal contrast study: contrast delineates the lumen of intestinal loops within the thorax. The diaphragm is difficult to visualize with ultrasound unless abdominal or pleural fluid is present but transhepatic and intercostal ultrasound can be used to identify herniated organs within the thorax.44 It is important to distinguish herniated liver lobe from consolidated lung and from mirror artifact.44,45 PPDH is considered to be a congenital condition in the cat although rare examples of traumatic PPDH are described in humans.46–48 During normal development, the pericardial cavity separates from the common pleuroperitoneal cavity before the pleural and peritoneal cavities separate. If these two processes fail during development,5 the pericardium and ventral diaphragm fuse to form a stoma in the central diaphragm immediately dorsal to the xiphisternum. In some cases, the caudal sternebrae and cranial linea alba may also be malformed producing concurrent ventral body wall hernias, sternal defects or pectus excavatum.46,48,49 PPDH may remain clinically silent for some time before causing clinical signs and the median age at diagnosis is over four years.46 Respiratory and gastrointestinal dysfunction are reported with equal frequency.46,47 Rarely, cardiac tamponade develops due to the presence of large volumes of herniated organs or the development of intrapericardial cysts from incarcerated hepatobiliary tissue, omentum or falciform fat.50–52 Forty percent of cases have no clinical signs, with PPDH diagnosed as an incidental finding.46,47,49 PPDH shares many of the clinical features of pleuroperitoneal hernias including muffling and displacement of the cardiac apex beat, dyspnea, and thoracic borborygmi.46,47,49 Concurrent cranial ventral abdominal wall hernias (located cranial to the umbilicus) or sternal defects are occasionally palpable and increase suspicion of PPDH.47,49 Rarely, signs of cardiac tamponade occur (open-mouth breathing, lethargy, weak femoral pulses, distended jugular veins, tachycardia).50–52 The key radiographic differences that distinguish PPDH from pleuroperitoneal defects are that the herniated organs are centered around the heart causing mediastinal widening and that the diaphragmatic contour is preserved on ventrodorsal views bilaterally although the cupula of the diaphragm is effaced (Fig. 45-6).6 PPDH may be mistaken for generalized cardiomegaly or pericardial effusion radiographically but cardiac ultrasound can distinguish between these conditions. Figure 45-6 Thoracic radiographs of a cat with a PPDH. (A) Lateral view: the cardiac silhouette appears enlarged giving the impression of cardiomegaly. The cupula of the diaphragm is effaced by soft tissue and there is increased contact between the diaphragm and pericardium. Forward displacement of the gastric axis due to liver herniation can also be seen (apparent microhepatica). (B) Dorsoventral view: the cupula of the diaphragm is effaced by soft tissue (arrowheads) but the diaphragmatic line is otherwise intact, distinguishing PPDH from pleuroperitoneal hernia (compare to Figure 45-4B). (With kind permission of the Image Archives of R(D)SVS, University of Edinburgh.)
Diaphragm
Surgical anatomy
Diagnosis and general considerations
Diagnostic imaging
Surgical diseases
Congenital pleuroperitoneal hernias
Acquired pleuroperitoneal ruptures

Congenital peritoneopericardial hernia

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Diaphragm
