Chapter 51Diagnosis and Management of Sacroiliac Joint Injuries
Anatomical and Functional Features
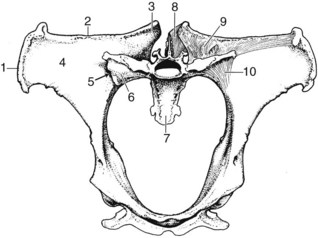
The sacroiliac joint is a synovial articulation located at the junction between the ventral aspect of the wing of the ilium and the dorsal aspect of the wing of the sacrum (Figure 51-1). The sacroiliac joint functions in pelvic attachment to the axial skeleton, providing support during weight bearing and helping to transfer propulsive forces of the hindlimb to the vertebral column. The sacroiliac joint is an atypical synovial articulation because of hyaline cartilage on the sacral articular surface and a thin layer of fibrocartilage on the ilial articular surface.1 The articular surfaces of the sacroiliac joint are nearly flat and closely apposed to support gliding movements. The sacroiliac articular surfaces diverge cranially at about 40 degrees from a transverse plane and are angled craniodorsally to caudoventrally at about 60 degrees from the horizontal plane. The joint capsule is thin and closely follows the margins of the sacroiliac articular cartilage. The sacroiliac joint capsule is reinforced ventrally by the ventral sacroiliac ligament.2 A small amount (<1 mL) of synovial fluid is normally present in the joint.1 Because of articular surface remodeling, the size and shape of the sacroiliac joint margins vary considerably according to age and body weight.3 Typically the sacroiliac joint outline is L-shaped, with the convex border directed caudoventrally.
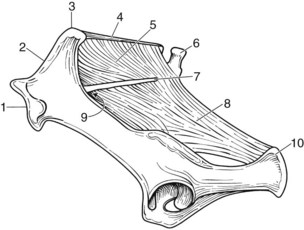
The pelvis is firmly attached to the axial skeleton by sacroiliac and sacrosciatic ligaments, which form a strong ligamentous sling (see Figure 51-1). The weight of the caudal aspect of the vertebral column is suspended from the sacroiliac ligaments, which function similarly to the fibromuscular sling found between the proximal aspect of the forelimb and the lateral thoracic body wall. Subsequently the sacroiliac articular cartilage may never be fully weight bearing, unlike most articular cartilage. The sacroiliac joint is supported by three pairs of strong ligaments: the dorsal, interosseous, and ventral sacroiliac ligaments. The dorsal sacroiliac ligament consists of dorsal and lateral portions (Figure 51-2). The dorsal portions form two round cords that span from the dorsal aspects of the tubera sacrale to the dorsal apices of the sacral spinous processes. The lateral portion forms a sheet of connective tissue that spans from the caudal margin of each tuber sacrale and iliac wing to the lateral border of the sacrum. The lateral portion of the sacroiliac ligament is continuous ventrally with the sacrosciatic ligament. The interosseous ligament of the sacroiliac joint is robust and consists of a series of vertical fibers that connect the ventral aspect of the wing of the ilium to the dorsal aspect of the wing of the sacrum (see Figure 51-1). The interosseous sacroiliac ligament provides the major resistance to vertically oriented weight-bearing forces acting on the sacrum. The ventral sacroiliac ligament interconnects the ventral aspects of the wings of the ilium and sacrum. The ventral sacroiliac ligament is thin and closely applied to the ventral margins of the sacroiliac joint capsule.
Neurovascular structures adjacent to the sacroiliac joint include the sciatic nerve, cranial gluteal nerve, and cranial gluteal artery and vein. These structures collectively travel through the greater sciatic foramen, ventromedial to the sacroiliac articulation (see Figure 51-2). The cranial gluteal artery and vein arise from the internal iliac vessels and travel over the ventral sacroiliac ligament and the caudomedial aspect of the sacroiliac joint before emerging at the greater sciatic foramen. The cranial gluteal artery and vein continue dorsally into the gluteal musculature. The middle and accessory gluteal muscles originate from the dorsal aspect of the ilial wing and have attachments near the caudomedial aspect of the sacroiliac joint. Within the pelvic canal, a portion of the internal obturator and iliacus muscles covers the ventral sacroiliac joint margins.
Pathological Conditions
OA of the sacroiliac joints is usually a bilateral condition and may be present despite symmetry of the tubera sacrale.19 Degenerative changes of the sacroiliac joint include (in apparent order of increasing severity) articular surface lipping, cortical buttressing, articular recession, osteophytes, and intraarticular erosions (Figure 51-3). In our survey of 36 TB racehorses, sacroiliac degenerative changes were classified as mild in 8% of specimens, moderate in 61%, and severe in 31%. Age was not associated with overall prevalence or severity of sacroiliac joint degenerative changes.17 Osseous changes are usually bilaterally symmetrical and most commonly located at the caudomedial aspect of the articulation.1,17 The pathogenesis of proliferative sacroiliac joint changes is uncertain, but it is thought to be related to chronic instability resulting in gradual remodeling and subsequent enlargement of the caudomedial joint surfaces. Histologically the caudomedial extensions consist of apparently normal cancellous bone.4 Articular cartilage erosion is a lytic process of articular surfaces that presumably leads to eventual sacroiliac joint ankylosis.17 However, ankylosis of the sacroiliac joint is rare, which is surprising based on the limited joint motion and the potential severity of osseous pathological conditions present.1,17,20 Fibrous interconnections between the articular surfaces have also been reported in presumed normal sacroiliac joints.1 Articular cartilage discoloration, a presumed indicator of sacroiliac joint degeneration, is common in racehorses, but it has a reported higher prevalence in Standardbreds (STBs) compared with TBs.14 One theory is that these changes are caused by differences in pelvic and sacroiliac joint biomechanics associated with pacing and trotting (i.e., lateral bending or shear forces) in STBs compared with galloping (i.e., flexion and extension movements) in TBs.21 Biomechanical studies are warranted to support or refute these claims.
Complete sacroiliac ligament disruption is most likely caused by substantial trauma, such as flipping over backward, or catastrophic musculoskeletal injuries associated with race training.17 Post mortem findings associated with traumatic sacroiliac ligament injuries include either unilateral or bilateral joint capsule disruption, avulsion fractures of the sacroiliac ligament attachment sites, and noticeable sacroiliac joint laxity. Dorsal or ventral sacroiliac ligaments can be affected, depending on the inciting mechanism of injury.9,17,23 Complete sacroiliac ligament disruption may produce unilateral or bilateral dorsal displacement of the tubera sacrale, depending on the extent of injury (Figure 51-4).
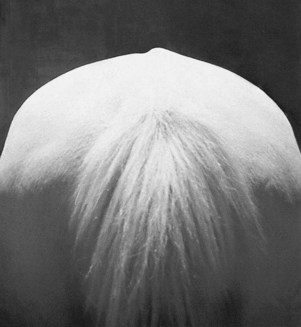
The pathogenesis of apparent spontaneous or insidious differences in tuber sacrale height needs to be further researched.4 Unilateral or bilateral dorsal displacement of the tubera sacrale is often a presumed indication of sacroiliac subluxation.25 In my opinion, variable degrees of tubera sacrale height asymmetry occur frequently and may be caused by chronic asymmetric muscular or ligamentous forces acting on the malleable osseous pelvis and not by direct sacroiliac ligament injury.26 Tubera sacrale height asymmetries are common in horses without documented sacroiliac joint injuries (see Figure 51-4). In only a few horses have tubera sacrale height asymmetries been associated with chronic sacroiliac ligament injuries or joint laxity.24 In a study of 4-year-old STB trotters with tubera sacrale height asymmetries of more than 1 cm, associations were found with poor performance, but otherwise the asymmetry was of questionable clinical importance.16 If substantial tubera sacrale height differences are identified, which side is affected is unclear and difficult to determine: the seemingly dorsally displaced tuber sacrale or the less prominent tuber sacrale on the opposite side.4,16 Presumed sacroiliac joint subluxation produces an elevated tuber sacrale on the affected side, whereas complete ilial wing fractures (the most common type of pelvic fracture) typically produce a palpably depressed tuber sacrale on the affected side.27
Clinical Presentation
Horses with sacroiliac joint injuries vary in clinical presentation, usually based on the duration and extent of injury present. The history of horses with acute sacroiliac joint injury usually includes slipping, falling, or trauma that causes pelvic rotation or induces high stresses.25 Horses with acute sacroiliac joint injuries often have noticeable lameness and localized sensitivity to palpation of the surrounding soft tissues or tubera sacrale (Figure 51-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree