Chapter 56Diagnosis and Management of Osteochondrosis and Osseous Cystlike Lesions
The pathogenesis of osteochondrosis (OC), palmar or plantar osteochondral fragments of the proximal phalanx, ununited palmar or plantar eminences of the proximal phalanx, subchondral bone cysts, and other osseous cystlike lesions is discussed in Chapters 36, 42, and 54. In this book the term subchondral bone cyst is used for large radiolucent areas in the subchondral bone of the medial femoral condyle; these cysts have a consistent pathological structure with a true cellular cyst lining. Osseous cystlike lesions in other locations vary more in structure. This chapter discusses the diagnosis and management of these lesions and other osseous fragments believed to be at least predominantly developmental in origin. The joints most commonly affected include the hock, stifle, fetlock, and shoulder. It is common for matching joints to have lesions but much less common to find OC lesions in different joints. This is consistent with the concept of such lesions occurring during some finite window of vulnerability during development that is specific for a given anatomical location.
Lesions in the Metacarpophalangeal and Metatarsophalangeal Joints
Osteochondritis Dissecans of the Sagittal Ridge of the Third Metacarpal and Metatarsal Bones
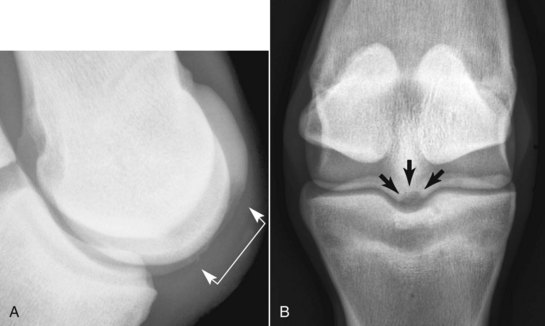
Lesions are more common in the MtIII than in the McIII, but all fetlocks should be examined radiologically if a lesion is recognized in one, using perfectly exposed (or slightly underexposed) flexed lateromedial images (Figure 56-1). Lesions on the dorsoproximal aspect of the sagittal ridge are easiest to recognize, but lesions may occur farther distally or, less commonly, on the palmar or plantar aspect of the sagittal ridge. The latter can also be seen radiologically on the dorsopalmar (plantar) image. The larger fragments extend abaxially along the proximal margin of the articular cartilage under the dorsal synovial fold.
Osseous Cystlike Lesions
Osseous cystlike lesions occur on the weight-bearing surface of the condyles of the McIII and the MtIII. Most occur in the medial condyle and are diagnosed in horses 1 to 2 years of age. The lesions are easy to recognize radiologically (Figure 56-2) and result in obvious lameness, exacerbated by distal limb flexion. Lameness is improved by perineural or intraarticular analgesia. Lameness associated with an osseous cystlike lesion sometimes occurs in foals. At the time of onset of lameness no lesion may be identifiable radiologically, or only a subtle defect in the outline of the subchondral bone may be apparent. However, sequential radiographs obtained over the following 6 to 8 weeks may reveal development of an osseous cystlike lesion. Surgical debridement may be successful,1 but corticosteroids administered intraarticularly or intralesionally also may result in clinically significant improvement in young horses. Although simple debridement of the McIII and the MtIII osseous cystlike lesions has been reasonably successful, the intensity of loading on the distal aspect of the McIII and the MtIII in athletic horses makes horses with these lesions good candidates for advanced joint resurfacing techniques.
Palmar or Plantar Osteochondral Fragments of the Proximal Phalanx
Osteochondral fragments arising from the proximal palmar or plantar aspect of the proximal phalanx are common radiological findings in WBLs, STBs, and TBs, especially in the hindlimbs. Palmar or plantar osteochondral fragments and ununited palmar or plantar eminences may not cause clinical signs or merely cause mild discomfort at high levels of performance. Assessment of clinical importance and management are discussed in detail in Chapters 36 and 42.