Chapter 9 Dermatologic Diseases
Anatomy, Physiology, and Husbandry Considerations
The skin of ferrets contains numerous sebaceous glands. Secretions of these glands sometimes cause the hair coat to have a greasy feel and a characteristic musky odor. Intact and sexually mature males and females have larger sebaceous glands than neutered ferrets,25 and glandular production appears to be under androgenic control. Secretions may be so profuse that intact male albino ferrets can appear yellow and dirty. Frequent bathing can remove essentials oils from the skin and result in pruritus and keratinopathies. Ferrets are quite fastidious animals, and routine bathing is not necessary.
Ferrets have epitrichial (apocrine) sweat glands on the body and atrichial (eccrine) sweat glands on the footpads.25 They are predisposed to hyperthermia when exposed to high ambient temperatures.
Normal ferret skin has a compound hair follicle arrangement composed of one primary hair and a collection of secondary hairs, the latter increasing in number with the ferret’s age until maturity.25 Ferrets have a thick cream-colored undercoat with coarse guard hairs that define the hair-coat color. The color of the undercoat remains the same, but the guard hair color can change at different times during the ferret’s life, as can the facial mask.3 The hair coat may become lighter as the ferret ages. Molting, which usually occurs twice a year, appears to be controlled by hormones responsive to changes in the photoperiod; thus estrogens cause hair and weight loss in ferrets.15 During the breeding season (March through August in the northern hemisphere), intact males increase sebaceous secretions in response to elevated hormone levels; the result can be an increased musky odor, oily fur, and a yellowish undercoat (see Chapter 1). In both intact and neutered ferrets, the hair coat normally thins in response to an increase in the number of daylight hours and in the ambient temperature (simultaneously with the breeding season)—that is, in the late spring in the northern hemisphere.15 This molt may result in bilaterally symmetric alopecia of the tail, perineum, and inguinal area, or the ferret may lose most of the guard hairs and appear “fluffy.” The spring molt is often more marked in females than in males and is usually more pronounced in intact ferrets. In the late fall, a less pronounced molt occurs coincident with an increase in density of the light-colored undercoat. As a result, the hair coat appears lighter during the fall and winter seasons. As the hair thins, red-brown waxy deposits, often sebaceous secretions, may be visible on the skin. Hair that is shaved during seasonal hair loss may not regrow for several weeks or months. Hair regrowth, such as occurs after shaving for surgery or after treatment of adrenal gland disease, sometimes imparts a bluish appearance to the skin, which may be mistaken for bruising or cyanosis.3 This apparent discoloration resolves as soon as hairs erupt from the skin. Both sexes accumulate subcutaneous fat beginning with the fall molt and resolving in the spring. As a result, body weight can fluctuate by 30% to 40%.15
The ideal ferret diet is rich in fat and animal protein and low in carbohydrate and fiber. Ferrets should be fed high-quality ferret, cat, or kitten food (see Chapter 1). If dietary requirements are not met, the hair coat can become dry and dull. The provision of a suitable diet, with or without short-term administration of a fat supplement, usually corrects this problem. In addition to inadequate levels of protein or fat, biotin deficiency can cause abnormalities in the hair coat. Avidin, an enzyme found in raw egg white, binds biotin and has been reported to cause bilaterally symmetric alopecia in ferrets fed diets containing more than 20% raw eggs.21 Feeding raw eggs to ferrets is not recommended.
Wild ferrets spend considerable time in underground dens with high humidity. Pet ferrets housed in dry environments (e.g., homes that are heated in the winter) may scratch or have flaky skin. The use of a cool-air humidifier or application of an emollient skin spray has been recommended in these cases.3 Exposure to clay kitty litter can also dry a ferret’s coat and should be avoided.3
Certain skin or hair problems in ferrets result from self-mutilation or trauma. Ferrets need privacy and should be provided with hide boxes or artificial burrows. A ferret with inadequate bedding, nesting, or hiding spots may rub its face on the floor in an attempt to hide and subsequently cause facial abrasions. Broken hair shafts can resemble those seen with dermatomycoses. Intact females may pull hair from themselves to use as bedding material.15 Ferrets can be quite rough during mating and playing and can inflict scratches and bite wounds.
Diseases
Ectoparasites
Fleas
Flea infestation is occasionally seen in ferrets. As with dogs and cats, Ctenocephalides species are usually involved,14 but infestations with Pulex irritans (the human flea), Paracaras meli (the badger flea), Ceratophyllus sciurorum (the squirrel flea), and Ceratopyllus vison (the mink flea) have also been reported, depending on the environment.4,44 Fleas are transmitted by direct contact with another animal or a flea-infested environment. Although some ferrets are asymptomatic, clinical signs generally include mild to intense pruritus, development of erythemic papules, and alopecia most often noted on the dorsal cervical and interscapular areas.47 Ferrets can less commonly develop signs of flea-bite hypersensitivity, including pruritic papulocrustous dermatitis over the tail base, ventral abdomen, or caudomedial thighs.14
Identifying fleas or flea excrement on the animal confirms the diagnosis. Treat the ferret as well as other animals in the household, and treat the environment concurrently. None of the treatments discussed below have been approved by the U.S. Department of Agriculture for use in ferrets. Traditional treatments include flea shampoos, dips, or powders containing pyrethrins, lindane, or carbamates;14 however, toxic reactions occasionally occur with some of these chemicals. Pyrethrins are among the least toxic.4 Organophosphates (malathion, ronnel, fenthion, cythionate, dichlorovos, neguvon) can be highly toxic in ferrets and are not recommended for topical use in this species.4 In addition to the risk of toxicity, dichlorvos-impregnated flea collars can get caught on objects in the environment. Because of the ferret’s small body size, caution is advisable in applying any topical medication. When using sprays, first spray a cloth and then rub the cloth on the ferret. Ferrets can ingest sprays and powders while grooming. Extreme care is advised in the use of pesticide dips; some dips can be toxic with prolonged exposure, and ferrets need to be dried and kept moderately warm after dips.
Although newer products developed for flea control in dogs and cats have not been approved for use in ferrets, anecdotal reports of toxicity are uncommon.4 We prefer the use of these products for flea control in ferrets in our practice. Imidacloprid is a flea adulticide that kills on contact and has larvacidal activity in the environment.4,14 Topical imidacloprid (Advantage 40 for Cats, Bayer Corp., Shawnee Mission, KS) applied at a dose of 0.4 mL. 10% on the skin at the base of the skull was well tolerated in ferrets and was effective in eliminating an established flea population as well as in dealing with a subsequent flea challenge for 3 weeks.9 In conjunction with environmental control, one application of imidacloprid might be sufficient to control a flea problem. Similarly, application of 0.4 mL imidacloprid 10%/moxidectin 1% spot-on (Advocate/Advantage Multi, Bayer Corp., Shawnee Mission, KS) on the interscapular skin in ferrets with established flea infestations resulted in a therapeutic efficacy of 100% on day 1 after treatment and a preventative efficacy of >90% for up to 30 days after treatment.44 Lufenuron (Program, Novartis Animal Health, Greensboro, NC), an insect growth regulator, kills immature fleas by interfering with chitin production. Because there is a lag time of approximately 6 to 8 weeks from the beginning of treatment with lufenuron and reduced numbers of adult fleas on the ferret, an adulticide may have to be used concurrently until the flea population in the environment has been controlled.4 A dosage of 45 mg lufenuron (half of a cat dose) given orally once a month has been used in ferrets.4 Rare side effects may include vomiting, lethargy, diarrhea, pruritus, or inappetance. Fipronil (Frontline, Merial Ltd., Duluth, GA) is a flea adulticide that also kills ticks. Topical application of a half to a full cat dose has been reported anecdotally in ferrets.4 Although the toxic action of fipronil is very specific to invertebrates and as such is not expected to affect mammals, the incidence of adverse reactions in a large population of ferrets is unknown.4 Either imidacloprid or fipronil can be used in conjunction with lufenuron. Selamectin (Revolution or Stronghold, Pfizer, New York, NY) is a semisynthetic avermectin that is approved for use in dogs and cats to control fleas, heartworms, ear mites, and sarcoptic mange mites. In a clinical trial, doses of either 6 or 18 mg/kg used monthly in ferrets for 4 months were 100% effective in preventing flea infestations for 7 to 21 days posttreatment.8 Treatment of the environment is the same as that in households with dogs and cats. Residual chemicals (e.g., microencapsulated formulas of pyrethrins with synergists and diazinon) or methoprene (insect growth retardant preventing fourth instar larval metamorphosis) have been recommended.14 Potentially less toxic forms of treatment that will also destroy parasites are steam cleaning of carpeting and the application of boric acid salts to the floor or carpet. These procedures will desiccate and destroy flea adults and larvae.4 Pets and humans should be prevented from coming in contact with any chemicals applied to the environment.
Mites
Ear Mites
The same ear mite that affects dogs and cats (Otodectes cynotis) affects ferrets.14 The mite is transmitted by direct contact with other infested animals. Ferrets may shake their heads or scratch their ears, but they are more commonly asymptomatic. Clinical lesions vary from inflammation of the external ear canal with accompanying mild pruritus to severe pruritus with excoriations and crusting. Dark brown waxy aural debris is often present; however, this can also be seen in some normal ferrets. The mite is identified by microscopic examination of the aural debris. Although ear mites can reportedly colonize other parts of the body, specifically the perineum,5 this rarely occurs.
To eliminate ear mites, all susceptible animals in the household should be treated. Gently clean the ears before any treatment, but avoid solutions that can damage the middle ear if the tympanic membrane is ruptured. Selamectin applied topically at a dose of 45 mg in the dorsal interscapular area approximately every 30 days was reported to be safe and efficacious for the treatment of ear mite infestation in ferrets.28 One of the authors (CO) commonly uses selamectin for the treatment of ear mites in ferrets. Another commonly used treatment protocol is ivermectin injected subcutaneously at a dose of 0.2 to 0.4 mg/kg and repeated every 2 weeks for three treatments. Although this protocol is often successful, some mite infestations are now refractory to treatment. Aural topical treatments have alternatively been reported to be safe and efficacious in ferrets. In a study that compared three protocols for treating ear mites in ferrets (parenteral ivermectin, aural topical administration of ivermectin, and aural topical administration of an otic preparation of thiabendazole, dexamethasone, and neomycin [Tresaderm, Merck Agvet, Rahway, NJ]), results showed that treatment with either the thiabendazole product (2 drops in each ear canal q24h for 7 days, untreated for the next 7 days, then treatment reinstituted for 7 days) or topical ivermectin (1% ivermectin diluted 1:10 in propylene glycol; 0.4 mg/kg divided between each ear canal, then repeated 2 weeks later) was more effective in eliminating mites than parenteral treatment with ivermectin (1% ivermectin diluted 1:4 in propylene glycol; 0.4 mg/kg SC).34 To avoid toxicity, it is recommended not to treat with topical and parenteral ivermectin concurrently. Extra care is advised in treating pregnant animals with ivermectin, because high doses administered to pregnant jills have resulted in an increased rate of congenital defects in kits.14 Thiabendazole is expected to have a wider margin of safety in pregnant animals.34 Topical otic treatments used alone can fail for several reasons: the ear canal may be too narrow for the medications to penetrate, the ferret may resist treatment, or mites may be present on other areas of the body left untreated.14 Some clinicians have recommended treating the entire body with flea powder.14 The entire environment, including bedding, should be thoroughly cleaned as part of any treatment protocol.
Sarcoptic Mange
Two different clinical syndromes are seen in ferrets with sarcoptic mange. In the generalized form, clinical signs include focal to generalized alopecia with intense pruritus.14 The localized form of the disease, in which only the feet are affected, is seen occasionally. The paws become inflamed, swollen, and crusted and can be very pruritic. In severe cases, the nails may become deformed or even slough. The layman’s term for this form of the disease is foot rot.14
Traditionally recommended treatment has been ivermectin injected subcutaneously at a dosage of 0.2 to 0.4 mg/kg every 14 days for three treatments.26 Alternative treatment recommendations have included dipping the ferret once weekly in 2% lime sulfur until 2 weeks after the signs resolve,42 but this agent has a strong odor and will discolor the fur. Treatment with either the same imidacloprid/moxidectin formulation mentioned above (Advocate/Advantage Multi Bayer Corp., Shawnee Mission, KS) or selamectin was reported to be highly effective against Sarcoptes scabiei in dogs,11 and although its use is off-label in ferrets, its use carries low risk.
Demodectic Mange
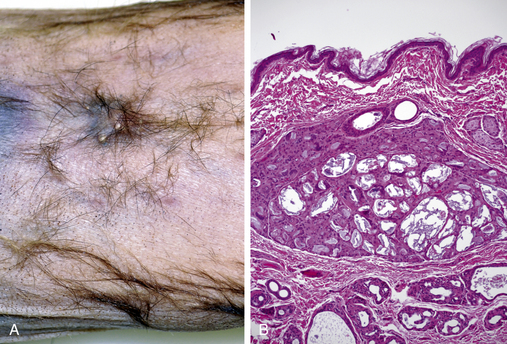
A histopathologic study on the skin of normal ferrets found Demodex species within the hair follicles and sebaceous glands in the perianal, vulvar, preputial, facial, and caudal abdominal regions in 9 of 25 ferrets aged 4 to 32 months.25 However, clinical demodicosis has rarely been reported in ferrets. In dogs and cats, adult-onset demodectic mange has been associated with immunosuppression. Demodicosis has been reported in ferrets with adrenal disease and systemic lymphoma1 as well as subsequent to prolonged treatment with corticosteroids.32 Clinical signs of demodicosis can include alopecia, skin thickening, and/or discoloration, erythema, and pruritus affecting the ears, face, ventral abdomen, inguinal area, or tail. A brown ceruminous exudate is commonly seen in the otic canals. One of the authors (CO) has seen a persistent Demodex infestation in the otic canals of three geriatric ferrets from the same household, all of which had received ivermectin for several years for heartworm prophylaxis (55 μg orally once monthly) (Heartgard Plus for Cats, Merial, Duluth, GA). All ferrets had histories of adrenal disease and prolonged treatment with prednisone for presumptive insulinoma or inflammatory bowel disease. One male neutered ferret had several small plaques in the skin surrounding the prepuce, histopathologic exam of which revealed multiple cystic apocrine glands. Many of the glands contained cross sections of mites with an elongate morphology consistent with Demodex species. Several mites free within the superficial dermis appeared to have incited a granulomatous reaction (Fig. 9-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree