Chapter 18 Dermatologic Diseases
Bacterial Infections
Subcutaneous Abscesses
Subcutaneous abscesses commonly occur in rabbits from traumatic wounds or bacteremia secondary to tooth root infection, oral foreign bodies, or upper respiratory tract or urinary tract infections. Frequently, no direct cause is identifiable.22,27,28,33 Abscesses usually are soft to firm swellings that gradually enlarge over days to weeks. Although abscesses most commonly develop on the head and limbs, they may occur anywhere on the body (Fig. 18-1). They usually are not painful, are frequently immovable, are minimally inflamed, contain caseous exudate, and are typically walled off by a thick capsule.19 Abscesses may be confined to the subcutaneous space, or they may extend to underlying dermis and bone. Facial abscesses are often associated with underlying dental or nasolacrimal duct disease. Periapical abscesses are common and are typically associated with elongated cheek teeth roots. Superficial abscesses may occur as a result of fight wounds or penetrating injuries. Affected rabbits may have no other clinical signs, or they may be inappetant, lose weight, drool (with oral abscesses), or become lame (with limb abscesses).
Diagnose subcutaneous abscesses by palpation and oral examination. Aspirate subcutaneous swellings with a 22-gauge or larger needle to obtain samples for cytologic evaluation, Gram’s stain, and both aerobic and anaerobic bacterial culture and sensitivity testing.27,28 Organisms most commonly isolated from rabbit abscesses include Staphylococcus aureus, Pasteurella multocida, Pseudomonas aeruginosa, Proteus species, Fusobacteria species, Bacteroides species, and Actinomyces species.19,20,32,41,58 Samples for bacterial culture and sensitivity testing are always recommended for recurrent abscesses because bacteria can become resistant to antibiotics.22 Despite the presence of bacteria within abscesses, cultures of abscess aspirates are sometimes negative for bacterial growth. Swabs taken from the inner lining of an abscess cavity are less likely to yield negative bacterial culture results than those taken from the purulent contents. Negative growth on aerobic culture may also occur if the primary pathogen is an anaerobic bacterial species. In addition to bacterial cultures, obtain radiographs to determine if the underlying bone is affected. For abscesses on the head, both thoracic and skull radiographs should be obtained because thoracic radiographs can reveal pneumonia or pulmonary abscessation. Ultrasonography and computed tomography may help delineate abscess margins and are especially useful with retrobulbar abscesses (see Chapter 35). A blood sample for a complete blood count (CBC) and plasma biochemical analysis and a urine sample for urinalysis are all indicated in the diagnostic workup of patients with subcutaneous abscesses.
Treatment depends on the location and extent of the abscess. Complete surgical excision of the abscess en bloc, followed by at least 2 weeks of antibiotic administration based on results of culture and sensitivity testing, is ideal.* If joints are affected, limb amputation may be necessary. With retrobulbar abscesses, enucleation may be warranted (see Chapter 33). All inciting causes, such as foreign bodies or dental disease, should be addressed to minimize the recurrence of the abscess. If en bloc excision including the abscess capsule is not possible, debride all infected soft tissue and bone. Because the purulent content is usually thick, rabbit abscesses cannot be treated effectively with drains. If any infected tissue remains after abscess debridement, recurrence is likely because antibiotics do not penetrate either the thick capsule or its caseous contents easily. If complete excision is impossible, abscessed tissue should be debrided, flushed with sterile saline solution twice a day, and the remaining pocket allowed to heal by second intention. Any part of the capsule that can be removed should be removed to minimize contamination of unaffected tissue with infected material.
Abscesses have been successfully treated by packing the completely debrided abscess cavity with antibiotic-impregnated polymethylmethacrylate beads (PMMA), bone cement, or a synthetic polymer.16,19,33,41 Beads slowly release antibiotics over days to weeks, providing high local tissue concentrations of drugs with low systemic levels and few systemic side effects (see Chapter 32). Commonly used heat-stable antibiotics in beads include cephalothin (2 g/20 g PMMA), cefazolin (2 g/20 g PMMA), amikacin (1.25 g/20 g PMMA), gentamicin (1 g/20 g PMMA), and tobramycin (1 g/20 g PMMA).74 While rabbits should not be given most cephalosporins orally owing to the risk of developing fatal enterotoxemia, they generally tolerate these drugs in beads because of the slow release and localized concentration.16,19 Be careful not to place beads in abscess pockets that communicate with the oral cavity, or rabbits may ingest them. Beads may be left in place for weeks and removed at a subsequent surgery. Beads may be left intact permanently, but they may eventually act as a nidus for further abscess formation and have to be removed later. Large abscesses may require multiple surgeries to treat. If contaminated abscess cavities must be temporarily closed to retain packed beads, use only nonabsorbable monofilament sutures because they are less likely to induce an intense tissue response than absorbable or multifilament suture. Close uncontaminated wounds with absorbable monofilament suture.
Older references mention the application of calcium hydroxide powder to abscess pockets after debridement to alkalinize the local wound environment and limit bacterial growth. Calcium hydroxide powder is no longer recommended owing to the severe soft tissue necrosis it can induce.16,19
Some authors advocate application of honey or 50% dextrose solution with or without topical antibiotics to the abscess cavity after debridement.16,74 This hyperosmotic solution may dry out the affected area, provide antibacterial effects through acidification of local tissue, and stimulate wound healing. It may also encourage the rabbit to lick the area and thus promote drainage.
Jaw abscesses are particularly difficult to treat. These abscesses may result from periapical disease causing abnormal tooth growth and destruction of surrounding bone.58 Dental abscesses often fistulate through underlying tissue to teeth roots. Bacteria commonly isolated from these abscesses are Fusobacterium, Prevotella, Peptostreptococcus, Actinomyces, and Arcanobacterium species.19,67,68 To treat dental abscesses, curette and flush necrotic tissue (including infected bone), extract infected teeth, and pack the remaining pocket with antibiotic-impregnated PMMA beads or a synthetic bone graft particulate (Consil, Nutramax Laboratories, Baltimore, MD) (see Chapter 32). Alternatively, marsupialize the debrided abscess pocket open to surrounding skin to allow daily flushing until a clean wound pocket is achieved. In addition, CO2 laser ablation has been used successfully in cases of recurrent mandibular abscessation.19
Regardless of how the wound is treated, choose systemic antibiotic therapy based on results of culture and sensitivity testing and administer antibiotics postoperatively for at least 2 weeks and up to 6 weeks or longer. While cultures are pending, administer a penicillin G benzathine/penicillin G procaine combination at a dosage of 75,000 U SC every other day for rabbits weighing less than 2.5 kg and 150,000 U SC every other day for rabbits weighing more than 2.5 kg.61 Combination treatment with enrofloxacin (5 mg/kg PO q12h) and metronidazole (30 mg/kg PO q12h) also provides broad-spectrum treatment until culture results are obtained.74 For rabbits with recurrent abscesses, lifelong antibiotic treatment and repeated surgeries may be necessary.28 The long-term prognosis for rabbits with abscesses is improved with proper husbandry, including good sanitation and a high-fiber diet.27
Mastitis
Rabbit mastitis is most common in heavily lactating does.28,41 It may be caused by trauma to the teats with secondary bacterial infection from environmental contamination. The most commonly isolated organism in rabbits with suppurative mastitis is coagulase-positive Staphyloccus aureus. Other bacteria that cause mastitis include Pasteurella and Streptococcus species. Mammary glands are typically swollen, indurated, and sometimes abscessed. Teats initially are pink from hyperemia and then turn blue from vascular stasis (hence the term, blue breast).19 Does become depressed, anorectic, septicemic, and febrile; they often die. Rabbits with mastitis should be treated with intravenous fluids and antibiotics, hot packing of infected teats, and surgical debridement of abscessed mammary glands Any affected animals should be isolated to prevent the spread of infection. Remove kits to prevent them from starving or contracting bacterial enteritis.65 Restrict contact with other carriers of S. aureus, including people, to minimize the risk of infection.55
Nonseptic cystic mastitis can develop in nonbreeding does (see Chapter 17).28 Mammary glands are swollen and firm, with discolored, distended nipples exuding clear to brown discharge. Glands usually are not painful and does usually are not systemically ill. This condition is often associated with uterine hyperplasia and adenocarcinoma. Treatment requires an ovariohysterectomy.
In young rabbits, S. aureus also causes exudative dermatitis with multiple raised pustules on the legs, head, back, and sides. One virulent biotype can cause high mortality of juvenile rabbits in rabbitries due to septicemia.19,55 Diagnosis and treatment is as for suppurative mastitis.
Methicillin-Resistant Staphylococcal Infection
Drug-resistant staphylococcal infections have been reported in rabbits. Methicillin-resistant S. aureus (MRSA) became a serious concern in human medicine during the late 1970s and has been reported frequently in animals over the past 10 years.45,60,69 MRSA strains are resistant to all penicillins, cephalosporins, and carbapenems; many are also resistant to aminoglycosides, macrolides, lincosamide, streptomycins, tetracycline, chloramphenicol, fluorquinolones, and rifampicin.76 Methicillin resistance also occurs in other staphylococcal species such as Staphylococcus intermedius and Staphylococcus schleiferi.
Numerous studies indicate potential transfer of these bacteria between humans and animals and vice versa, and evidence increasingly demonstrates that isolates from dogs and cats are indistinguishable from those found in human health care facilities.40,43,70 Research also suggests that veterinary hospital staff and hospitalized pets can transit MRSA back and forth.17,64,66,78,79 MRSA has been isolated in companion animals and livestock; pigs, in particular, have found to be a source of human infection.* Few studies have focused on the prevalence of MRSA in exotic pets. MRSA has been isolated in chinchillas and parrots, and another report cites MRSA in a pet rabbit and a guinea pig.77 MRSA was also isolated from a rabbit with bilateral facial dermatitis and conjunctivitis (K. Quesenberry, personal communication, 2010). The widespread nature of these “superbug” infections and their potential transmission between humans and animals necessitates awareness of this organism as another possible cause of dermatitis in rabbits. In any case of dermatitis in a rabbit that does not respond to empiric antibiotic therapy, submit a sample for bacterial culture and sensitivity testing.
Cellulitis
Cellulitis in rabbits usually occurs acutely and may develop secondary to respiratory tract infection.3,27,32,33 Affected rabbits have fevers of 104° to 108°F (40°-42.2°C), and the skin around the head, neck, and chest becomes painful, inflamed, and edematous. Bacteria commonly isolated from these lesions include S. aureus, P. multocida, and Bordetella bronchiseptica. In these cases, treat affected rabbits with parenteral antibiotics (enrofloxacin, beta lactams, and aminoglycosides) based on the results of culture and sensitivity testing, topical antiseptics (1% chlorhexidine or 10% povidone-iodine), and cool baths. In rabbits that survive, lesions may become necrotic eschars or abscesses requiring surgical debridement.
Moist Dermatitis
In rabbits, moist dermatitis usually develops on the chin, dewlap, or ventral neck (“slobbers”) or perianally as urine scald (“hutch burn”).* Chin or neck lesions can result from excessive drooling secondary to dental disease or from a constantly wet dewlap in rabbits that drink out of dirty water bottles or bowls. In addition, some rabbits chew their dewlaps as a displacement behavior for pain. Urine scald can be associated with excessive urination or urinary incontinence from renal disease (including renal infection with Encephalitizoon cuniculi), cystitis, urolithiasis, or urine “sludge.” Urine scald may also occur with immobility from posterior paresis, ulcerative pododermatitis (see below), obesity, genital infection with Treponema cuniculi (see below), vaginal discharge from uterine disease, or limited cage space/damp bedding. Rabbits that do not groom themselves may develop perianal and inguinal fur mats that absorb urine and trap feces, resulting in a moist dermatitis. With both perianal and ventral neck dermatitis, the skin may be inflamed, alopecic, ulcerated, necrotic, and fly-infested. Commonly, P. aeruginosa causes secondary dewlap infection and produces pyocyanin pigment that turns the skin blue-green; hence this condition is sometimes referred to as “blue fur disease.”19,80
To determine any underlying cause for moist dermatitis, take skull or abdominal radiographs and submit samples for urinalysis, a CBC, and a plasma biochemical analysis. Submit swab samples of exudate or skin for bacterial culture and sensitivity testing. Do a cytologic examination of a skin swab sample to look for yeast and the type of bacteria present (cocci or rods) to guide treatment pending culture results. Treat underlying diseases and correct associated environmental factors. Clip the hair over the affected skin and allow the area to dry. Drying agents, such as Domeboro Powder (Bayer Inc., Elkhart, IN) or dilute topical chlorhexidine, may help. Administer a systemic antibiotic while awaiting the results of culture and sensitivity testing and provide analgesics and/or nonsteroidal anti-inflammatory drugs (NSAIDs) for pain. Compounded topical preparations containing antibiotics, antifungal agents, and NSAIDs in combination, based on cytologic and bacterial culture results, can be helpful; consult with a veterinary dermatologist for recommendations. If obesity is a factor, ensure that the diet is high in fiber and low in calcium and encourage exercise. Keep affected rabbits indoors to prevent myiasis.16 Urine scald in grossly obese rabbits may require surgical removal of excess skin folds that interfere with urination; a more conservative approach is to restrict food and encourage exercise to promote weight loss.
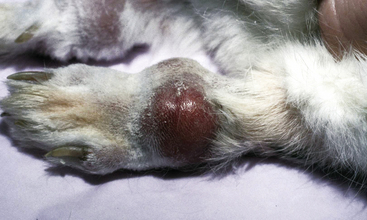
Ulcerative Pododermatitis
Ulcerative pododermatitis (sore hocks) is a chronic, granulomatous, ulcerative dermatitis of the plantar metatarsal and, occasionally, volar metacarpal and phalangeal surfaces of the feet. This condition usually results in avascular necrosis of the plantar foot surfaces from trauma due to rough, dirty floors or frequent thumping.19,73 It may also develop in rabbits with thin plantar fur pads (such as Rex rabbits, which lack protective guard hairs), in rabbits with altered weight bearing due to spondylosis, or in large-breed or obese rabbits as a result of ischemia and pressure necrosis from confinement in small cages with concrete or wire floors.* The plantar surfaces of rabbits housed on rough carpet, tile, or vinyl also are exposed to increased frictional forces, predisposing them to pododermatitis.19 Rabbits kept on inappropriate bedding shift their weight off their claws and the plantar surfaces of their feet and onto their metatarsi and hocks. This shift causes lesions to develop that start as erythematous decubital ulcers and then become secondarily infected, usually with S. aureus or P. multocida, from contaminated bedding. Infected ulcers progress to abscesses covered with raised, dry, hyperkeratotic fibrotic scabs. Infection can spread to underlying bone and ligaments, causing osteomyelitis and sepsis. Osteomyelitis and synovitis may lead to superficial flexor tendon displacement. This forces rabbits to shift weight permanently onto their hocks and away from their digits, thus exacerbating the condition and worsening the long-term prognosis. In addition, chronic bleeding from ulcerated feet can lead to anemia.
To treat pododermatitis, submit samples of abscessed tissue for bacterial culture and sensitivity testing and take radiographs of the legs to check for osteomyelitis.22 Clip ulcerated areas free of hair but be careful not to clip away hair surrounding ulcers, as the hairs may actually relieve pressure on the ulcer itself.19 Clean wounds with warm saline, lactated Ringer’s solution, or dilute antiseptics such as 0.05% chlorhexidine and debride necrotic tissue. Consider packing severe abscesses with antibiotic-impregnated PMMA beads or honey (see above). Surgical debridement is often very difficult or impossible because very little extra skin is present on the plantar metatarsus for wound closure.16,74 Postoperatively, bandage open wounds left to heal by second intention or delayed primary closure with light dressings. A variety of nonadherent semi-occlusive to occlusive dressings are available for wound treatment in small animals; Tegaderm (3M Medical-Surgical Division, St. Paul, MN), Telfa pads (The Kendall Co., Mansfield, MA), and other wound dressings have been used successfully in several rabbits. Protect superficial wounds with liquid bandage preparations (New Skin, Prestige Brands, Irvington, NY), surgical glue painted on topically, or cyanoacrylate skin protectants (Marathon Liquid Skin Protectant, Medline Industries Inc., Mudelein, IL). Alleviate pressure at ulcerated sites by applying donut-shaped bandages with the ulcer in the center of the donut.19 Regardless of the type of dressing used, change bandages daily to prevent reinfection from feces and urine. Additionally, a variety of topical agents that promote wound healing and epithelialization may be applied to aid in wound closure.16 Application of water-based, topical antibiotics, such as silver sulfadiazine (Silvadene Cream 1%, Monarch Pharmaceuticals, Bristol, TN) or a nontoxic antimicrobial product (Vetericyn, Innovacyn, Inc., Rialto, CA), and systemic antibiotics, selected based on results of culture and sensitivity testing, usually is warranted. Avoid using petroleum-based topical antibiotics because these are more likely to cause local allergic reactions and rabbits may ingest them. In addition, avoid using topical steroids in rabbits, as they may cause immunosuppression and delayed wound healing.
Change the environment to nonabrasive, solid cage floors and clean, soft, dry bedding such as towels, cellulose fiber bedding (CareFRESH, Absorption Corp., Ferndale, WA), or clean hay.16 Provide analgesia with NSAIDs and/or opioids. Increase the fiber and lower the carbohydrates in the diets of obese rabbits and encourage exercise. Unilateral pododermatitis that is unresponsive to treatment may require amputation at the midfemur. Bilateral severe pododermatitis involving osteomyelitis and infection of underlying tendons or ligaments may warrant euthanasia.
Rabbit Syphilis
Rabbit syphilis, also called venereal spirochetosis or “vent disease,” is a nonzoonotic, contagious venereal disease caused by the spirochete Treponema paraluiscuniculi (see also Chapter 17).16,54,55,63,80 Transmission is through direct contact with infected skin or from infected dam to kits at birth.3,22,28 Intrauterine transmission is not reported and there is an age-related susceptibility, with some young rabbits seeming relatively resistant to certain strains.53 Incubation periods are long, lasting up to 10 to 16 weeks.65 Lesions in affected, typically juvenile rabbits may appear as nonpruritic, erythematous, edematous papules and crusty ulcers at the mucocutaneous junctions of the lips, eyelids, nostrils, philtrum, vulva, prepuce, and perineum (Fig. 18-2).41 Affected rabbits also may experience metritis, abortion, or neonatal death. Lesions usually wax and wane over months. Recovered bucks may have star-shaped scrotal scars and can remain carriers.65 Asymptomatic carrier rabbits may develop lesions if exposed to stress (e.g., overcrowding, poor sanitation). Rabbit syphilis is diagnosed from clinical signs and identification of the characteristic corkscrew-shaped causative organisms with dark-field microscopic examination of wet-mounted skin scrapings.55 Serologic testing can also help in diagnosis but lesions may be present before animals are serologically positive; thus false negatives can occur.* Because of low sensitivity in comparison with other methods, demonstration of spirochetes in silver-stained histologic sections is a less reliable diagnostic tool.55
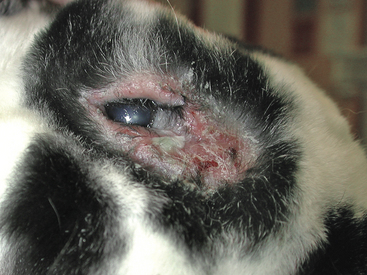
Fig. 18-2 Periocular erythema and erosions in a rabbit infected with Treponema cuniculi (rabbit syphilis).
(Courtesy of Stephen White, DVM. Picture from the case files of the Veterinary Medical Teaching Hospital, School of Veterinary Medicine, University of California. Used with permission.)
Rabbit syphilis is usually self-limiting; however, autoinfection from perineum to face is possible and rabbits with syphilis may be more susceptible to other infections. Treatment is with parenteral benzathine penicillin G/procaine penicillin G (42,000-84,000 IU/kg SC q7d for three treatments) or penicillin G procaine (40,000-60,000 IU/kg IM q24h for 5-7 days). Treat all exposed rabbits and remove nursing kits from dams during treatment to decrease the risk of their developing penicillin-associated enterotoxemia.19 Breeding rabbits should be inspected regularly for lesions.
Necrobacillosis
Necrobacillosis, or Schmorl’s disease, is an uncommon skin infection with Fusobacterium necrophorum, an anaerobic, filamentous gram-negative bacterium normally found in the gastrointestinal tract and feces.22,33 Infection occurs commonly from wound contamination. Abscessed, ulcerated, necrotic lesions may be found around the head, neck, and feet.3,19 Does with large dewlaps that salivate profusely or rabbits with malocclusion may be prone to necrobacillosis due to excessive moisture in skin.55 The causative bacterium may be isolated from anaerobic culture of affected tissue. Debride and flush lesions and administer antibiotics effective against anaerobic bacteria, such as penicillin G procaine.
Fungal Infections
Dermatophytosis
Dermatophytosis, or ringworm, is a potentially zoonotic and often asymptomatic infection of rabbit skin, most commonly caused by Trichophyton mentagrophytes.† Rabbits are less often infected with Microsporum species, but this species may be more common in pet rabbits.81 Dermatophytosis occurs more often in young rabbits, possibly because of their incompletely developed immune systems and low levels of fungistatic fatty acids in sebum. Asymptomatic carriers may develop lesions in response to overcrowding, malnutrition, or other infections. Rabbits also may acquire infection from humans or other pets.
Dermatophytes cause alopecic skin lesions around the head, legs, feet, and nail beds that may be dry, crusty, erythematous, or pruritic. Histopathologic examination shows a hyperkeratotic and acanthotic epidermis with an acute to chronic inflammatory cell infiltrate in the underlying dermis. Diagnose dermatophytosis based on growth of the infecting organism on dermatophyte culture medium from hair or skin samples. Speciating the dermatophyte may determine the origin of the dermatophyte infection. Fungal mycelia and arthrospores on hair shafts also may be seen on skin scrapings or hair plucks mounted in 10% potassium hydroxide or in skin biopsy samples stained with a periodic acid-Schiff stain, Gridley fungal stain, or Gomori’s methenamine silver stain. Fluorescence of mycelia under ultraviolet light from a Wood’s lamp is not a reliable method of testing in rabbits because T. mentagrophytes does not fluoresce and debris, bacteria, and keratin plugs can cause false-positive white to blue fluorescence.6
Although most dermatophyte infections in rabbits are self-limiting, treatment is recommended because of potential zoonosis.6,57 Several methods can be used to treat dermatophytosis in rabbits. Localized, topical therapy for dermatophytosis is not recommended because dermatophytes can also be present in nonlesional areas.
Effective treatments for dermatophytosis include dips with lime sulfur solution (LymDyp, IVX Animal Health, Inc., St. Joseph, MO) 1:32 dilution with water twice weekly, or 0.2% enilconazole (Immaveral, Janssen; not available in the United States) twice weekly. There have been anecdotal reports of stress-induced death from bathing rabbits; thus rabbits may have to be tranquilized beforehand. In addition, treat rabbits with multiple lesions systemically with griseofulvin (15-25 mg/kg PO q24h or divided q12h for 30 days; Grifulvin V Suspension, Ortho Pharmaceutical, Raritan, NJ).3,27,41,74 If griseofulvin is in an ultramicrosized form, decrease the dose by 50%, and administer with a high-fat meal for better absorption.6 Use griseofulvin cautiously, because at high doses it can cause bone marrow suppression and panleukopenia.11 Also, griseofulvin is teratogenic and cannot be given to pregnant does. Owners administering griseofulvin should wear gloves. Other drugs used to treat dermatophytosis include itraconazole (Sporanox, Ortho-McNeil-Janssen Pharmaceuticals, Titusville, NJ), 5 to 10 mg/kg PO q24h, and terbinafine (Lamisil, Novartis Pharmaceuticals Corp, St. Louis, MO), 10 mg/kg PO q24h. Anecdotal reports exist of treatment of rabbit dermatophytosis with lufenuron (Program, Novartis Animal Health, Greensboro, NC), an insect growth regulator that inhibits chitin synthesis in fungal cell walls.6 However, use of lufenuron in rabbits is off label; controlled studies of this drug in rabbits have not yet been performed, and this treatment is not considered effective in the management of dermatophytosis in other animals.
The clipping lesions of before applying topical medications is controversial. Some feel that clipping helps to make medications penetrate the skin; others warn against clipping because of the risk of inducing skin abrasions through which infection may become generalized.6 If hair is clipped, clip only the hair surrounding the wound and dispose of infected hair carefully.
Continue systemic antifungal treatment until monthly fungal cultures are negative twice.11,28,33 Most treatments last a minimum of 3 to 4 months. Disinfection of the environment also is essential. Vacuum contaminated areas, and clean all surfaces with a 1:10 solution of bleach and water. Foggers containing enilconazole or formaldehyde are preferred to steam cleaning for carpets because steam cleaning does not reach a temperature high enough to kill infectious spores. Commercial steam cleaning services are preferable, because they use higher-temperature steam to clean carpets. Be careful not to use oral cisapride concurrently with azole drugs as they may potentially interact adversely.19
Dermatophytes may be hard to eliminate from large rabbit colonies. Large numbers of infected rabbits can be sprayed with a 2% to 3% lime sulfur solution weekly for 4 weeks. In large outbreaks of dermatophytosis, also treat with a systemic antifungal such as griseofulvin-medicated diets (0.825 g griseofulvin per kilogram of diet).41
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree