CHAPTER 21 Dental and Oral Diseases
Resorption of multiple teeth is very common in cats. However, its etiology remains a mystery up to this day. Similarly, stomatitis has been described for many decades, but progress in identifying its cause and providing effective treatment continues to be challenging. Oral and maxillofacial trauma also manifests somewhat uniquely in the cat in that the mandibular symphysis, the temporomandibular joints, and the hard palate are typically affected, but rarely the midportion of the mandibular body. Squamous cell carcinoma is the most common tumor of the oral cavity in the cat, and curative surgical treatment is usually reserved for those tumors affecting the lower jaw. A comprehensive review of dental and oral diseases in the cat has recently been published.8
Oral Anatomy
Eruption of Deciduous and Permanent Teeth
Cats have two sets of teeth, the deciduous and permanent dentitions. Deciduous incisors erupt at 2 to 3 weeks, canines at 3 to 4 weeks, and premolars at 3 to 6 weeks of age. There should be 26 deciduous teeth. Permanent incisors erupt at 3 to 4 months, canines at 4 to 5 months, premolars at 4 to 6 months, and molars at 4 to 5 months of age. There should be 30 permanent teeth. At 7 months of age, the young cat should have 30 fully erupted permanent teeth in place (Table 21-1).
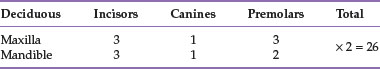
TABLE 21-1 Eruption of the Deciduous and Permanent Dentitions in the Domestic Cat
| Deciduous Teeth | Permanent Teeth | |
|---|---|---|
| Incisors | 2-3 weeks | 3-4 months |
| Canines | 3-4 weeks | 4-5 months |
| Premolars | 3-6 weeks | 4-6 months |
| Molars | No deciduous molars | 4-5 months |
There are four specific types of teeth, each serving a distinct purpose. The incisors are designed to cut, prehend, and groom. The canines are used to penetrate and grasp prey or food and also function as defensive weapons in protection. The cheek teeth (premolars and molars) assist in the ability to hold and carry, in addition to the breaking and tearing of food into smaller pieces in preparation for digestion. The so-called carnassials refer to the maxillary fourth premolar and mandibular first molar teeth, which serve a shearing function in carnivores.66
Tooth Formula in the Domestic Cat
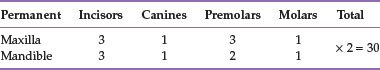
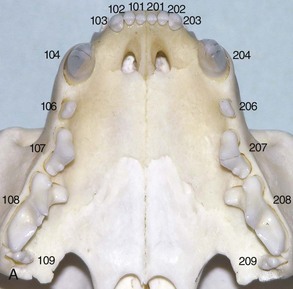
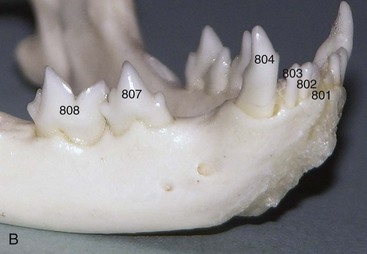
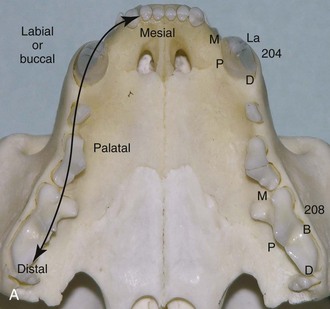
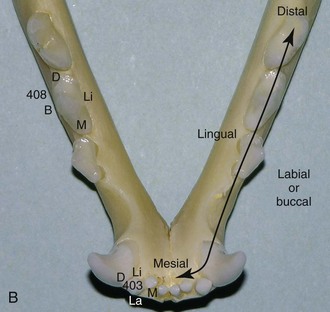
The total number of teeth in the cat is greatly decreased compared with that of the dog, and the shapes of the crowns of feline teeth reflect the function of a true carnivore.90 Accepted dental formulas for the deciduous and permanent dentition in the domestic cat are shown in Tables 21-2 and 21-3. Using the modified Triadan tooth-numbering system, each jaw quadrant is numbered as follows: right maxillary quadrant 100 (500 when referring to deciduous teeth), left maxillary quadrant 200 (600 when referring to deciduous teeth), left mandibular quadrant 300 (700 when referring to deciduous teeth), and right mandibular quadrant 400 (800 when referring to deciduous teeth).66
Beginning with 01 for the first incisor (the one closest to the midline), teeth are consecutively numbered from mesial (the surface of the tooth that faces the midline of the dental arch) to distal (the surface of the tooth that faces away from the midline of the dental arch). Several premolars and molars have been evolutionarily lost in the permanent dentition of the cat. The canine (04) and the first molar (09) are present as reference teeth to allow counting forward or backward when numbering teeth. The permanent maxillary first (05) premolar and the permanent mandibular first (05) and second (06) premolars are absent in the cat. Because the maxillary fourth premolar (08) and mandibular first molar (09) are the largest cheek teeth of the upper and lower jaws, counting forward identifies the premolars between the maxillary canine and fourth premolar as the maxillary second and third premolars (teeth 06 and 07). Similarly, the premolars between the mandibular canine and first molar are identified as the mandibular third and fourth premolars (teeth 07 and 08).66
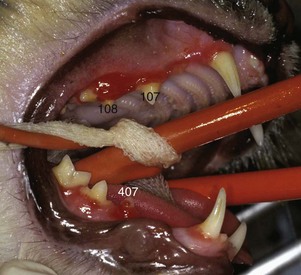
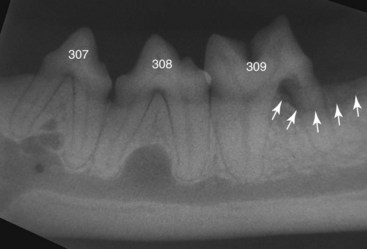
Taking the quadrant and tooth number into consideration, three numbers are used to identify a specific tooth. For example, the permanent right maxillary canine is tooth 104. The permanent right maxillary fourth premolar is tooth 108. The permanent left maxillary second premolar is tooth 206. The permanent left mandibular third and fourth premolars are teeth 307 and 308. The permanent right mandibular first molar is tooth 409 (Figure 21-1). The deciduous right maxillary canine is tooth 504. The deciduous right mandibular fourth premolar is tooth 808 (Figure 21-2).
Teeth
The tooth consists of a crown and one or more roots. Enamel (with >95% mineralization, the hardest tissue of the body) covers the crown, and cementum covers the root(s). The borderline between the anatomic crown and root(s) is the cementoenamel junction.21 The incisors and canine teeth have one root. The maxillary second premolars and first molars have two roots that are often fused to each other, giving the appearance of only one root.114 The mandibular third and fourth premolars and first molars and the maxillary third premolars have two roots. The maxillary fourth premolar has three roots. The furcation is where two or more roots meet at the crown.66
Dentin makes up the bulk of the adult tooth. It is approximately 70% mineralized and porous, and consists of thousands of dentinal tubules per square millimeter radiating outward from the pulp to the enamel in the crown and cementum in the root.90 Odontoblasts line the periphery of the pulp cavity and produce dentin, which—in a vital tooth—is laid down throughout life. Dentinal tubules contain cytoplasmic processes of odontoblasts, fluid, and nerves extending from the pulp. Tooth pain may result from fluid movement and nerve stimulation in the area of exposed tubules. Odontoblasts adjacent to exposed dentinal tubules may respond by producing tertiary dentin to halt the progression of an external insult.66
The pulp cavity consists of the pulp chamber in the crown and the root canal(s) in the root(s) of the tooth. It contains the pulp, which is made up of undifferentiated mesenchymal cells, fibroblasts, odontoblasts, blood and lymph vessels, and nerves.90 Odontoblasts line the inside of the pulp cavity at the periphery of the pulp, initially producing nonmineralized predentin, which later becomes mineralized dentin. Unlike human teeth that have only one apical foramen, the pulp of cat teeth connects with periapical tissues through several foramina in the root apex (forming the apical delta). Secondary, accessory, lateral, and furcation canals also may connect pulp tissue with the periodontal ligament.80 Therefore entrance into the pulp cavity can be through exposed dentinal tubules, direct pulp exposure, and apical and non-apical ramifications.
The tooth “grows” toward the inside. The dentin becomes continually thicker in a vital tooth. Dentin apposition along the inside of the pulp cavity continues throughout life, unless irreversible pulpitis or pulp necrosis occurs. Therefore teeth of young adult cats have a fairly wide pulp cavity (Figure 21-3). In older cats the pulp cavity of teeth with vital pulps is usually very narrow (Figure 21-4). The narrower the pulp cavity, the thicker are the dentinal walls, and thus the stronger and more aged is the tooth.
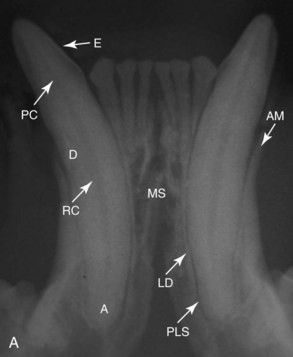
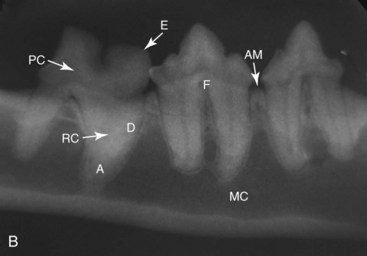
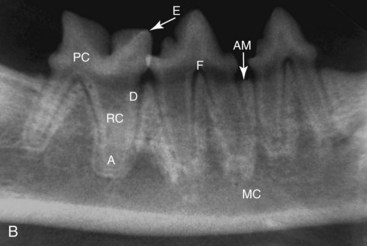
FIGURE 21-4 Radiographs of the mandibular incisors and canines (A) and the right mandibular cheek teeth (B) in a cat older than 3 years of age. Note the thicker dentinal walls, narrower pulp cavities, and closed root apices, compared with Figure 21-3. E, Enamel; PC, pulp chamber; D, dentin; RC, root canal; A, apex; MS, mandibular symphysis; AM, alveolar margin; LD, lamina dura; PLS, periodontal ligament space; F, furcation; MC, mandibular canal.
Periodontium
The periodontium is a functional unit and consists of the gingiva, periodontal ligament, cementum, and alveolar bone.90 The gingiva surrounds the tooth like a collar and is firmly attached to the alveolar bone and cervical portion of the tooth. The most coronal edge of the gingiva is the gingival margin. A normal space between the tooth and most coronal gingiva is called the gingival sulcus, which should not be deeper than 0.5 mm in cats. The periodontal ligament acts as shock absorber and attaches the tooth to the alveolar bone by means of Sharpey’s fibers. Some fibers connect adjacent teeth by traveling through or coronal to the alveolar septum. Radiographically, the periodontal ligament space appears as a dark line surrounding the root.
The cementum covers the root(s) and is produced by cementoblasts. It is similar in mineral composition and histologic appearance to bone. Cementum width increases with age.66 An excessive production of cementum (hypercementosis) is often seen in cat teeth, most commonly at the apical portion of the root. Alveolar bone surrounds the alveolar socket. An increased radiodensity of alveolar bone is visible adjacent to the periodontal ligament space, referred to as the lamina dura, which is an extension of cortical bone into the alveolus. The most coronal edge of the alveolar bone is the alveolar margin.66 Alveolar bone is constantly remodeling in response to use and the forces placed on it.
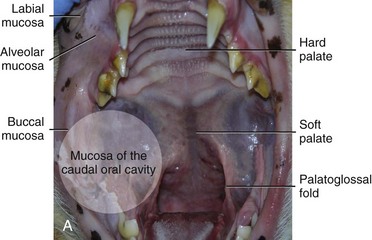
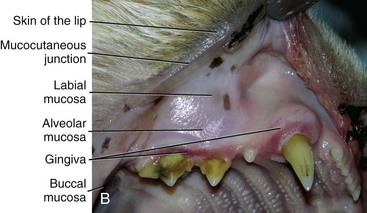
Oral Mucosa
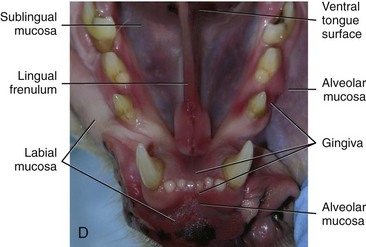
Oral mucosa other than gingiva includes the very flexible and elastic alveolar mucosa, which covers the alveolar bone and is separated from the gingiva by the mucogingival junction; the labial and buccal mucosae, which line the inside of the lip and cheek; the loose sublingual mucosa, the mucosa covering the dorsal and ventral tongue surfaces; the mucosa of the hard palate, which is firmly attached to underlying maxillae and palatine bones; and the mucosa of the soft palate.66 The oral mucosa is separated from the skin by the mucocutaneous junction (Figure 21-5).
Bones and Joints
Most cats are mesaticephalic; in other words, their heads are of medium proportions. Brachycephalic cats, such as the Persian, have short, wide heads. Dolichocephalic cats, such as the Siamese, have long, narrow heads. The upper jaw and the face consist of the paired incisive bones; maxillae; palatine, nasal, zygomatic, and temporal bones; and the unpaired vomer bone. The incisive bones carry the maxillary incisor teeth, and the maxillae carry the maxillary canines, premolars, and molars. The infraorbital canal (containing the infraorbital artery, vein, and nerve) penetrates the maxillary bone in the area of the fourth premolar and molar teeth.66
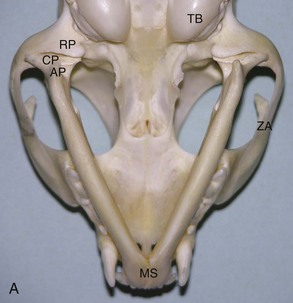
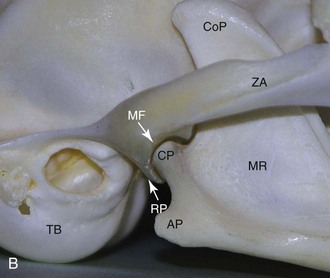
The lower jaw consists of the paired mandibular bones. The ventral third of each mandible includes the mandibular canal, which contains the inferior alveolar artery, vein, and nerve. Right and left mandibles are separated rostrally by a fibrocartilaginous synchondrosis (mandibular symphysis) and carry all mandibular teeth. The temporomandibular joint is formed by the condylar process of the mandible and the mandibular fossa and retroarticular process of the temporal bone (Figure 21-6). A thin fibrocartilagenous disk lies between the hyaline cartilage–covered articular surfaces. A thick band of fibrous tissue on the lateral aspect of the joint capsule forms the lateral ligament, which tightens when the jaw opens.66
Muscles, Cheeks, and Lips
The masticatory musculature includes the masseter, temporal, and pterygoid (medial and lateral) muscles, which close the mouth, and the digastricus muscle, which opens the mouth.90 The lips and cheeks of cats are “tighter” and their oral vestibules less spacious than in dogs, making their labial and buccal mucosae less available for closure of large intraoral wounds. The commissure is where the upper and lower lips meet. There are three important structures within the soft tissues of the cheek that run nearly parallel over the masseter musle in a rostrocaudal direction: the dorsal and ventral buccal branches of the facial nerve and the parotid duct traversing between the two nerves and opening into the mouth at the parotid papilla in the buccal mucosa near the maxillary fourth premolar.66
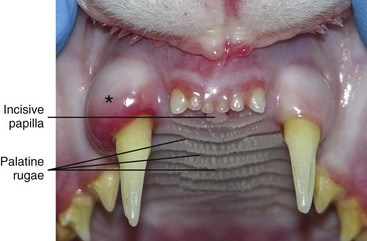
Palate
The primary palate is made up of the rostral upper lip and the most rostral hard palate. The majority of the hard palate and the soft palate constitute the secondary palate. The hard palate mucosa is non-elastic and has several transverse ridges (palatine rugae) and depressions. On the midline rostral to the first palatine ruga and just caudal to the maxillary first incisor teeth is the incisive papilla, which should not be confused with an abnormal proliferative lesion (Figure 21-7).90 The main blood supply to the hard palate mucosa is provided by the paired major palatine arteries, which pass through the palatine canals and emerge at the major palatine foramina palatal to the level of the maxillary fourth premolar teeth about halfway toward the midline, from where they run rostrally in the palatine sulci to the palatine fissures.66
Tongue
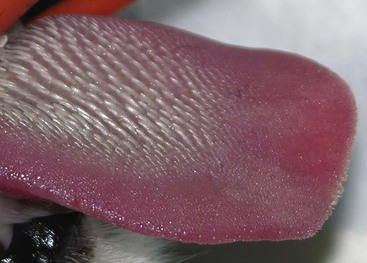
The lingual mucosa is thick and heavily cornified dorsally but thin and less cornified ventrally. The cat’s dorsal tongue surface is very rough, with firm papillae that point caudally (Figure 21-8). The lingual frenulum, which is part of the sublingual mucosa whose submucosa contains the paired sublingual veins and mandibular and sublingual gland ducts, connects the body of the tongue to the floor of the mouth. The sublingual caruncles are situated at the frenulum’s rostroventral aspect and contain the orifices of mandibular and sublingual gland ducts. The lingual artery is the major blood supply to the tongue.66
Salivary Glands
There are four pairs of major salivary glands in cats: the parotid gland surrounding the horizontal ear canal; the mandibular gland situated in the Viborg’s triangle, near the maxillary and linguofacial veins; the sublingual gland, with its monostomatic part intimately attached to the mandibular gland and its polystomatic part located more rostrally between the mandible and the tongue; and the zygomatic gland, located on the floor of the orbit, whose ducts open on the buccal mucosa near the maxillary first molar tooth.90 Scattered glandular tissue is present submucosally in the lips (ventral and dorsal buccal glands). A small lingual molar gland is situated caudolingually to each mandibular first molar tooth and should not be confused with an abnormal proliferative lesion.88
Lymph Nodes and Tonsils
There are three lymph centers in the head (parotid, mandibular, and retropharyngeal).66 The parotid lymph node is located at the rostral base of the ear. Several mandibular lymph nodes lie ventral to the angle of the jaw above and below the linguofacial vein. The medial retropharyngeal lymph node is an elongated, transversely compressed node and lies along the craniodorsal wall of the pharynx. The paired small palatine tonsil is attached to the lateral pharyngeal wall.
Neurovascular Structures
The maxillary artery provides blood supply to the upper jaw by way of the infraorbital, palatine (major and minor), and sphenopalatine arteries. The inferior alveolar artery (running in the mandibular canal) is a branch of the maxillary artery and provides blood supply to the lower jaw. It exits at the caudal, middle, and rostral mental foramina to supply the lower lips. Veins often exist concurrently with arteries and empty by way of the maxillary and linguofacial veins into the external jugular vein.66
Common Terminology
Rostral refers to the direction toward the tip of the nose, caudal to the direction toward the tail, ventral to the direction toward the lower jaw, and dorsal to the direction toward the top of the head or muzzle. Mesial is the surface of a tooth facing the midline of the dental arch, and distal is the surface of a tooth facing away from the midline of the dental arch. Labial is the surface of a tooth facing the lip, and buccal is the surface of a tooth facing the cheek. Lingual refers to the surface of mandibular teeth facing the tongue, and palatal refers to the surface of maxillary teeth facing the hard palate (Figure 21-9). Occlusal refers to the surface of a tooth facing an opposing dental arch, coronal refers to a location or direction toward the crown of a tooth, and apical refers to a location or direction toward the apex of a tooth’s root. Subgingival refers to an area that is apical to the gingival margin, and supragingival refers to an area that is coronal to the gingival margin.66
Oral Examination
Patient History and Clinical Signs
Age, breed, and sequence of development of clinical signs often are useful indicators. A full patient history is essential and should include questions about appetite; eating and drinking patterns; prehending, chewing, and swallowing; preference for soft or hard food; behavioral idiosyncrasies; access to treats and toys; vomiting, diarrhea, and weight loss; coughing and sneezing; polydipsia and polyuria; scratching, head shaking; presence of rapid lower jaw motions; previous and current medications (and responsiveness to medications); the animal’s environment; and the type and frequency of home oral hygiene.46
The presence of halitosis, preferential chewing on one side of the mouth, inability or reluctance to open or close the mouth, dropping food from the mouth, drooling of saliva, inappetence, weight loss, sneezing, nasal discharge, pawing at the face, enophthalmos or exophthalmos, oral and maxillofacial swellings, pain on palpation of oral and maxillofacial tissues, atrophy of masticatory muscles, malocclusion, and other abnormal clinical signs should be assessed. It is often helpful for the examiner to watch the animal eat and drink if the owner reports any abnormal behavior during eating and drinking.46
Halitosis may be caused by oral disease (e.g., periodontal disease, stomatitis, neoplasia), nonoral diseases (e.g., uremia, respiratory or gastrointestinal disease), and the diet. Inappetence may result from pain associated with inflammation and ulceration in the oral cavity. This may progress to unwillingness or inability to drink, which in turn leads to dehydration. Pawing at the mouth and rubbing the mouth on furnishings are indications of oral or facial pain. Drooling usually results from the reluctance or inability to swallow rather than from increased salivary production. It also may be caused by the reluctance or inability to close the mouth. Saliva may be blood stained if ulceration is present in the mouth. Dysphagia (i.e., difficulty in or pain on swallowing) may result from inflamed, ulcerated, or traumatized tissues that cause local pain or from obstruction to the mechanics of swallowing by a mass lesion, neurologic disease, or palate defects. Rapid lower jaw motions (“jaw chattering”) often indicate oral pain in cats with tooth resorption. Nasal discharge may be related to rhinitis, endodontic disease, neoplasia, or a palate defect.46
The cat may be unable or unwilling to eat or chew on the side of the mouth that has a problem. Teeth on the affected side may then show increased plaque and calculus accumulation compared with those on the healthy side. Differential diagnoses for a cat that is unable or unwilling to open the mouth include oral ulceration, temporomandibular joint ankylosis, maxillofacial fractures, tetanus, ocular disease, space-occupying retrobulbar lesion, ear disease, and neoplasia. Differential diagnoses for a cat that is unable or unwilling to close the mouth include temporomandibular joint luxation or fracture of bones forming the joint, open-mouth jaw locking, maxillary and (bilateral) mandibular fractures, and neoplasia.46
Extraoral Examination
The jaws, intermandibular tissues, zygomatic arches, and neck should be palpated for pain, asymmetry, discontinuity, crepitus, and emphysema. The range of mouth opening is assessed, which also provides information about abnormalities of the temporomandibular joints and muscles of mastication.46
Intraoral Examination
The skin and mucocutaneous areas should be examined before opening the cat’s mouth. The labial and buccal mucosa is examined by lifting the cat’s upper and lower lips. The oral mucosa should be moist, intact, and nonpainful on touch and may be pigmented. The color, size, location, thickness, surface characteristics, and symmetry of any oral lesions should be noted.46 The incisors, canines, and most cheek teeth can be evaluated without opening the mouth. Opening the mouth is greatly facilitated when the cat’s head is rotated dorsally. One hand holds the entire head (in the area of the zygomatic arches) and then rotates it dorsally. The other hand opens the mouth by pushing the lower jaw ventrally (Figure 21-10). The ventral surface of the tongue and sublingual tissues can be inspected by gently forcing the thumb of the second hand into the intermandibular area. This raises the tongue. The hard palate can also be inspected.46 Obvious lesions such as fractured teeth, moderate to severe periodontal disease, stomatitis, and oral masses can often be identified in the conscious patient. However, sedation or general anesthesia is usually required for a thorough intraoral examination.
The two most important instruments for evaluation of dental and periodontal tissues are the dental explorer and periodontal probe (Figure 21-11). The structural integrity of teeth is assessed with a dental explorer whose pointed tip can detect irregularities of the crown surface. It is also used to determine the presence of pulp exposure in a fractured tooth. The alveolar mucosa over the roots of the teeth should be inspected and palpated for the presence of swellings and sinus tracts (the latter are often located near the mucogingival junction), which may indicate endodontic disease or neoplasia.46 The periodontal probe is invaluable for an accurate periodontal examination. The probe is gently inserted into the gingival sulcus, and measurements are obtained at several locations around the entire circumference of each tooth. The gingival sulcus of cat teeth should not be deeper than 0.5 mm. Greater measurements indicate the presence of a periodontal pocket or, in the case of gingival enlargement, a pseudopocket. Other periodontal parameters include plaque and calculus (tartar) accumulation, gingival index, gingival recession or enlargement, total attachment loss, tooth mobility, and missing teeth. Any other abnormalities should be recorded in the dental chart, such as persistent (retained) deciduous teeth, supernumerary teeth, dental or skeletal malocclusion, circumscribed ulcers, widespread oral inflammation, palate defects, oral masses, lacerations, and other signs of trauma.46
Laboratory Examination
Examination for systemic disease is important to assess anesthetic risk or determine the possibility of dental and oral lesions being secondary to a systemic condition.46 Preanesthetic blood tests should include a complete blood cell count and biochemical profile. Blood typing and cross-matching may occasionally be indicated. Urinalysis and cardiac examination are performed as necessary. Cats with acute or chronic oral inflammation (beyond gingivitis) should be tested for feline leukemia virus (FeLV), for feline immunodeficiency virus (FIV), and occasionally for feline bartonellosis.
Diagnostic Imaging
Dental Radiography
Dental radiographs should always be obtained before tooth extraction to assess alveolar bone health and variations in root anatomy and to determine the presence of dentoalveolar ankylosis or replacement resorption of roots that could complicate the extraction procedure. They are also essential during all steps of endodontic procedures, including assessment of treatment outcome at follow-up visits. In addition to dental-related conditions, most jaw pathology can be satisfactorily assessed with dental (nonscreen) film and intraoral and extraoral imaging techniques.28
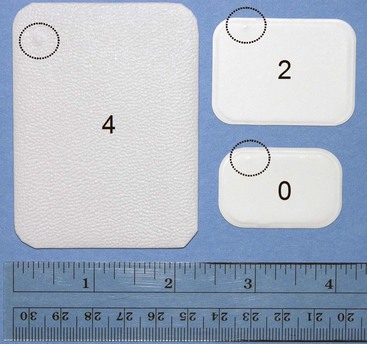
Needed equipment includes a dental radiography machine, dental (nonscreen) films, a chairside film processor, developer and fixer solutions, and a view box. Digital imaging uses sensor pads or phosphor plates (instead of films) that transfer the image to a computer. The digital system requires less radiation to produce an image, which may also be modified with software programs. Exposure time often is the only adjustment to be made and depends on the size of the patient and tissue thickness to be imaged.82,84 Dental film is available in several sizes and speeds, with sizes 0, 2, and 4 and D film (ultra speed) most commonly used (Figure 21-12). The largest dental film (size 4) is very useful to evaluate diseases of the nasal cavity, orbit, zygomatic arch, mandibular ramus, temporomandibular joint, and tympanic bulla in cats. The films are inside a moisture-resistant packet and surrounded by black paper. A layer of lead foil is located at the back of the packet next to the tab opening, protecting the film from secondary radiation. A dimple is located in one corner of the film packet and also on the film and is used to distinguish images obtained from the left and right sides of the mouth on the processed radiographs. The convex (raised) surface of the dimple must face the radiographic beam during exposure. Dental rapid developer and fixer solutions are placed in small containers within a chairside film processor (from left to right: developer, water, fixer, and water).47
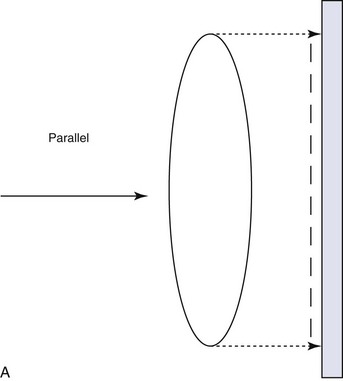
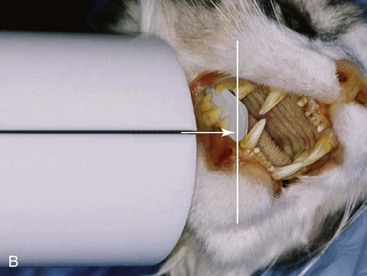
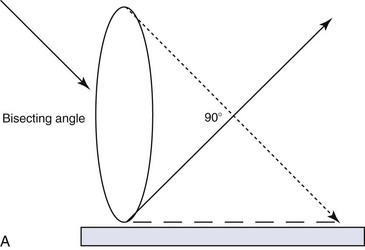
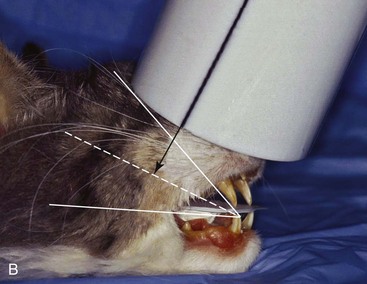
All personnel should leave the room while radiographs are exposed. If this is not possible, anyone remaining in the room should stand at least 6 feet from the radiographic cone and at a 90- to 135-degree angle to the tube head. Gauze or paper may be used to hold the films in proper position inside the mouth of an intubated cat. The parallel technique is used for imaging the mandibular molars and the caudal mandibular premolars, with the film placed parallel to the teeth and the radiographic beam directed perpendicular (90 degrees) to the film and teeth (Figure 21-13).84 The bisecting angle technique minimizes distortion when obtaining radiographs of all maxillary teeth and the mandibular canines, incisors, and rostral premolars (Figure 21-14).42 The film is placed as close to the teeth as possible. The angle that is formed between the long axis of the teeth and the plane of the film is bisected by an imaginary line. The tube head is positioned perpendicular to this imaginary line. An extraoral technique has also been suggested for imaging the maxillary cheek teeth to avoid overlapping of the teeth with the zygomatic arch of the cat.28,47,83
The lid of the chairside film processor must be closed when processing dental radiographs. One hand holds the film, the other hand a film clip. Both hands are slid through the front windows of the processor. The exposed film is removed from the packet and placed in the film clip. The film is first placed into developer for about 30 seconds, then briefly rinsed in water, and placed in fixer for at least 60 seconds before viewing. After another brief water rinse, the film may be viewed using a dental view box. After initial viewing the film should be placed for another 15 minutes in the fixer solution. This is followed by thorough rinsing under running water for 20 minutes before air drying the film. Films dried over night are stored in a labeled envelope and kept as part of the patient’s medical record.28,86
Dental radiographs should be viewed in labial mounting (all of the radiographs in this chapter were obtained with dental film and are arranged in labial mounting), which requires that the processed film be placed on the view box with the raised dot facing the viewer.28 It is determined whether the image is of the upper or lower jaw and of the left or right side. The only three-rooted teeth are the maxillary fourth premolars. The palatine fissure is also located in the upper jaw. The ventral mandibular cortex or mandibular canal is often visible on films of the lower jaw. Films of teeth of the left jaws are placed on the right side of the view box, and those of the right jaws on the left side of the view box. Each film should be rotated so that the crowns of the maxillary teeth face downward and those of the mandibular teeth face upward.
The enamel, dentin, cementum (visible radiographically only when thickened), alveolar margin, periodontal ligament space, lamina dura, and pulp cavity are evaluated. The mandibular canal is visible as a radiolucent tubular structure in the mandible. Mental foramina and palatine fissures may sometimes be mistaken for periapical pathology.28,47
Computed Tomography
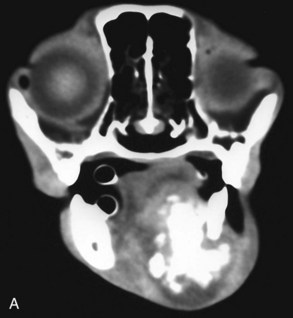
Computed tomography is a useful imaging modality for the diagnosis and treatment planning of oral and maxillofacial trauma, neoplasia, and many other conditions.3,108 It is of great value for exploration of a large volume of soft and hard tissue in a significantly shorter examination time and at a much lower cost than magnetic resonance imaging. This is particularly important when a rapid diagnosis is needed for patients with head trauma or uncertain head pathology and for those that are less than optimal anesthesia candidates. Computed tomography is of great value for detection of hard tissues, which is imperative when defining tumor margins and planning radical surgical excision. It also allows three-dimensional reconstruction, which facilitates understanding of the overall appearance of lesions, and can help guidance of a needle aspiration to establish a cytologic diagnosis.
Soft tissue structures are evaluated on soft tissue algorithm images, and the teeth, bones, and joints of the head are evaluated on bone algorithm images (Figure 21-15). Window levels and widths are adjusted manually as needed. Maxillofacial soft tissue structures of interest include the masticatory muscles, salivary glands, soft tissue coverings of the nasal and oral cavity, soft palate, pharynx and larynx, and head and neck lymph nodes. These soft tissues can be evaluated for their size, precontrast tissue attenuation and shape of abnormal densities, and degree and distribution of contrast enhancement. Enlarged soft tissues are consistent with edema, inflammation, or neoplasia. Abnormally small soft tissue structures are indicative of atrophy, necrosis, or fibrosis. Precontrast tissue hypoattenuation indicates increased fluid content consistent with edema. Irregular contrast enhancement is indicative of areas of increased vascularity consistent with inflammation or neoplasia, and non-enhancing cores are suggestive of necrosis or abscess. Bones and joints of the head are evaluated for any evidence of periosteal reaction or periarticular new bone formation, fractures, osteolysis, deformity, masses, and joint pathology.37 The teeth are evaluated for structural defects, abnormal root canal widths, and changes to the periodontal attachment apparatus.
Local and Regional Anesthesia
Local and regional anesthesia allows reduction in the concentration of an inhalant anesthetic, which minimizes complications from hypotension, bradycardia, and hypoventilation. Patients consequently recover more quickly and with fewer complications. Furthermore, local and regional anesthesia continues to provide analgesia in the postoperative period, thus increasing patient comfort and decreasing the need for systemic administration of analgesics.6,43,59,103
Local anesthesia (e.g., infiltration anesthesia, use of topical anesthetic gels, and splash block) is less commonly performed in dentistry and oral surgery. Regional anesthesia (nerve blocks) refers to injection of a local anesthetic solution around a major nerve, utilizing 27-gauge,  -inch needles on 1-mL syringes (22-gauge needles when going through skin).53,59,103 Commonly used local anesthetics in dentistry and oral surgery include bupivacaine 0.5% (effective for 6 to 10 hours) and lidocaine 2% without epinephrine (effective for less than 2 hours). The onset time for analgesia is longer with longer-acting local anesthetics (a few minutes for lidocaine, up to 30 minutes for bupivacaine). The total maximum dosage in cats is 2 mg/kg for bupivacaine and 1 mg/kg for lidocaine.53,59 There are 5 mg of bupivacaine in 1 mL of a 0.5% solution (bupivacaine 0.5%).
-inch needles on 1-mL syringes (22-gauge needles when going through skin).53,59,103 Commonly used local anesthetics in dentistry and oral surgery include bupivacaine 0.5% (effective for 6 to 10 hours) and lidocaine 2% without epinephrine (effective for less than 2 hours). The onset time for analgesia is longer with longer-acting local anesthetics (a few minutes for lidocaine, up to 30 minutes for bupivacaine). The total maximum dosage in cats is 2 mg/kg for bupivacaine and 1 mg/kg for lidocaine.53,59 There are 5 mg of bupivacaine in 1 mL of a 0.5% solution (bupivacaine 0.5%).
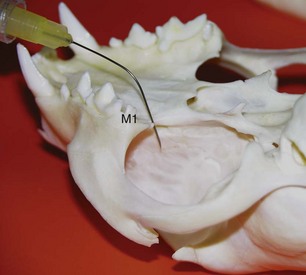
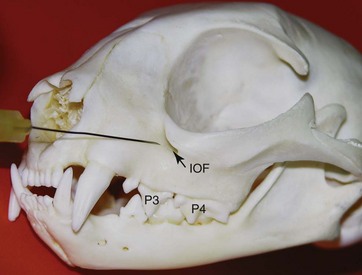
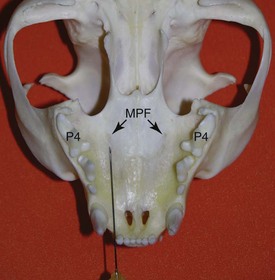
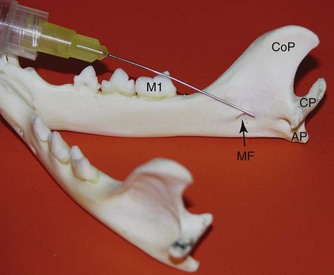
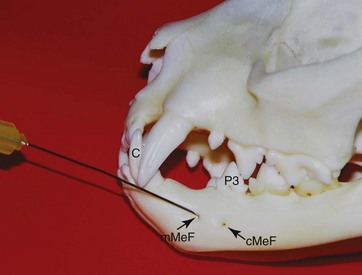
The maxillary nerve block is given just caudal to the first molar tooth where the maxillary nerve enters the infraorbital canal through the maxillary foramen (Figure 21-16). Care must be taken not to inject anesthetic into the eye globe. The areas blocked include the incisive bone, maxilla and palatine bone, all maxillary teeth on that side, and adjacent soft tissues. Because the infraorbital canal is very short in the cat and the maxillary nerve can easily be reached by a needle advanced through the infraorbital canal, an infraorbital approach is usually chosen to perform a maxillary nerve block. The infraorbital nerve block is given at the infraorbital foramen or inside the infraorbital canal (Figure 21-17). The areas blocked include the incisive bone and maxilla, maxillary incisors, canine, and premolars/molars (depending how far the needle is advanced into the infraorbital canal) and adjacent soft tissues. The major palatine nerve block is given through the thick palatal mucosa just rostral to the major palatine foramen (Figure 21-18). The areas blocked include the palatine shelf of the maxilla and adjacent soft tissues. The inferior alveolar nerve block can be given intraorally (at a relatively flat angle through the alveolar mucosa at the lingual surface of the mandible) (Figure 21-19) or extraorally through the skin slightly rostral to the angular process at the medial side of the mandible. The areas blocked include the mandibular body, all mandibular teeth, and adjacent soft tissues. The middle mental nerve block is given through the lateral labial frenulum at the middle mental foramen halfway between the canine and third premolar (Figure 21-20). The areas blocked include the rostral mandibular body, teeth rostral to the injection site, and adjacent soft tissues.6,53,59,103
Periodontal Disease
Periodontal disease affects a majority of adult cats and involves inflammation and infection of the periodontium (gingiva, periodontal ligament, alveolar bone, and cementum) caused by plaque bacteria and the host’s response to the bacterial insult. Its systemic effects have been well documented in humans (heart disease and stroke, diabetes, respiratory disease, and increased risk of premature delivery and low-birth-weight infants) and are being increasingly investigated in companion animals.98
Gingivitis and Periodontitis
Gingivitis is reversible, affecting gingiva only (Figure 21-21). The gingiva may detach from the tooth, creating a periodontal pocket, and a shift occurs in the gingival flora from a gram-positive aerobic to a gram-negative anaerobic spectrum. Treatment of gingivitis requires plaque control, and daily toothbrushing can resolve gingivitis. In adolescent cats a particular form of gingivitis has been recognized. This so-called juvenile hyperplastic gingivitis occurs after eruption of the permanent dentition at about 6 to 8 months of age, with the inflamed gingiva being enlarged to a degree that it can cover the crowns of the teeth (Figure 21-22). It is not known whether juvenile hyperplastic gingivitis is a precursor form of more severe oral inflammation or whether it can progress to stomatitis in the adult cat. Gingival enlargement is also caused after administration of anticonvulsants, cyclosporine, and calcium channel blockers. Treatment of gingival hyperplasia involves cessation of its cause and removal of excess gingiva. Because most cat teeth have less than 2 mm of attached gingiva, gingival surgery should be carefully executed and is often reserved for canine teeth and teeth with significant gingival enlargement.8
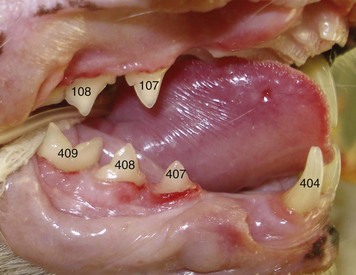
FIGURE 21-21 Gingivitis (worst at tooth 407) in a cat. The right maxillary canine and second premolar teeth are missing.
Periodontitis is the more severe form of periodontal disease, affecting all periodontal tissues and resulting in attachment loss, gingival recession, furcation exposure, periodontal pocket formation, and alveolar bone loss (Figure 21-23).69 Bacterial infection of the pulp is possible in areas devoid of cementum and through apical and non-apical ramifications. Alveolar bone loss is usually irreversible, causing the tooth to become mobile and ultimately to exfoliate.45 Similar to juvenile hyperplastic gingivitis, a so-called juvenile-onset periodontitis has been described in cats younger than 1 year of age.8 The teeth of such adolescent cats often are severely mobile on digital palpation and show most other clinical and radiographic signs associated with periodontitis.
Periodontal Therapy
Closed treatment may be sufficient when periodontal pocket depths do not exceed 2 mm in cats. Professional dental cleaning is performed with power scalers, followed by the use of hand scalers to remove residual calculus in pits, fissures, and developmental grooves of the crowns supragingivally and hand curettes to clean and plane exposed root surfaces subgingivally (Figure 21-24).64 Prevention of hypothermia is particularly important when water is used to cool power instruments or rinse debris from the mouth.44 Hand curettes can also be used for gingival curettage that removes the inflamed and infected soft tissue lining of the periodontal pocket. Once scaling is completed, the tooth surfaces are polished with fine polishing paste and a rubber cup on a prophy angle that is attached to a low-speed handpiece. Debris and polishing paste are rinsed from the tooth surface with water from an air–water syringe.45
Open treatment is usually indicated when pocket depths exceed 2 mm and is performed after reflection of a mucoperiosteal flap with or without vertical releasing incisions made into gingiva and alveolar mucosa. Osseous surgery and placement of implants are possible with this flap design.7 The flap is sutured closed with synthetic absorbable monofilament material such as poliglecaprone 25 (e.g., Monocryl, Ethicon). Lateral sliding flaps and free gingival graft techniques are available for treatment of gingival clefts. Medical therapy includes the use of topical rinsing solutions (e.g., 0.2% chlorhexidine) or systemic antimicrobials (e.g., amoxicillin–clavulanic acid, clindamycin). Because of potential side effects and the possibility of bacterial resistance, systemic antimicrobials should be used only in selected cases to serve as an adjunct to local treatment.25 Low-dose doxycycline gel (e.g., Doxirobe Gel, Pfizer Animal Health) may be inserted into cleaned periodontal pockets greater than 4 mm after root planing and gingival curettage.
Home Oral Hygiene
Plaque control is a critical component of periodontal disease prevention and in the maintenance of treatment success.17,18,25,104 The owner is given instructions on daily tooth brushing with a soft-bristled toothbrush and pet dentifrice.92 In addition, oral hygiene is enhanced by the use of treats, diets, and products that meet established criteria for effectiveness in mechanically or chemically controlling plaque or calculus deposition.36,40,56,115 For a list of approved products, please visit the website of the Veterinary Oral Health Council (http://vohc.org).
Tooth Resorption
Tooth resorption (previously called feline odontoclastic resorptive lesion [FORL]) affects 25% to 75% of cats, depending on the population of cats investigated and diagnostic tools applied. The condition usually involves multiple permanent teeth and can start anywhere on the tooth’s root surface.101 Chronic dietary intake of excess vitamin D has been suggested as one potential cause of tooth resorption in cats.99,100
Replacement Resorption and Inflammatory Resorption
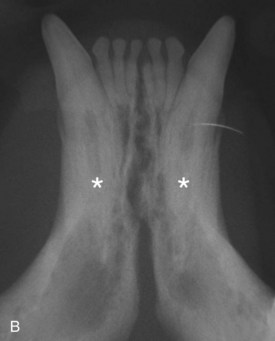
Feline teeth may appear clinically healthy, but they often show histologic and radiographic changes of periodontal and dental tissues, such as periodontal ligament degeneration, hypercementosis, and hyperosteoidosis. Narrowing of the periodontal space may result in ankylotic fusion (dentoalveolar anylosis) between the tooth and alveolar bone. These findings demonstrate events that occur before obvious tooth resorption and suggest that the very early lesion is probably noninflammatory.41 Ankylosed roots are at risk of being incorporated into the normal bone remodeling process, resulting in gradual resorption of the root and replacement by bone (replacement resorption) (Figure 21-25).100,101
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree