Chapter 52 Degenerative Skeletal Diseases of Primates
Osteoarthritis
Osteoarthritis refers to the pathologic failure of synovial joints characterized by the mechanical destruction of articular cartilage, with secondary changes in the subchondral bone (osteophytes, sclerosis, and eburnation). Morphologically, it is well established that human OA resembles the disease in baboons and macaques, which are used as experimental models.2,4,6 OA is distinct from erosive and infectious arthritis, in which cartilage dissolution and erosion of exposed bone surfaces are predominantly mediated by inflammatory changes in the synovial lining (pannus formation), without reactive bone proliferation (osteophytosis). No longer considered simply age-related or trauma-induced wear and tear, OA is the result of complex structural and biochemical changes in the synovial membrane and fluid, chondrocytes, collagen matrix and proteoglycans, and underlying cortical and cancellous bone.13 Additionally, genetic predispositions strongly influence the development of OA in humans.25 When no specific underlying condition is identified, the term primary osteoarthritis is used. Secondary osteoarthritis results when an underlying joint condition or systemic disease leads to premature joint degeneration.17 Previous extremity trauma is the most common predisposition in humans.8 Intra-articular fractures may result in incongruence of the articular surfaces, whereas extra-articular malunions may alter weight bearing, stance, gait, and joint loading. Ligament, tendon, meniscal, and muscle injuries will also affect biomechanics, especially if they result in joint instability. Similarly, osteomyelitis and septic arthritis, bleeding diatheses, crystal deposition diseases (e.g., gout), or osteonecrosis will change the physical characteristics of the articular surfaces of the bones, a risk factor for the development of OA.
Degenerative arthritis is recognized in free-ranging wild primates. Reported prevalence varies widely among studies, because data interpretation from wild specimens is often confounded by limited information on age, unknown history of injuries, and variation in observer interpretations. OA prevalence in wild great apes has been reported at 1% to 3%,9 although much higher frequencies have also been reported.5 Similar frequencies of OA were found in large studies of free-ranging prosimians (1.4%) and Old World (0.9%) and New World monkeys (1.5%).21,22
Assessing OA prevalence in wild populations is difficult because of the presumed impact of OA on survival. Selective pressures are likely to remove affected animals from the population rapidly. Captivity itself may play a role in the development of OA through alterations in environment, but this becomes difficult to evaluate because of the bias resulting from longer life expectancies in captive primates. Age is the most consistent risk factor for OA development in humans26 and similar increases in prevalence and severity with age has been noted in baboons and macaques.2,4,6 OA was found to be four and six times more common in captive Old World primates and prosimians, respectively.21 Another study found OA in 12.5% of captive New World primates, compared with only 1.5% of wild specimens.22 Housing may also play a role; captive macaques in a free-range setting had a higher prevalence and severity of OA than those in cages, possibly because of the protective trauma-free environment afforded by the cages.6,10
A higher incidence is seen in women and has been similarly reported in female rhesus macaques,2 as well as an increased incidence in females with higher parity.6 In humans, obesity is associated with earlier onset, increased prevalence, and more rapid progression of knee OA, but not necessarily hip OA.16 Body weight was not found to be an influence in two studies of NHPs2,4; however, it is uncommon for NHPs in research settings to display significant obesity.
Clinical Signs
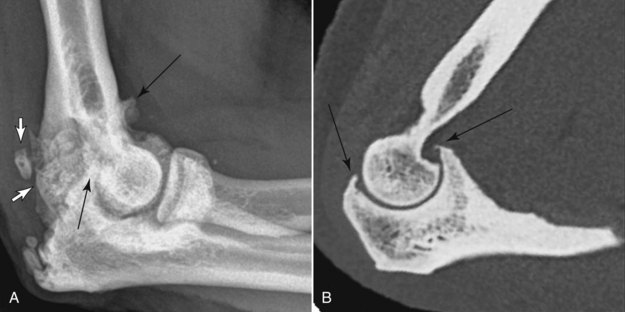
Signs of OA in NHPs may include alterations in gait, reluctance to walk and climb, appreciable lameness, and joint swelling.6,10 Pain is difficult to assess accurately, but the clinician should err on the side of assuming that pain is present when OA is suspected. In humans, although joint pain is the most common clinical manifestation of OA, not all arthritic joints are symptomatic, and the severity of pain does not necessarily correlate with radiologic or histologic findings. When present, the pain of osteoarthritis increases with activity and improves with rest. Stiffness and decreased range of motion are also common. Mechanical symptoms—catching, locking, clicking—often indicate a complication of the disease, such as the development of loose bodies. Instability and malalignment caused by OA typically only occur in end-stage disease. Because of an often stoic nature and inability to describe pain verbally, NHPs with severe radiologic changes (Fig. 52-1) may show only mild clinical signs of discomfort (see later).
Joints Affected
In humans, primary OA in the upper extremity most commonly affects the basal joints of the thumbs, proximal and distal interphalangeal joints of the fingers, and glenohumeral and acromioclavicular joints in the shoulder.17 Involvement of the elbows, metacarpophalangeal joints, and wrists is uncommon. In the lower extremities, hip, knee, and great toe metatarsophalangeal joint disease is most common. Spinal column OA occurs primarily in the facet joints of the lower cervical and lumbar spines, uncovertebral joints in the lower cervical spine, and the articulation between the anterior ring of C1 and the dens. Secondary osteoarthritis caused by trauma may afflict any joint, but most cases of OA in the ankles, hindfeet, midfeet, and elbows are post-traumatic. Atypical polyarticular distributions are often a clue to an underlying systemic condition.
In NHP, clear patterns of distribution are not as well defined, but several studies have noted similarities and differences from human patterns. As in humans, stifle, hip, interphalangeal, and spinal OA are common in NHP.6,10,21,22 In contrast, primary elbow OA is uncommon in humans, but is seen frequently in geriatric quadrupedal and arboreal NHPs (Fig. 52-2). Interestingly, the relative risk of OA affecting the thumb base was almost eight times higher in humans than in a colony of macaques.12 The more rudimentary NHP opposable thumb may be less prone to OA, because the evolutionary incongruence between joint design and altered functional demand in humans leads to increased OA. Studies in wild chimpanzees have shown OA to be more prevalent in the joints of the forelimbs than the hindlimbs.5
Skeletal distribution of OA may also differ between captive and wild NHPs. Among Old World primates, the elbow was more commonly affected in captive specimens and the knee more so in wild specimens.21 In captive New World monkeys, OA more commonly affected the shoulder, compared with the elbow and knee in free-ranging monkeys.22
Spondylosis
Understanding the general anatomy of the primate spine is important for understanding degenerative changes. The spine consists of multiple motion segments, each composed of an adjacent pair of vertebrae and the connective tissues between the two.18 Anteriorly, the vertebral body endplates are attached to the fibrocartilaginous disc through strong fibrous attachments called Sharpey’s fibers. Each disc has a fibrous annulus surrounding a spongy nucleus. Strong longitudinal ligaments run the length of the spine craniocaudally, attached to the anterior and posterior margins of the vertebral bodies and annulus fibrosus of the discs. Posteriorly, paired synovial facet joints are supported by the ligamentum flavum between the lamina and interspinous ligaments further dorsally. The orientation of the facet joints differs throughout the spine, so that the cervical spine motion segments demonstrate angular excursion (flexion-extension), rotation, and lateral bending, the lumbar spine shows angular excursion and lateral bending, and the thoracic spine is largely limited to a small amount of flexion-extension. The cervical spine also has specialized synovial joints in addition to the facets. These joints include the articulations between the lateral masses of C1 and C2 and the articulation between the anterior ring of the atlas and odontoid process, which allow for neck rotation.
The synovial joints in the spine are commonly affected by OA, analogous to the synovial joints in the extremities. In addition to pain and stiffness, facet and uncovertebral joint OA may result in radiculopathy in humans. The spinal nerves run adjacent to the joints, so osteophytes are an important cause of nerve compression.7 Based on large numbers of wild ape specimens, spinal degenerative disease was found to be significantly more prevalent in humans than apes.9 The human bipedal stance exerts greater compressive forces on the vertebral column than that seen in quadrupeds and may account for this disparity. Although quadrupedal for locomotion, many NHP still spend most of their time in an upright position.
Degenerative Disc Disease
Degeneration of the fibrocartilaginous interbody joints likely begins in the nucleus pulposus of the disc, which desiccates with age. As the process progresses, radially oriented tears occur within the annulus fibrosis. Herniated nucleus material may extend through these defects, protrude beyond the confines of the disc, or even extrude through the longitudinal ligaments. Gas clefts or calcification may develop in the degenerating discs. Collapse of the disc is a relatively late manifestation. These morphologic changes each affect the biomechanics of the motion segment. Specifically, loss of disc height and turgidity (often combined with facet joint osteoarthritis) increase the load in the vertebral endplates, and predispose to segmental hypermobility. The response of the endplates is marginal bone proliferation, similar to the formation of osteophytosis in synovial joint osteoarthritis.1 Like osteophytes, this endplate remodeling increases the weight-bearing surface area of the bone, decreasing strain. Formation of primarily horizontally oriented vertebral endplate remodeling may also be in response to stress from chronic pulling of the Sharpey’s fibers.
Baboons have been shown to be a natural model for human DDD, displaying similar disc space narrowing, endplate changes, and facet joint arthropathy.11 Severe kyphosis may be present in NHPs, seen first as a loss of spinal flexibility on physical examination and later as an obvious structural abnormality. As in humans, the process is correlated with age.
Degenerative disc disease in humans produces symptoms in a variety of ways.23 Provocative discography, in which a patient’s typical pain is reproduced by injection into the disc, has shown that some degenerated discs may be pain generators, even without disc herniation. Neurologic symptoms may result from endplate remodeling or disc herniation. In the cervical and thoracic spine, stenosis of the central canal caused by bone overgrowth or disc protrusion may cause cord compression and upper motor neuron symptoms, whereas in the lumbar spine lower motor neurons are usually affected after they have exited the cord, but are still in the neural canal; in humans, the conus medullaris is typically located at the L1-L2 level. Throughout the spine, posterolateral disc herniation and endplate remodeling often produce foraminal stenosis, impinging on exiting nerve roots and resulting in radicular pain and weakness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree