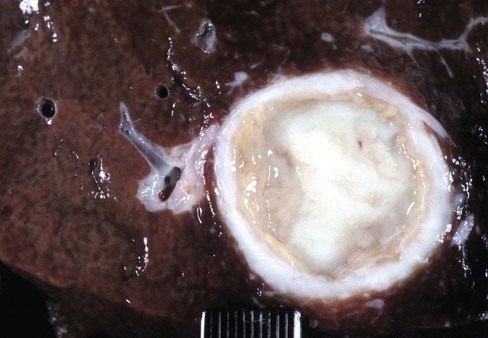
After completing this chapter, you will be able to • Describe and recognize clinical signs associated with specific diseases • Understand and describe the etiology of the diseases • Understand and describe common treatments of disease • Know the common and scientific names of parasites associated with these species • Know the common vaccinations and their schedules associated with these species See Chapter 13, Common Bovine Diseases. Clinical signs of infection often include dyspnea, tachypnea, cough, and weight loss. Diagnosis involves culture of the bacteria from a transtracheal wash. Thoracic radiographs may reveal masses in the thoracic cavity. Hepatic abscesses may be found upon necropsy (Fig. 17-1). The disease often causes abscessation of the lymph nodes. Identification and removal of sick animals from the herd can help control outbreaks. Sanitation during management practices such as castration, tail docking, and parturition can also help prevent infection. Vaccination is controversial. See Chapter 13, Common Bovine Diseases, for discussion of paratuberculosis (Figs. 17-2 and 17-3). Ewes or does are often infected by age 4 years. They seldom abort from toxoplasmosis in subsequent pregnancies. Prevention should include reducing cat access to sheep areas and equipment as well as preventing cats from eating placenta and tissue (Tables 17-1 and 17-2). TABLE 17-1
Common Ovine and Caprine Diseases
Bacterial Diseases
Anthrax
Caseous Lymphadenitis
Paratuberculosis (Johne Disease)

Other Microbial Diseases
Toxoplasma
Disease/Vaccination
Ewes
Lambs
Feedlot lambs
Rams
Comments
Clostridium perfringens type C
4–6 weeks before parturition
If animals have never been vaccinated, twice 4 weeks apart with last dose 4–6 weeks before parturition
If born to unvaccinated ewe, at birth and booster in 4–6 weeks
Lambs from vaccinated ewes should be vaccinated at 12–16 weeks and booster given in 4–6 weeks
Upon entering feedlot and booster in 2–4 weeks
Annually
Clostridium perfringens type D
4–6 weeks before parturition
If animals have never been vaccinated, twice 4 weeks apart with last dose 4–6 weeks before parturition
If born to unvaccinated ewe, at birth and booster in 4–6 weeks
Lambs from vaccinated ewes should be vaccinated at 12–16 weeks and booster given in 4–6 weeks
Upon entering feedlot and booster in 2–4 weeks
Annually
Clostridium tetani
Can be given during pregnancy with Clostridium types C and D
At time of castration and tail docking
Annually
Annually
Often combined with Clostridium types C and D
Other clostridial diseases (black disease, blackleg, malignant edema, struck, lamb dysentery, botulism)
4–6 weeks before parturition
If animals have never been vaccinated, twice 4 weeks apart with last dose 4–6 weeks before parturition
If born to unvaccinated ewe, at birth and booster in 4–6 weeks
Lambs from vaccinated ewes should be vaccinated at 12–16 weeks and booster given in 4–6 weeks
Annually
Annually
Primarily used only in high-risk herds
Leptospirosis
Primarily used only in high-risk herds
Sore mouth
At least 2 months before parturition, booster every 5–12 months depending on risk
1–2 days of age, booster every 5–12 months depending on risk
4 weeks before risk, booster every 5–12 months depending on risk
4 weeks before risk, booster every 5–12 months depending on risk
Live virus
Vaccinated sheep can spread the disease for up to 8 weeks after vaccination
Use in infected herds only
Performed by scratching skin in area without wool (inner ear or under tail in adults and inner thigh in young animals) and then brushing on the vaccine
Sores will form at application site
Foot rot
4 weeks before lambing, booster every 4–6 months
4 weeks of age, booster in 4–8 weeks
4 weeks before wet/rainy season, booster every 4–6 months
4 weeks before wet/rainy season, booster every 4–6 months
Vaccinate behind the ear
Only reduces infection levels
Abscesses are not uncommon, discoloration of the wool at the injection site
Booster in 4 weeks from first time of vaccination
Caseous lymphadenitis
Annually
Annually
Annually
Annually
Primarily used only in high-risk or infected herds
Booster in 4 weeks after the first dose
Enzootic abortion in ewes (EAE)
4 weeks before breeding
Do not use in pregnant ewes
Primarily used only in high-risk or infected herds
Toxoplasma
4 weeks before breeding
Do not use in pregnant ewes
Booster every 2 years
Primarily in only high-risk or infected herds.
Vaccine is not available in the United States
Vibriosis
Annually, 2 weeks before breeding
Booster in midpregnancy if first vaccination
Primarily used only in high-risk herds
Brucellosis
Rams test positive if vaccinated
Rabies
Common in pet sheep and possibly in endemic areas
Escherichia coli
4–6 weeks before parturition
If animals have never been vaccinated, twice 4 weeks apart
If ewes were unvaccinated, oral antibody can be given at birth
Primarily used only if diarrhea in 1- to 2-day-old lambs is a problem ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Common Ovine and Caprine Diseases



 years of age. The infection is thought to be result from contact with infected animals or the environment.
years of age. The infection is thought to be result from contact with infected animals or the environment.