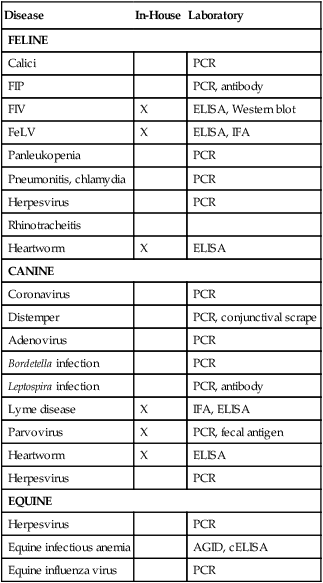
CHAPTER 23 Mastery of the content in this chapter will enable the reader to: • Identify common diseases and vaccinations. • Define diagnostic equipment and procedures. • Explain the importance of preanesthetic procedures. • Explain the importance of labeling medications. • Explain to owners how to administer medications. • Define the nutritional needs of puppies and kittens. • Differentiate therapeutic diets based on characteristics. It is the responsibility of all team members, but especially veterinary assistants and technicians, to check the patient into a room and obtain a complete history from the client. Chapter 14 provides detailed instructions on how to take an accurate history. It is very important to know if a pet has been vomiting or has diarrhea, how long it has had the presenting symptoms, and whether the owner can correlate any symptoms with abnormal events. The history taker must write down all the information provided by the owner; the details may provide a valuable tool for the doctor as an attempt is made to make a diagnosis. A good history taker is a valuable asset to the practice. If a muzzle is needed at any time, team members should not hesitate to use it (Figure 23-1). Muzzles are made to protect team members from being bitten! Some owners may argue that their pet does not need a muzzle; however, for everyone’s safety, including the owner’s, muzzles should be used. Both dog and cat muzzles are available and come in a variety of sizes. Muzzles should fit snugly on a dog’s nose. If the dog can open its mouth, the muzzle is too large, and the purpose of the muzzle is defeated. Cat muzzles should fit snugly over the entire head. Cat bags and towels may also be helpful to prevent team members from becoming scratched (Figure 23-2). The full cat body is placed inside the bag with only the head exposed. Most bags have two small openings that will allow front legs to be pulled through if needed. virus or bacteria that has been passed through a culture to reduce its virulence, whereas a killed vaccine introduces an inactivated virus into the body. Recombinant vaccines are available in two types. The first is the subunit vaccine, produced by a microorganism that has been engineered to make a protein, which then elicits an immune response in a target host. Another is the recombinant vector type, in which harmless genetic material from a disease-causing organism is inserted into a weakened virus or bacterium (the vector). When the vector organism replicates, the genetic material that was inserted elicits the desired immune response. A variety of combinations of vaccinations are available on the market; the preference rests with the veterinarian as to which combination to order. It is highly recommended to indicate in the medical record where the vaccine was given. Some vaccines may cause localized reactions, and if the location of administration has been documented in the record, vaccine reaction can be ruled in or ruled out. Stamps are available to chart the location easily (Figure 23-3). Boxes 23-1 through 23-3 are not a complete list of diseases, but rather a summary of diseases for which there are vaccines. A brief description of the disease and symptoms is also included. Some tests are available for in-house diagnostics to determine if a pet has a disease, whereas other tests need to be submitted to an outside laboratory for diagnostics. Table 23-1 summarizes tests available for diagnostics. Table 23-1 Tests Available for Common Diseases Laboratory tests may include in-house bloodwork or panels sent to an outside laboratory (see Chapter 9). In-house lab work may consist of complete blood count (CBC) and chemistries (both abbreviated and complete panels are available), heartworm tests, fecals, urinalyses, cytologies, FeLV/FIV tests, and parvovirus tests. A variety of companies produce a number of tests that are available for use in practice; the product insert should be used as a guide to completing each test correctly. Directions that are not followed correctly can yield inconclusive results, producing a false-positive or –negative result. Not only does this provide substandard medicine, it decreases the profits of the veterinary practice. Any failed tests should be repeated and reported to the practice manager in case the tests are tracked. It is imperative for the veterinary assistant and technician to become familiar with general tests that are run in-house. Clients will ask what test correlates with what bodily system, and these questions must be answered clearly and confidently. Table 23-2 lists the names of common tests and the system with which the test correlates. Table 23-2 Urine samples can provide a wealth of information for the veterinarian, and several tests can be performed on one sample. Most urine samples are obtained by free catch; either the owner has obtained a sample or an assistant has walked the dog and caught a midstream urine sample (Figures 23-4). Other methods of collection include cystocentesis or catheterization (Figure 23-5). If a urine sample will be sent to the laboratory for culture, a sample acquired by cystocentesis is highly recommended because it is a sterile sample that is obtained without any contamination. Cystocentesis is the process of inserting a needle into the bladder and withdrawing a sample. The tests that can be completed on urine are numerous; the most common tests completed in the hospital include specific gravity, stick urinalysis, and sediment (Boxes 23-4 and 23-5). The specific gravity provides the concentration of the urine and is a key indicator of how well the kidneys can concentrate the urine. Certain disease processes can affect the concentration, including renal disease and diabetes. A stick urinalysis is performed by dipping a urinalysis stick into the sample itself (if it is a sterile sample, the urine should be dropped onto each testing block) (Figure 23-6). The sediment is essential to verify the information provided by the stick. Electrocardiograms, often referred to as EKGs or ECGs, are recordings of the heart’s electrical activity. The recording traces the entire heartbeat process, through both the systolic and diastolic phases. Arrhythmias and conduction disturbances of the heart can be detected on ECGs, and an ECG is highly recommended before administering anesthesia to patients (Figure 23-7). Care must be taken when taking radiographs. Safety cannot be emphasized enough. Studies indicate that excess radiation causes cancer, birth defects, a decreased life span, and fertility issues. Protection must be worn at all times while taking radiographs (Box 23-6 and Figure 23-8). Lead thyroid collars, gowns, and gloves are the absolute minimum that should be provided to all team members allowed to take radiographs. Eye goggles are also a good idea (eyes cannot be replaced!) to provide ultimate protection. Team members who are exposed to radiation on a daily basis have a higher incidence of reproductive, thyroid, and eye cancers. Lead aprons, collars, and gloves should never be folded; any fold can crack the lead and allow radiation to penetrate the team member, decreasing safety (Figure 23-9). All apparel should be hung on a wall or laid flat on a table surface to prevent cracking. Aprons, collars, and gloves should be radiographed yearly to check for any cracks that may have appeared (Figure 23-10). Radiographs should be compared year to year, and safety equipment should be replaced as soon as visible cracks appear. Team member safety cannot be compromised. A radiology log can be helpful to team members when a digital system is not used. Figure 17-1 shows an example, listing the date, client and patient name, area being studied, position, and machine settings. This type of log allows team members to retrieve settings used in previous radiographs in case repeat or follow-up radiographs are required. To compare radiographs, the same setting should be used on both. Different settings may produce slight differences in quality of images, thereby making comparison difficult. Digital radiographs have setting information stored with the image, allowing exact settings to be used. Radiograph checkout logs should also be implemented when owners take x-rays for second opinions or when films are sent to a specialist. Figure 17-2 shows a log that allows radiographs to be traced if they have not been returned. After clients have received all appropriate education regarding the procedure and the risk of anesthesia, they must sign an anesthetic release. Examples of anesthetic release forms are provided in Chapter 2. It is imperative that the client’s phone number, cell phone, and/or pager be listed in case an emergency occurs and the client must be contacted during the procedure. Clients must be informed of the risks and benefits the pet is subject to before the procedure is performed. Informed consent ensures that the client has been advised, understands the risks, and agrees to the procedures elected. Chapter 4 defines informed consent in more detail. • Bloodwork: The very minimum that should be offered is bloodwork that evaluates the kidney and liver function, as well as red blood cells, white blood cells, and platelet function. Most manufacturers offer preoperative panels that include blood urea nitrogen, creatinine, alanine aminotransferase, alkaline phosphatase, glucose, total protein, and a complete blood count. Anesthesia is metabolized by the liver and kidneys; it is imperative to know if they are functioning correctly. If a patient is deficient in platelets, it is helpful to know this before surgery; a patient with low platelets could bleed to death. • ECG: An ECG is an excellent indicator of heart disease. An ECG will detect premature ventricular contractions or other abnormalities that may necessitate postponement of surgery. • IV catheter and fluids: If IV fluids are not a requirement of the practice, the owner should be strongly advised to permit them. IV fluids help maintain the patient’s blood pressure while under anesthesia, help support the kidneys, and allow an access port to the vein in case of emergency. If a patient goes into cardiac arrest while under anesthesia, drugs can be administered much faster through an existing line versus placing a catheter in an emergency. • Histopathology: If a patient is having a mass or growth removed, clients should be advised to send the growth to a pathologist to determine the correct pathology. Many cancerous tumors look benign but are not. A pathologist who reviews cytologies as a profession can make an informed diagnosis of masses submitted.

Clinical Assisting
EXAMINATIONS
Taking a History
Restraint

VACCINATIONS AND DISEASES

Common Diseases
Disease
In-House
Laboratory
FELINE
Calici
PCR
FIP
PCR, antibody
FIV
X
ELISA, Western blot
FeLV
X
ELISA, IFA
Panleukopenia
PCR
Pneumonitis, chlamydia
PCR
Herpesvirus
PCR
Rhinotracheitis
Heartworm
X
ELISA
CANINE
Coronavirus
PCR
Distemper
PCR, conjunctival scrape
Adenovirus
PCR
Bordetella infection
PCR
Leptospira infection
PCR, antibody
Lyme disease
X
IFA, ELISA
Parvovirus
X
PCR, fecal antigen
Heartworm
X
ELISA
Herpesvirus
PCR
EQUINE
Herpesvirus
PCR
Equine infectious anemia
AGID, cELISA
Equine influenza virus
PCR
DIAGNOSTICS
Bloodwork
Test
Associated With
AST
Liver
ALT
Liver
Total bili
Liver
Alk phos
Liver
GGT
Liver
Total protein
Protein
Albumin
Protein
Globulin
Protein
A/G ratio
Protein
Cholesterol
Lipids
BUN
Kidney
Creatinine
Kidney
BUN/crea ratio
Kidney
Phosphorus
Mineral
Calcium
Mineral
Glucose
Diabetes
Amylase
Pancreas
Lipase
Pancreas
Sodium
Electrolytes
Phosphorus
Electrolytes
Na/K ratio
Electrolytes
Chloride
Electrolytes
Triglycerides
Lipids
Magnesium
Mineral
WBC
White blood cell count
RBC
Red blood cell count
HGB
Hemoglobin concentration
HCT
Hematocrit
MCV
Mean corpuscular volume
MCH
Mean cell hemoglobin
MCHC
Mean cell hemoglobin concentration
Total T-4
Thyroid
T-4 equil. dialysis
Thyroid
TSH
Thyroid
Bile acids
Liver
Urinalysis

Electrocardiogram
DIAGNOSTIC IMAGING
Safety
Guidelines
SURGERY
Preanesthetic Documentation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine

 PRACTICE POINT
PRACTICE POINT
 PRACTICE POINT
PRACTICE POINT What Would You Do/Not Do?
What Would You Do/Not Do? PRACTICE POINT
PRACTICE POINT PRACTICE POINT
PRACTICE POINT





 PRACTICE POINT
PRACTICE POINT PRACTICE POINT
PRACTICE POINT