CHAPTER 73 Chemotherapy Administration
Administration of chemotherapy has become a common procedure in many general veterinary practices, necessitated by the incidence of neoplasia in our feline patients. Thirty per cent of all cats over the age of 10 will be diagnosed with some type of cancer.1 Many small animal and feline practices now are quite comfortable administering chemotherapy on-site rather than referring these patients to specialty hospitals. The increasing demand for veterinarians and their nursing staff to administer these drugs highlights the need for improved guidelines and more accurate information regarding chemotherapy administration for our feline patients. This chapter will cover basic chemotherapy safety and administration, as well as provide helpful charts, client handouts, and sedation protocols.
CHEMOTHERAPY SAFETY
Maintaining safe working conditions remains the highest priority for all veterinarians and nursing staff when administering chemotherapy. Many issues must be considered before the first dose of chemotherapy is administered. First, those individuals who are administering the chemotherapy are at the greatest risk for exposure. Women of childbearing age must use special caution when handling chemotherapy drugs, and women who are pregnant should be strongly discouraged from handling any chemotherapy drugs.2 Second, veterinary hospitals should have a standard operating procedure (SOP) in place for chemotherapy administration; all staff members should be familiar and comfortable with this document and should be able to locate it easily. In accordance with Occupational Safety and Health Administration (OSHA) guidelines, all nursing staff involved in the administration of hazardous drugs should wear the following protective gear:
Gloves: Veterinary hospitals can purchase specially made chemotherapy administration gloves. These gloves are thicker than the average latex glove and come in specific sizes for a better fit to enhance manual dexterity. If chemotherapy administration gloves are not available, latex gloves with minimal or no powder are preferred, because the powder can absorb contamination.3,4 Double-gloving is recommended to minimize the risk of exposure to hazardous drugs, when using latex gloves.3 Gloves always should be removed immediately if they are punctured, torn, or contaminated from a spill. Nursing staff always should wash their hands prior to putting the gloves on and again after they are removed.
The room in which chemotherapy is administered should be a low-traffic, quiet area with good ventilation and lighting. There should be no eating, drinking, smoking, chewing gum, applying cosmetics, or food storage where chemotherapy is prepared or administered. The preparation and administration of all chemotherapy drugs should be performed over a plastic-backed absorbable pad. A designated sharps container should be available for chemotherapy use only and labeled as such. The storage of chemotherapy drugs should be kept separate from other drugs and human food products. Areas housing chemotherapy drugs should be labeled clearly, and the drugs should be stored in bins with barrier fronts. If refrigeration is required, a separate unit should be used.5
It is always preferable to use Luer-Lok syringes to minimize the chances of aerosolization and chemotherapy spills. Never fill a syringe to more than 75 per cent of its capacity volume. This will minimize the chances of accidentally pulling the plunger out of the syringe resulting in a spill. If removing a needle and syringe from a bottle of chemotherapy drug is required, and a fume hood is not available, wrap a 70 per cent alcohol-soaked gauze around the chemotherapy bottle and needle. The alcohol-soaked gauze will serve as an absorptive barrier for any chemotherapy that may aerosolize from the bottle (Figure 73-1). As with any medication, accurate labeling of all syringes is crucial. When preparing a flushing syringe, it is best to use saline rather than a heparinized saline mixture because heparin precipitates with some chemotherapy agents. A chemotherapy dispensing pin can be used if mixing or reconstituting drugs is required (B. Braun Medical Inc, Bethlehem, PA). This “chemo-pin” has hydrophobic filters that help to equalize the pressure inside the bottle that is being mixed, further reducing the risk of exposure during mixing (Figure 73-2).
Most chemotherapy pills can not be broken and capsules should never be opened. However, chlorambucil, a commonly used chemotherapy drug for feline small cell gastrointestinal lymphoma, can be broken in half if necessary. Chlorambucil is available in 2-mg tablets. These tablets are coated and may be broken carefully for 1-mg dose increments. When prescribing more than one tablet per dose, it often is easiest to place the tablet (or tablet halves) in an empty clear gelatin capsule so that the entire dose may be administered at one time. All clients and staff members should wear gloves when handling or administering this medication, regardless of whether it is in a gelatin capsule. If tablets need to be cut in half, this ideally should be done under a hood. If no hood is available, this can be performed over an absorbent pad. The person handling the medication should wear a mask if pills are being broken into halves, and the area subsequently should be cleaned with diluted bleach. The absorbent pad should be discarded as chemotherapy waste along with the gloves and mask.6
Wherever chemotherapy drugs are being mixed or administered, a clearly labeled hazardous chemical spill kit should be easily accessible. All staff members should be aware of its contents, how to use the components, and how to clean up a spill properly. The American Society of Hospital Pharmacists (ASHP) recommends that kits contain the following items: one to two pairs of chemical splash goggles, two pairs of gloves, two pairs of utility gloves, a low-permeability gown, two (12″ × 12″) absorbent pads, a sharps container, a small scoop to collect glass fragments, and two hazardous drug disposal bags (Figure 73-3).3
RECORD KEEPING
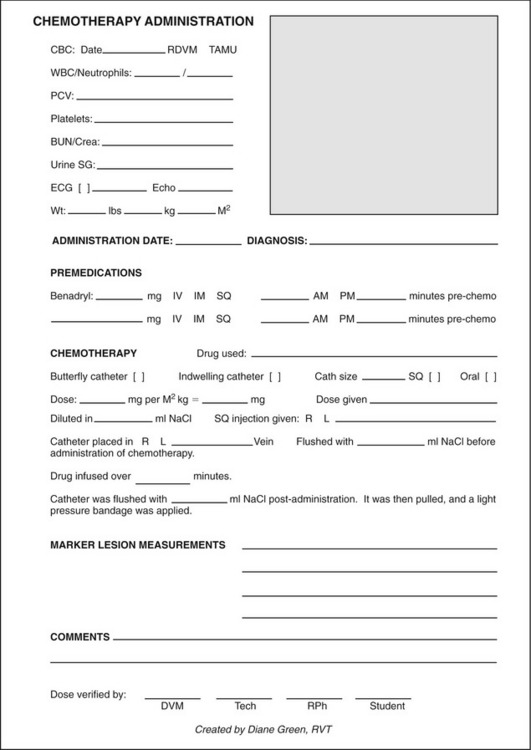
The chemotherapy administration form (Figure 73-4) is designed to have all the pertinent information on one sheet. The patient is identified (square shaded box located in the upper right corner of Figure 73-4), complete blood count and other pertinent test results can be recorded, and the patient’s weight in pounds (lb), kilograms (kg), and meter squared (m2) body surface area is recorded for each dose of chemotherapy. One should always refer to the kg to m2 conversion chart each time when calculating chemotherapy drugs that are administered based on body surface area (Table 73-1). If a patient’s weight in kg does not match precisely with the numbers on the chart, it is advisable to extrapolate between numbers and round the numbers down. There also is a section designated for recording any premedications, sedatives, or antihistamines that are administered. This form provides a place for listing the chemotherapy drug being administered, the route by which it was given, catheter placement information including location, and notes about marker lesion assessment. It also provides a site for the person(s) calculating the chemotherapy dose to initial or sign. Ideally more than one person should calculate and check the chemotherapy dose before administration. This form should be incorporated into the medical record at each visit, so that any comments or important information can be accessed conveniently.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree