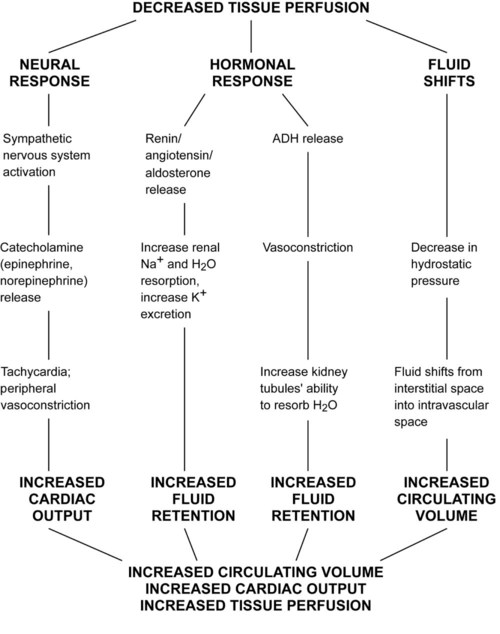
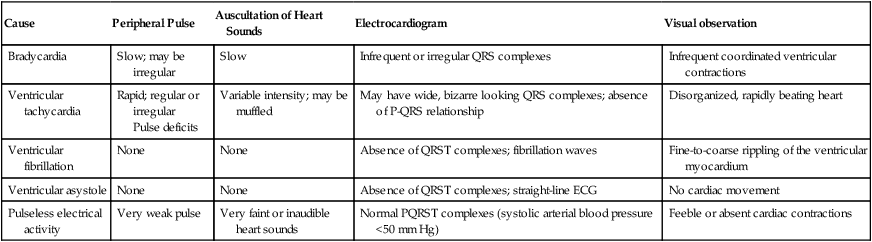
29 Most drugs used for anesthesia produce hypotension. Hypotension, cardiac arrhythmias (bradycardia, ventricular tachycardia), and decreased peripheral perfusion (low cardiac output) leading to shock can occur after the administration of sedatives and anesthetics. The potential for cardiac emergencies is increased in severely stressed, debilitated, or traumatized animals. A variety of physical and pharmacologic approaches have been developed to prevent or reverse deterioration of the circulation and reestablish normal hemodynamics. It is imperative to have a physical, technical, and working knowledge of the techniques and drugs used to provide successful cardiopulmonary resuscitation (CPR). Successful resuscitation should be followed by continuous intensive nursing care and close monitoring for 3 to 7 days (see acvecc-recover.org). I Definition: a cardiovascular emergency is any condition involving the heart or vasculature that results in the inability to maintain adequate blood flow, tissue perfusion, and oxygenation A Respiratory failure (hypoxia) 1. Hypoventilation (hypercarbia, increased PaCO2) 3. Ventilation-perfusion abnormalities 4. Intracardiac or pulmonary shunt 1. Respiratory acidosis (PaCO2 >60 mm Hg) 2. Metabolic acidosis (usually lactic acid) 3. Respiratory alkalosis (PaCO2 <35 mm Hg) 1. Hyperkalemia (bradycardia; poor contractility, vasodilation) 3. Hypocalcemia (hypocontractility, hypotension) 1. Increased sympathetic tone; increased myocardial automaticity and irritability 2. Increased parasympathetic tone; predisposition to bradycardia and various forms of heart block; predisposition to atrial arrhythmias, including atrial fibrillation 3. Increased sympathetic and parasympathetic tone; predisposition to ventricular arrhythmias E Hypothermia (35° C, 95° F; see Chapter 17) G Rapid, excessive, or inappropriate drug administration 1. Any hypersensitivity or drug overdose such as a hypotensive crisis caused by rate or amount of drug administered a. Most commonly observed after intravenous drug administration b. Treatment includes fluids, steroids, and occasionally vasopressors (i.e., epinephrine) c. Administration of catecholamines during inhalant anesthesia (ventricular arrhythmias, tachycardia) 2. Accidental intra-arterial drug administration (e.g., accidental intracarotid administration of preanesthetic drugs [phenothiazines, xylazine] in horses and cattle); treatment should include adequate padding, anticonvulsants (diazepam), fluids, and glucocorticosteroids 3. Myocardial depressant factors produced by ischemic organs (e.g., pancreas) 4. Species predisposition: Reports of adverse responses to anesthetic drugs are sometimes reported. The most notable is the postulated association of cardiac arrest after the administration of acepromazine to boxer dogs. The incidence or cause is unknown. H Cardiac disease and/or arrhythmias (Table 29-1; Fig. 29-1) TABLE 29-1 Distinguishing Characteristics of Several Types of Cardiac Failure or Arrest ECG, Electrocardiogram. 1. Cardiovascular collapse: cardiac failure that is unresponsive to therapy a. Occurs primarily in animals that have advanced heart disease or are inadvertently administered too much drug too quickly 2. Bradycardia: lower-than-acceptable heart rate a. Increased parasympathetic tone d. Specific medications (opioids, α2-agonists) e. Cardiac disease (e.g., cardiomyopathy, sick sinus syndrome, atrioventricular fibrosis) 3. Tachycardia: higher-than-acceptable heart rate 4. Atrial or ventricular arrhythmias (atrial tachycardia, ventricular tachycardia); associated with conditions that cause ischemia, hypoxia, hypotension, hypercarbia, metabolic acidosis or alkalosis, hyperkalemia, hypomagnesemia, hypothermia, or hypotension. Cardiac arrhythmias are also caused by surgical manipulation, anesthetic drugs, and cardiac catheterization. (1) Most likely to occur during hypoxia because of the instability of autonomic reflexes and endogenous release of catecholamines (2) Rarely associated with the administration of injectable or inhalant anesthetics (3) May follow severe hypercarbia, hypoxia, hypovolemia, acidosis, and/or hyperkalemia c. Ventricular asystole (lack of ventricular contraction) d. Pulseless electrical activity; electrocardiogram reading is present, but poor cardiac contraction produces low arterial blood pressure (mean arterial pressure <50 mm Hg). Electromechanical dissociation is a special type of pulseless electrical activity wherein ventricular contraction is uncoupled from electrical activation. I Weak or absent peripheral pulses II Irregular pulses or heart sounds III Cyanosis: faint blue or gray color in anemic (hemoglobin <5 g/dL) animals IV Poor perfusion; prolonged capillary refill time (>2 seconds) VI Abnormal breathing pattern or apnea (agonal breathing) VIII Depression, weight loss, or edema IX No bleeding from cut surfaces
Cardiovascular Emergencies
Overview
General Considerations
Cause
Peripheral Pulse
Auscultation of Heart Sounds
Electrocardiogram
Visual observation
Bradycardia
Slow; may be irregular
Slow
Infrequent or irregular QRS complexes
Infrequent coordinated ventricular contractions
Ventricular tachycardia
Rapid; regular or irregular
Pulse deficits
Variable intensity; may be muffled
May have wide, bizarre looking QRS complexes; absence of P-QRS relationship
Disorganized, rapidly beating heart
Ventricular fibrillation
None
None
Absence of QRST complexes; fibrillation waves
Fine-to-coarse rippling of the ventricular myocardium
Ventricular asystole
None
None
Absence of QRST complexes; straight-line ECG
No cardiac movement
Pulseless electrical activity
Very weak pulse
Very faint or inaudible heart sounds
Normal PQRST complexes (systolic arterial blood pressure <50 mm Hg)
Feeble or absent cardiac contractions
Indicators of Poor Cardiac Function