CHAPTER 55 Brain Tumors
Clinical Spectrum
INCIDENCE AND ETIOLOGY
The true incidence of feline brain tumors is unknown. Estimates from several studies suggest that feline brain tumors are relatively uncommon, ranging from 3.5 per 100,000 cases (0.0035 per cent) to as high as 4.6 per cent.1–3 However, data from these studies must be interpreted cautiously because they are derived from analyses of necropsy records, and may not reflect the true incidence in the population at large.
The etiology currently is unknown for most tumor types. With the exception of increased incidence of meningioma in young cats with mucopolysaccharidosis I,4 there are no studies in veterinary medicine that correlate genetic or environmental risk factors with intracranial neoplasia (see Chapter 56).
A recent retrospective study analyzed the frequency of different tumor types in a large cohort of cats with intracranial tumors.5 The medical records of 160 cats with an intracranial neoplasm identified at necropsy were analyzed (Table 55-1). The neoplasm was considered a primary brain tumor in 70 per cent of the cats, and classified as a secondary brain tumor in the remaining 30 per cent. As with other studies,1,3,6–12 meningioma was the most common tumor type identified, occurring in 58 per cent of the cats. The most common secondary tumors were lymphoma (16 per cent) and pituitary tumors (9.3 per cent). Metastatic brain tumors were identified in only nine of the 160 cats (5.6 per cent), whereas only six cats (3.8 per cent) had direct extension of a tumor into the brain.5 Compared with other tumor types, multiple meningiomas are fairly common in cats.3,10 Two or more discrete intracranial tumors of the same type (primarily meningiomas) were found in 16 of the cats (10 per cent). Another 16 cats (10 per cent) had two different histological types of intracranial tumors.5
Table 55-1 Top 10 Brain Tumors Identified in 228 Cats with 244 Brain Tumors*
| Tumor Type | Number | Frequency (%) |
|---|---|---|
| PRIMARY BRAIN TUMORS | ||
| Astrocytoma | 7 | 2.8 |
| Ependymoma | 7 | 2.8 |
| Meningioma | 144 | 59.0 |
| Olfactory neuroblastoma | 2 | 0.8 |
| Oligodendroglioma | 6 | 2.4 |
| SECONDARY BRAIN TUMORS | ||
| Hemangiosarcoma | 2 | 0.8 |
| Lymphoma | 39 | 16.0 |
| Nasal (adeno) carcinoma | 3 | 1.2 |
| Pituitary | 22 | 9.0 |
| Pulmonary adenocarcinoma | 3 | 1.2 |
* Adapted from Troxel MT, Vite CH, Van Winkle TJ, et al: Feline intracranial neoplasia: retrospective review of 160 cases (1985-2001), J Vet Intern Med 17:850, 2003.
Tumor location appears to be predictive of tumor type.5 In addition to expected relationships (e.g., meningioma in the meninges, pituitary tumor in the pituitary gland), third ventricular tumors are most likely to be meningiomas. Lymphoma was identified in all cats with either diffuse cerebral or diffuse brainstem involvement.
SIGNALMENT
Brain tumors have been reported in all ages and breeds of cats.5 Although there is a wide variation in age at presentation, most affected cats are older than 10 years of age.1,5–7,13–16 Male cats are affected more often by meningioma or pituitary tumor than female cats; however, a statistically significant difference has not been detected. No gender bias has been identified for other brain tumors.
CLINICAL SIGNS
Clinical signs of brain tumors are caused by primary or secondary effects of the lesion. Primary effects include direct compression of surrounding brain parenchyma or invasion into adjacent brain tissue. Secondary effects include edema, obstructive hydrocephalus, and hemorrhage.7,8
The duration of clinical signs is variable.7,13,14,16,17 Many cats are brought to a veterinarian for examination following an insidious onset of clinical signs with a chronic, progressive course, but an acute onset of clinical signs is possible. One study reported that an acute onset of clinical signs occurred in 15 per cent of affected cats,14 whereas another reported an overall median duration of clinical signs of only 21 days.5 A wide variety of clinical signs have been reported by owners, but the abnormalities reported most commonly include behavior changes, locomotor deficits (e.g., circling, pacing), and ataxia.5,7,13–15,17
Seizures reportedly are uncommon in cats with brain tumors compared with dogs.15 Two recent studies, however, found that seizures are among the most commonly recognized abnormalities noted by owners prior to presentation, with a frequency of 14 to 22.5 per cent.5,18 In one of these studies one third of the cats with a forebrain (cerebrum, thalamus) tumor had experienced seizures.18 Seizures were the first clinical sign observed by owners in 64 per cent of all cats with a brain tumor who had experienced seizures.18 It also was thought previously that cats with a structural brain lesion were more likely to have partial or complex partial seizures, whereas cats with metabolic or toxic diseases were more likely to have generalized seizures.19 A retrospective study of 61 cats with intracranial tumors found that 14 cats (23 per cent) had experienced seizure activity at the time of presentation. Ten of these 14 cats (71 per cent) had either generalized seizures only or both generalized and partial seizure activity. An additional cat experienced partial seizures with secondary generalization. Only three of the 14 cats (21.4 per cent) experienced partial seizures alone.18 These findings suggest that cats with brain tumors commonly experience generalized seizures.
Cats with nonspecific clinical signs are fairly common.1,5 One study found that 21 per cent of cats had no specific neurological signs at the time of presentation.5 The most commonly reported nonspecific signs are lethargy (20 per cent) and inappetence or anorexia (18 per cent).1,5
DIAGNOSIS
The following section describes common methods used to diagnose intracranial tumors, as well as brief descriptions of some techniques that are less sensitive and specific or are not utilized routinely. Histopathological examination remains the gold standard for diagnosis.7,8
NEUROLOGICAL EXAMINATION
A thorough and systematic neurological examination, as well as a complete general physical examination, should be performed on all cats who present with clinical signs referable to the nervous system. A description of the neurological examination can be found elsewhere.20 (See Chapter 49 in the fifth volume of this series for a discussion of the neurological examination of cats.) Goals of the neurological examination are twofold: (1) to determine whether the patient likely has neurological disease, and (2) to determine the likely location of disease. The clinical signs displayed by the cat and the results of the neurological examination reflect lesion location, rather than specific etiology (Table 55-2). Based on the patient’s signalment, history, and neurological examination findings, the practitioner then can formulate a differential diagnosis list and diagnostic plan.
Table 55-2 Clinical Signs Commonly Observed in Cats Based on Lesion Location
| Lesion Location | Possible Clinical Signs |
|---|---|
| Cerebrum, thalamus | Seizure, behavior change, altered mental status, circling, pacing, head pressing, head turn, contralateral postural reaction deficits, blindness |
| Brainstem | Altered mental status, circling, head tilt, nystagmus, ataxia, hemiparesis or tetraparesis, postural reaction deficits (contralateral most common, ipsilateral if rostral midbrain), dysphagia, cranial nerve deficits (III-XII possible), irregular respiration |
| Cerebellum | Cerebellar ataxia, truncal ataxia, hypermetria, intention tremors, broad-based stance, ipsilateral menace response deficit with normal vision and palpebral reflex, opisthotonus, vestibular signs |
MINIMUM DATABASE
The minimum database for diagnosis of neurological disease in cats includes a complete blood count, serum biochemical analyses, urinalysis, serum total T4, feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV) testing, thoracic radiographs, and systolic blood pressures.6–915 These tests rarely provide a definitive diagnosis for intracranial neoplasia. However, these tests help to exclude systemic or metabolic diseases that lead to secondary neurological signs. In addition, they are important preanesthetic screening tools, because many of the diagnostic methods used to diagnose brain tumors and other central nervous system (CNS) disorders require general anesthesia. Unlike cats with spinal lymphoma, cats with brain tumors, including lymphoma, have a low incidence of FeLV infection. In a recent retrospective study, less than 4 per cent of 160 cats with brain tumors tested positive for either FeLV or FIV.5 Abdominal radiographs or ultrasound should be performed if there are clinical signs or physical examination findings referable to the abdominal cavity.
ADVANCED IMAGING
Magnetic Resonance Imaging
The physics of MRI has been described in numerous publications and details can be found elsewhere.21 Briefly, MRI involves placing a patient in a scanner that has a large magnet. The protons (hydrogen nuclei) that are found in water molecules in the body align themselves with the magnetic field. Another electromagnetic field oscillates at specific radiofrequencies perpendicular to the main magnetic field, which pushes some of the protons out of alignment with the main magnetic field. As these protons return to their normal alignment with the main magnetic field, they emit a radiofrequency signal that is detected by a receiver. Protons in different tissue types throughout the body realign at different speeds. A computer analyzes these differences, and images are created based on the location and speed of realignment.21
MRI is the imaging modality of choice for detection of CNS lesions in human patients. The sensitivity for detection of brain tumors has been shown to be 98 to 99 per cent for human beings, dogs, and cats.22–24 MRI provides superior resolution of intracranial lesions compared with CT, and is more sensitive for detection of primary and secondary brain tumors, infarction, white matter diseases, subacute to chronic hemorrhage, and neurodegenerative diseases.25 Advantages of MRI over CT include the ability to produce high resolution images of soft-tissue structures, the acquisition of images in multiple planes without having to move the patient, lack of ionizing radiation, the ability to visualize edema easily, and lack of “beam-hardening” artifacts surrounding the brainstem and cerebellum that can obscure small lesions.21,25 Relative disadvantages compared with CT include increased cost, lower sensitivity in identifying bone lesions, calcification, acute hemorrhage, and longer scan time.21,25
MRI features of individual brain tumors have been described for several tumor types and will be discussed in additional detail below. Findings that appear to aid in the differentiation of neoplastic from nonneoplastic lesions include single lesion, regular shape (spheroid or ovoid), contact with the meninges, presence of a dural tail (extension of hyperintense signal or contrast enhancement along the meninges beyond the boundary of the lesion), lesions that affect the adjacent bone, and the presence of contrast enhancement.26
Computed Tomography
Computed tomographic images essentially are cross-sectional “slices” of the body utilizing x-ray technology. However, photon detection is much higher with CT compared with conventional radiographs; therefore slight differences in attenuation lead to improved contrast resolution.* Advantages of CT compared with MRI include shorter scan times; higher sensitivity for detection of bone lesions, calcification, and acute hemorrhage; and reduced cost.21,29 Disadvantages compared with MRI include exposure of the patient to large doses of radiation; decreased sensitivity for soft tissue structures; presence of bone artifacts created by thick bone surrounding the caudal fossa (brainstem and cerebellum), which can lead to inability to visualize lesions; and inability to easily obtain images in all planes without moving the patient.21,29 Description of CT features of large numbers of feline brain tumors primarily has been limited to meningioma,13,14,28,30,31 but small case series or case reports have described the use of CT for pituitary tumors,32–34 lymphoma,35–37 ependymoma,38 intracerebral plasma cell tumor,39 and middle-ear tumors extending into the brainstem.40
HISTOPATHOLOGICAL AND CYTOLOGICAL EXAMINATIONS
Although neurological examination findings and advanced imaging may lead to a strong presumptive diagnosis of intracranial neoplasia,5,24 histopathological examination remains the gold standard for definitive diagnosis.9 Tissue biopsy can be made via surgical or stereotactic techniques. Cytological examination of tissue specimens obtained at surgery or necropsy also may be useful in rapid diagnosis.41,42
ANCILLARY DIAGNOSTIC TESTS
Cerebrospinal Fluid Analysis
CSF analysis rarely provides a definitive diagnosis for brain tumor.16,43 It is used to aid in the diagnosis of CNS disease, but may not be necessary based on results of MRI or CT imaging.6 In general, CSF collection is very safe. However, space-occupying masses can lead to increased intracranial pressure (ICP), and the subsequent alteration of ICP with CSF drainage may lead to brain herniation.22 CSF collection should be performed after imaging whenever possible to evaluate potential risks versus benefits.6
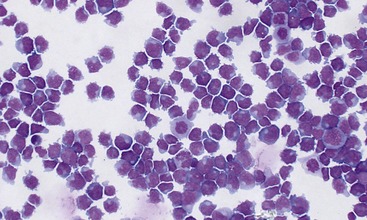
CSF analysis is very sensitive for identification of CNS disease, but is not specific to etiology with the exception of the occasional detection of lymphoblasts with CNS lymphoma (Figure 55-1), rare identification of tumor cells on CSF cytology, and identification of infectious organisms (e.g., Cryptococcus neoformans).5,37,43,44 There is a wide range of reported CSF results for various tumor types.† For example, one study found normal CSF in 3 of 10 cats with meningioma.17 CSF analysis was performed in 28 cats in a retrospective study of 160 cats with brain tumors. The median total protein was 38 mg/dL (range, 16 to 427; normal, <25) and the median nucleated cell count was 5 cells/µL (range, 0 to 162; normal, <5).5 Similar findings were reported in a retrospective study of CSF analyses of cats with noninflammatory CNS disease.44 Albuminocytologic dissociation (increased total protein without a concomitant increase in nucleated cell count) has been reported to occur with intracranial neoplasia. This abnormality was identified in eight (28.6 per cent) cats.5 However, albuminocytologic dissociation has been reported with other CNS disorders, including noninflammatory degeneration with tissue necrosis, vascular lesions with hemorrhage, and certain types of viral encephalitis.43
Skull Radiographs
In general, skull radiographs have limited value in the diagnosis of brain tumors, but may be of some assistance if advanced imaging is not available or cost-prohibitive to the owner. Routine views should include lateral and ventrodorsal (VD) or dorsoventral (DV) views. The closed-mouth VD view is best for evaluation of the frontal and prefrontal regions, whereas the open-mouthed VD view is best for evaluation of the nasal cavity. Open-mouth frontal view is best for evaluation of the foramen magnum and cerebellar region.27 Dorsoventral and right and left oblique DV views can be used to evaluate the tympanic bullae to rule out otitis media and ear tumors (see Chapter 31).15,27 Meningiomas lead frequently to thickening of the overlying calvaria (hyperostosis) that can be detected on skull radiographs, as well as with CT and MRI.5,17,28 Varying degrees of calcification within the tumor, enlargement of the middle meningeal artery, and rare invasion of the calvaria with localized destruction of bone also may be detected on routine skull radiographs.17
Electroencephalography
Electroencephalography (EEG) is the recording of spontaneous electrical activity from the cerebral cortex via subcutaneous or surface electrodes. A study analyzing EEG results from 201 dogs and six cats thought to have space-occupying lesions found that EEG recordings from all of the patients had abnormalities in at least one lead. However, there was no correlation between the side of the brain affected on EEG and lesion location in the 27 dogs that underwent necropsy (none of the cats underwent necropsy). A major limitation of the study was that none of the patients appeared to undergo advanced imaging, and only a small proportion of the patients underwent necropsy.47 Another smaller study of 10 cats with meningioma found that only 50 per cent of the cats had EEG abnormalities over the appropriate cerebral hemisphere. Two cats had normal EEG recordings, two cats had changes contralateral to lesion location, and one cat had abnormalities only on the right side despite a massive tumor distorting both sides of the brain. These studies suggest that EEG is sensitive for detecting a cerebral lesion, but not specific to lesion location.17
Ultrasound
Brain imaging with ultrasound is limited because of bone interference. However, it can be directed through an open fontanelle (primarily to diagnose hydrocephalus), or intraoperatively through a craniotomy window to assist with locating an intraparenchymal lesion and for ultrasound-guided biopsy.27
Other Diagnostic Tests
Many other diagnostic tools have been described in the literature, including magnetic resonance spectroscopy,27,48 electromyography (EMG),16 cerebral angiography,16,27 cavernous sinus venography,16,27 optic thecography,16,27 scintigraphy,16,27 and others. Many of these are performed infrequently because of the widespread availability and increased sensitivity of MRI and CT. Others (EMG) are performed uncommonly or are still in the early stages of use in veterinary neurology (MR spectroscopy).
TREATMENT
Treatment options generally fall into two categories: (1) symptomatic treatment and (2) definitive treatment. The goal of symptomatic treatment is to alleviate secondary effects of the brain tumor, whereas definitive treatment is aimed at eliminating the tumor or reducing tumor volume.49 There are few large scale studies describing treatment options for individual tumor types with the exception of meningioma. Additional information regarding treatment for individual tumor types is presented later in this chapter.
SYMPTOMATIC TREATMENT
Corticosteroids
Corticosteroids are the mainstay of symptomatic treatment.6–915 They are used primarily to reduce peritumoral edema and decrease CSF production, both of which help to lower ICP, alleviating clinical signs temporarily. Prednisone or prednisolone is used most commonly. The typical dose is 0.5 mg/kg PO q12h for 1 to 2 weeks, followed by tapering to the lowest effective dose. Once daily dosing may be required long term to control clinical signs.
Anticonvulsants
Phenobarbital is the first-line anticonvulsant in cats and should be started if seizures occur. The standard starting dose is 1 to 2 mg/kg PO q12h.7 Serum phenobarbital levels should be measured 2 weeks after initiating treatment or after any change in dose. The “therapeutic range” is 15 to 40 µg/mL. Although hepatotoxicity appears to be less common in cats compared with dogs, many neurologists prefer not to exceed 35 µg/mL to decrease the risk of inducing liver damage. Phenobarbital induces synthesis and release of liver enzymes, particularly alkaline phosphatase (ALP). Bile acid assays should be performed every 6 months to differentiate hepatotoxicity from normal increases in liver enzyme values. Bile acid assays, and possibly abdominal ultrasound and liver biopsy, also should be performed when there are clinical signs of liver dysfunction, compatible blood value alterations (e.g., increased liver enzymes, decreased blood urea nitrogen, decreased cholesterol, decreased albumin), or increasing serum phenobarbital levels without increasing doses of phenobarbital.
Potassium bromide (KBr) can be used if needed; however, a recent study found that almost 40 per cent of cats developed a cough and had clinical and radiographic features similar to those seen in feline asthma. One of the cats was euthanized because of the severity of coughing.50 Potassium bromide should be discontinued at the first sign of coughing in the feline patient.
Diazepam is a very effective anticonvulsant and at one time was the second choice for oral anticonvulsant therapy until several reports described acute, fulminant hepatic necrosis in some cats treated with oral diazepam.51–53 Oral diazepam can be used, but with extreme caution. Serum liver enzymes should be monitored at 1 week and at 1 month after initiation of treatment.54
A recent study evaluated levetiracetam (Keppra; 20 mg/kg PO q8h) as an adjunct to phenobarbital in a small group of cats with suspected idiopathic epilepsy. A good response (greater than 50 per cent reduction of seizures) was observed in seven of 10 cats. Side effects were transient and included lethargy and inappetence in two cats.55 Limited information is available regarding other anticonvulsants; however, there is anecdotal use of zonisamide (Zonegran; 5 to 10 mg/kg PO q12h) in cats with seizures and it appears to be well tolerated. (See Chapter 54 for further discussion of novel anticonvulsant therapies.)
DEFINITIVE TREATMENT
Surgery
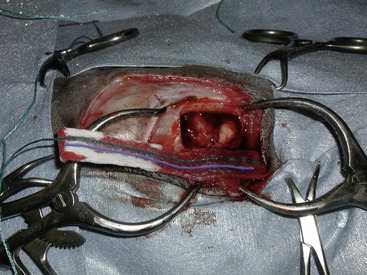
Excision of meningioma and other tumors that are surgically accessible is considered the gold standard for definitive treatment and should be performed whenever possible.7,15 Multiple studies have been published describing the surgical removal of meningioma in small case series, as well as individual case reports.5,13,14,17,30 In general, meningiomas (Figure 55-2) in cats are less invasive than in dogs and, as a result, they usually are easily excised.49 Sporadic case reports describe surgical excision of lymphoma,37 ependymoma,38,56 medulloblastoma,57,58 and aural tumors that extended into the brain.40 A recent report also describes the technique of transsphenoidal hypophysectomy for removal of pituitary gland tumors.34
Radiation Therapy
Along with surgical excision, radiation therapy (RT) can be an effective definitive treatment option for cats, and is becoming more widely available in veterinary medicine. Despite this, there are few reports describing its use in cats. Most of these reports describe use of RT in cats with pituitary tumors or intracranial lymphoma.32,33,37,59 Typically RT consists of 15 to 20 fractions of radiation to the tumor, requiring a brief (10 to 15 minute) anesthetic procedure each time. Administration of photons or electrons via linear accelerator is the most common form of RT in veterinary medicine, but some institutions use Cobalt-60 gamma radiation. DNA is damaged by the radiation in the targeted tissue. When the tumor cells attempt to divide, they are unable to replicate themselves and undergo cell death. For tumors that are dividing rapidly, the tumor will shrink sooner and a clinical effect is seen more quickly, whereas slow-growing tumors may take up to 3 to 4 months before clinical benefit is noted. Oral corticosteroids are often started prior to RT to help alleviate clinical signs. In general, patients who do not respond to corticosteroids prior to starting RT may not be acceptable candidates for RT, because it may take too long to see the beneficial effects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree