Chapter 101Bone Biomarkers
Bone is a complex tissue that undergoes change throughout life by the processes of bone formation by osteoblasts and bone resorption by osteoclasts.1 Modeling and subsequent remodeling of bone are required for bone health and allow the skeleton to respond rapidly to changes in its internal and external environment. Bone formation and resorption of bone are “coupled”2; the cycle of remodeling begins with the recruitment of osteoclasts, which attach to the bone surface and resorb the subjacent bone matrix. After osteoclasts evacuate a resorption pit, osteoblasts differentiate from mesenchymal precursors and fill in the lacuna with new bone matrix.3 In a healthy adult skeleton, formation and resorption are balanced. However, the balance is changed during growth, in response to altered exercise, by hormonal changes, during ageing, after therapeutic intervention, in metabolic bone disease, in neoplasia, and in response to injuries such as stress fractures.4-6 Changes in subchondral bone metabolism are also potentially important in the pathogenesis of osteoarthritis (OA).7,8 A challenge is to develop sensitive and specific noninvasive methods to detect changes in bone turnover in vivo. Abbreviations used in this chapter are summarized in Box 101-1.
BOX 101-1 Abbreviations
| ALP | Alkaline phosphatase |
| BALP | Bone-specific alkaline phosphatase |
| BGP | Bone gla-protein |
| BMD | Bone mineral density |
| CTX | Type I collagen C-terminal telopeptide |
| DEXA | Dual-energy x-ray absorbiometry |
| DMD | Dorsal metacarpal disease |
| DPD | Deoxypyridinoline |
| GGHyl | Glucosylgalactosylhydroxylysine |
| Ghyl | Galactosylhydroxylysine |
| HPLC | High-performance liquid chromatography |
| Hyp | Hydroxyproline |
| ICTP/CTX-MMP | Carboxy-terminal cross-linked telopeptide of type I collagen |
| IGF-1 | Insulin-like growth factor 1 |
| IRMA | Immunoradiometric assay |
| MRI | Magnetic resonance imaging |
| NTX | Type I collagen N-terminal telopeptide |
| OA | Osteoarthritis |
| OCa | Osteocalcin |
| PICP | Carboxy-terminal propeptide of type I collagen |
| PINP | Amino-terminal propeptide of type I collagen |
| PYR | Pyridinoline |
| QCT | Quantitative computed tomography |
| QUS | Quantitative ultrasound |
| RIA | Radioimmunoassay |
| WGL | Wheat germ lectin |
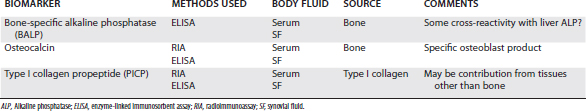
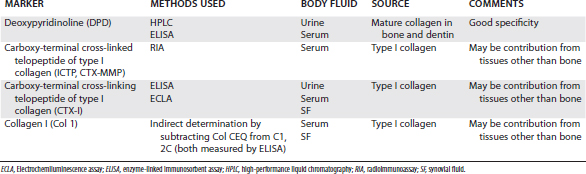
Bone biomarkers are generally classified as markers of bone formation or markers of bone resorption or degradation, although some reflect changes in both processes (Tables 101-1 and 101-2). In general, bone biomarkers are enzymes expressed by osteoblasts or osteoclasts or organic components released during the synthesis and resorption of bone matrix.15-17 However, many bone biomarkers are present in tissues other than bone and may therefore be influenced by other physiological processes. Because each biomarker may reflect a different physiological process, it is preferable to assay for a combination of markers, as this will provide more information on bone (re)modeling. However, human studies have shown that in certain diseases individual markers give more useful information than others,15 and the same may be true in horses. Other criteria that determine the value of any biochemical marker are whether the factors that control its synthesis and metabolic pathway are understood and what factors influence its biological variability. For many biomarkers used in human clinical studies, surprisingly little is known about the regulation of synthesis and metabolism, and in horses even less is understood about these variables.
Biomarkers That Reflect Changes in Bone Formation
Bone formation biomarkers are synthesized by osteoblasts and reflect different aspects of osteoblast activity. They are all measured in serum or plasma (see Table 101-1).
Biomarkers That Measure Changes in Bone Resorption
The majority of bone biomarkers that reflect osteoclastic resorption of bone matrix are degradation products of type I collagen (see Table 101-2). Originally, collagen-related resorption biomarkers were measured in urine samples collected over a 24-hour period, but in practice this is difficult in the horse. More recently developed resorption markers can be measured in serum and synovial fluid.