Chapter 7 Blood vascular system
The blood vascular system is made up of four parts:
Blood
Blood is a highly specialised fluid connective tissue (see Ch. 2), consisting of several types of cell suspended in a liquid medium called plasma. Blood makes up about 7% of the total body weight and has a pH of about 7.4. (7.35–7.45).
Functions
Transport
Regulation
Blood plays a vital role in homeostasis by regulating:
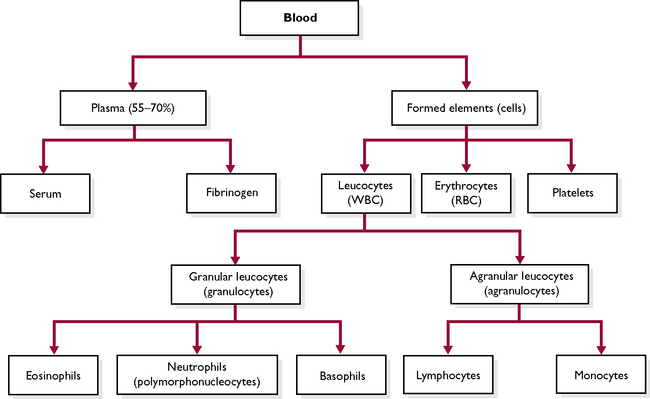
Composition of blood
Blood is a red fluid that is carried by the blood vessels of the circulatory system. It is composed of a fluid part, the plasma, and a solid part, the blood cells (Fig. 7.1). Plasma forms part of extracellular fluid (ECF) (see Ch. 1). Each constituent of the blood plays a specific part in the overall function of blood.
Plasma
In addition to these, plasma contains:
 Albumin: helps to maintain the osmotic concentration of the blood, i.e. holds the water in the blood
Albumin: helps to maintain the osmotic concentration of the blood, i.e. holds the water in the bloodBlood cells
The blood cells (Fig. 7.1) make up the solid component of blood and can be divided into three types:
Before studying the different types of blood cell it is useful to understand a number of terms.
Erythrocytes (or red blood cells)
Erythrocytes are the most numerous blood cell – there are about 6–8 million per cubic millilitre of blood (Fig. 7.2). Their function is to transport oxygen and a small proportion of carbon dioxide around the body (most carbon dioxide is carried in solution in the plasma).
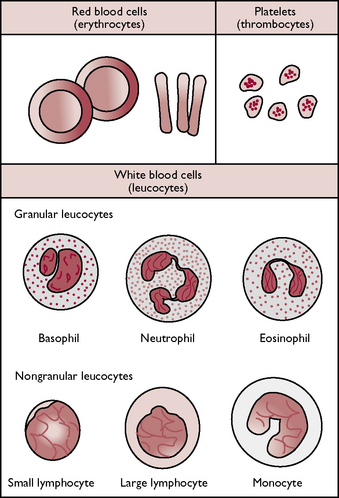
Fig. 7.2 The cellular components of blood.
(With permission from Colville T, Bassett JM 2001 Clinical anatomy and physiology for veterinary technicians. Mosby, St Louis, MO, p 197.)
The production of red blood cells is controlled by a hormone called erythropoietin (see Ch. 6), which is released by cells in the kidney in response to low oxygen levels in the tissues. Erythropoietin stimulates the stem cells in the bone marrow to produce more erythrocytes.
Leucocytes (or white blood cells)
Leucocytes are much less numerous than red blood cells and the cells contain nuclei. Leucocytes can be classified as either granulocytes or agranulocytes depending upon whether or not they have visible granules in their cytoplasm when stained and viewed under a microscope (Fig. 7.2). The function of leucocytes is to defend the body against infection.
Granulocytes
Agranulocytes
Agranulocytes have a clear cytoplasm. There are two types:
Blood clotting
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree