Chapter 15 Approach to Polyuria and Polydipsia
Normal Physiology
Polydipsia
c. Normal water intake is more variable than urine output because of variations in environmental conditions, dietary water intake, fecal water content, respiratory evaporative losses, age, and physiologic status (e.g., pregnancy, lactation).
d. Cats typically drink less water than dogs, and maximal water intake for normal cats is 45 mL/kg/day (20 mL/lb/day).
e. Measurement of water intake at home by the owner can be helpful to determine if PD is really present. This approach is practical primarily in dogs.
Pathophysiology
General Features
Mechanisms of Polyuria/Polydipsia
Hypothalamic Lesions
Loss of Renal Medullary Hypertonicity
a. The normal hypertonicity of the renal medulla is crucial for elaboration of highly concentrated urine. When medullary hypertonicity is decreased, the osmotic gradient necessary for movement of water from the collecting ducts into the interstitium and back into the bloodstream is disrupted, causing inappropriately dilute urine.
b. Although the major cause of impaired concentrating ability in chronic renal disease is the necessity to excrete the daily solute load with a decreased number of functional nephrons, several renal diseases are associated with structural (i.e., histopathologic) abnormalities that also can contribute to impaired concentrating ability.
c. Renal medullary washout of solute.
(1) Long-standing PU/PD of any cause can result in loss of medullary solutes (e.g., NaCl, urea) necessary for normal urinary concentrating ability.
(3) Increased medullary blood flow associated with long-standing PU/PD can accelerate removal of solutes by the systemic circulation.
(4) Decreased plasma osmolality associated with long-standing PPD impairs ADH release and the relative lack of ADH impairs reabsorption of urea by the inner medullary collecting ducts of the kidney.
(5) Aldosterone deficiency in hypoadrenocorticism impairs NaCl reabsorption in the collecting ducts and contributes to medullary washout of solute. This effect explains why dogs with hypoadrenocorticism often have impaired urinary concentrating ability at presentation despite having structurally normal kidneys.
2. Obligatory solute diuresis in the kidneys.
a. The filtered load of glucose in hyperglycemic diabetic patients exceeds the reabsorptive capacity of the renal tubules and results in an osmotic diuresis and glucosuria. Infusion of 5% or 10% dextrose in water can result in hyperglycemia and glucosuria. Rarely, a defect in renal tubular reabsorption of glucose (i.e., renal glucosuria) can be the cause.
b. To maintain fluid balance, the decreased number of functional nephrons in patients with chronic renal disease must excrete the normal daily solute load and thus function under conditions of solute diuresis which results in PU and impaired urinary concentrating ability.
Differential Diagnosis of Polyuria/Polydipsia
A. There are many causes of PU/PD in dogs and cats including renal disease and several endocrine diseases.
B. Diseases associated with PU/PD, the mechanisms of PU/PD in these diseases, and useful diagnostic tests are listed in Table 15-1. An eponym to remember the causes of PU/PD is presented in Table 15-2.
TABLE 15-1 Causes of Polyuria and Polydipsia With Mechanisms and Confirmatory Diagnostic Tests
| Disease | Mechanism of Polyuria and Polydipsia | Confirmatory Tests |
|---|---|---|
| Chronic renal disease∗ (S) | Osmotic diuresis in remnant nephrons | ECC |
| Disruption of medullary architecture by structural disease | CBC | |
| Profile | ||
| Urinalysis | ||
| Radiography | ||
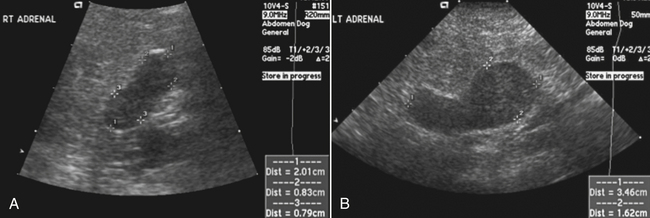
| Ultrasonography | ||
| Hyperadrenocorticism∗ (W) | Defective ADH release and action | LDDST, HDDST |
| Psychogenic | Plasma ACTH | |
| Ultrasonography | ||
| Diabetes mellitus∗ (S) | Osmotic diuresis caused by glucosuria | Blood glucose |
| Urinalysis | ||
| Hyperthyroidism∗ (W) | Increased medullary blood flow and MSW | T4 |
| Psychogenic | Technetium scan | |
| Hypercalciuria | ||
| Pyometra (W) | Escherichia coli endotoxin | History |
| Immune complex glomerulonephritis | Physical | |
| CBC | ||
| Abdominal radiographs | ||
| Postobstructive diuresis (S) | Elimination of retained solutes | History |
| Defective response to ADH | Physical examination | |
| Defective sodium reabsorption | Urinalysis | |
| Hypercalcemia (W) | Defective ADH action | Serum calcium |
| Increased medullary blood flow | ||
| Impaired NaCl transport in loop of Henle | ||
| Hypercalcemic nephropathy | ||
| Direct stimulation of thirst center | ||
| Liver disease (W) | Decreased urea synthesis with loss of medullary solute | Liver enzymes |
| Decreased metabolism of endogenous hormones (e.g., cortisol, aldosterone) | Serum bile acids | |
| Psychogenic (hepatic encephalopathy) | Liver biopsy | |
| Hypokalemia | Blood ammonia | |
| Pyelonephritis (W) | E. coli endotoxin | Urinalysis |
| Increased renal blood flow | Urine culture | |
| MSW | CBC | |
| Renal parenchymal damage | Excretory urography | |
| Ultrasonography | ||
| Hypoadrenocorticism (W) | Renal sodium loss with MSW | Serum Na and K |
| ACTH stimulation | ||
| Hypokalemia (W) | Defective ADH action | Serum K |
| Increased medullary blood flow and loss of medullary solute | ||
| Diuretic phase of oliguric ARF (S) | Elimination of retained solutes | History |
| Defective sodium reabsorption | CBC | |
| Profile | ||
| Urinalysis | ||
| Ultrasonography | ||
| Renal biopsy | ||
| Partial urinary tract obstruction (S) | Redistribution of renal blood flow | History |
| Defective sodium reabsorption | Physical examination | |
| Renal parenchymal damage | ||
| Drugs (W) | Various mechanisms depending on drug | History |
| Salt administration (S) | Osmotic diuresis caused by excess sodium administered | History |
| Excessive parenteral fluid administration (W) (polyuria only) | Water diuresis caused by excess water administered | History |
| Central diabetes insipidus (CDI) (W) | Congenital lack of ADH (rare) | Water deprivation test |
| Acquired lack of ADH (idiopathic, tumor, trauma) | Exogenous ADH test | |
| ADH assay | ||
| Nephrogenic diabetes insipidus (NDI) (W) | Congenital lack of renal response to ADH (very rare) | Water deprivation test |
| Acquired lack of renal response to ADH | Exogenous ADH test | |
| ADH assay | ||
| ECC | ||
| Psychogenic polydipsia (PPD) (W) | Neurobehavioral disorder (anxiety?) | Water deprivation test |
| Increased renal blood flow | Exogenous ADH test | |
| MSW | Behavioral history | |
| Renal glucosuria (S) | Solute diuresis caused by glucosuria | Blood glucose |
| Urinalysis | ||
| Primary hypoparathyroidism (W) | Unknown (psychogenic?) | Serum calcium |
| Serum phosphorus | ||
| Serum PTH | ||
| Acromegaly (W, S) | Insulin antagonism | Neuroradiography |
| Glucose intolerance | Insulin-like growth factor | |
| Diabetes mellitus in affected cats | ||
| Polycythemia (W) | Unknown (increased blood viscosity?) | CBC |
| Multiple myeloma (W) | Unknown (increased blood viscosity?) | Serum electrophoresis |
| Renal MSW (W) | Depletion of medullary interstitial solute (urea, sodium, potassium) | Gradual water deprivation (3-5 days) |
| Hickey-Hare test |
ACTH, adrenocorticotropic hormone; ADH, antidiuretic hormone; ARF, acute renal failure; CBC, complete blood count; ECC, endogenous creatinine clearance; HDDST, high dose dexamethasone suppression test; LDDST, low dose dexamethasone suppression test; MSW, medullary washout of solute; PTH, parathyroid hormone; (S), solute diuresis; (W), water diuresis.
∗ Most common causes of polyuria and polydipsia.
Adapted from Bruyette DS, Nelson RW: How to approach the problems of polyuria and polydipsia, Vet Med 81:112-128, 1986.
TABLE 15-2 Differential Diagnoses to Be Considered With Polyuria/Polydipsia
| C | Calcium, Cushing, Cancer, Corticosteroids |
| L | Liver insufficiency, Leptospirosis (subacute) |
| A | Adrenal (hyperadrenocorticism and hypoadrenocorticism) |
| M | Metabolic, Mellitus (Diabetes), Malignancy, Medullary washout |
| P | Psychogenic, Pituitary, Polycythemia, Pyometra, Portosystemic shunt, Partial urinary obstruction, Paraneoplastic (hypoglycemia), Postictal |
| E | Endocrine, Electrolytes (increased or decreased calcium, decreased potassium) |
| D | Drugs, Diabetes, Diuresis (post-obstructive, hypertension-induced) |
| R | Renal insufficiency/failure |
| I | Insipidus (nephrogenic, central) |
| B | Brain |
| S | Salty treats, Salty diets |