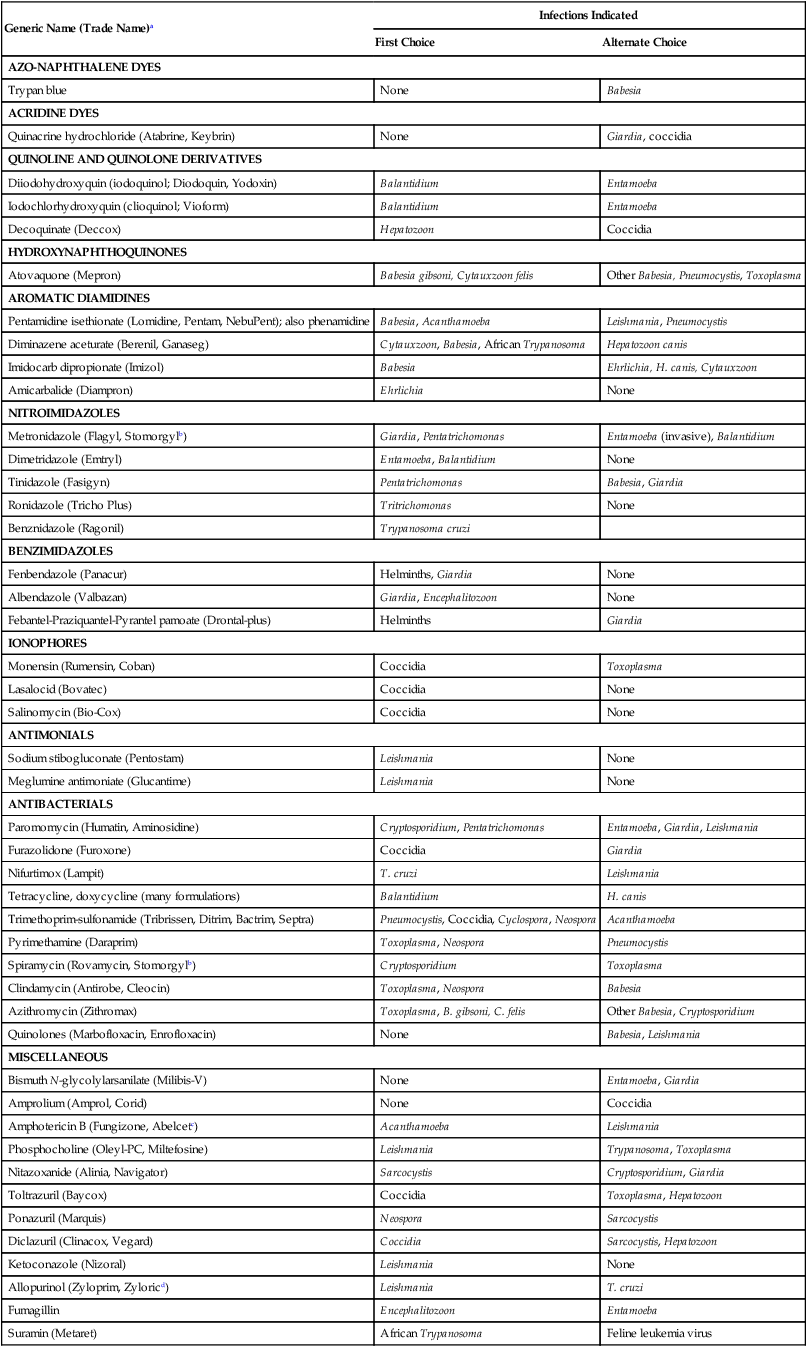
Table 71-1 summarizes the indications for current antiprotozoal drugs. See Chapters 72 to 81 for details about chemotherapy for specific diseases. Dosages of various drugs are available in the Drug Formulary in the Appendix. TABLE 71-1 Properties of Antiprotozoal Drugs aSee the Drug Formulary in the Appendix for additional information on these drugs. bCombination of metronidazole (25, 125, 250 mg) with spiramycin (46.9, 234, 469 mg) in tablets. cLipid formulations preferred. Trypan blue was one of the first compounds used to treat babesiosis. Because local irritation and abscesses develop after subcutaneous injection, it is administered intravenously. Trypan blue does not completely eliminate Babesia organisms, but infected animals recover from illness and remain in a state of premunition. They must be treated with aromatic diamidines (see Aromatic Diamidines) within 1 month to be cured. A disadvantage of trypan blue is that it stains all body tissues and secretions for several weeks. Diiodohydroxyquin and iodochlorhydroxyquin are halogenated oxyquinolines that have been provided as topical antifungal drugs. They are also amebicidal when administered orally. They are not absorbed systemically and have relatively low toxicity. Signs of toxicity are abdominal pain, diarrhea, and neurologic signs, all of which have been reported in dogs. Atovaquone is a closely related hydroxynaphthoquinone derivative licensed to treat Pneumocystis species infections. It has been used in combination with azithromycin to treat babesiosis in humans and dogs (see Chapter 76).79 Buparvaquone, which has been used to treat theileriosis in herbivores, has not effectively treated leishmaniasis or cytauxzoonosis in dogs or cats, respectively.165 Decoquinate, a hydroxyquinolone licensed for treating coccidiosis in poultry, is effective in ameliorating the signs of hepatozoonosis (see Chapter 74 and the Drug Formulary in the Appendix).94 Phenamidine, pentamidine, diminazene, amicarbalide, and imidocarb, which are diamidine derivatives, are the drugs of choice for treating Babesia, Cytauxzoon, and African Trypanosoma species infections in dogs and cats. They also effectively treat some other protozoa (see Table 71-1) by interfering with nucleic acid metabolism. These drugs are formulated as salts to reduce irritation after parenteral (intramuscular or subcutaneous) injection. Pentamidine has also been used to treat leishmaniasis.135 Derivatives of pentamidine have shown high in vitro efficacy against a North American isolate of Leishmania.139 Aromatic diamidines have some of the highest activity against Babesia gibsoni infection; however, drug resistance can develop.70a,101 Although imidocarb has been recommended to treat Hepatozoon canis and Cytauxzoon felis infections, incomplete responses have been noted26a,144a, and other drugs should be considered first (see Table 71-1). Nitroimidazoles are effective against anaerobic enteric protozoa that cause trichomoniasis, amebiasis, giardiasis, and balantidiasis. They can be used to treat intraintestinal and invasive parasites. The nitro group within anaerobic protozoa and bacteria undergoes a reduction to produce various unstable metabolites, some of which have antimicrobial activity. The drugs are generally much less effective against microaerophilic or aerobic microorganisms. Metronidazole, tinidazole, ronidazole, ipronidazole, nimorazole, dimetridazole, secnidazole, and ornidazole are close structural analogs marketed in various regions of the world. Fexinidazole is in clinical trials for treatment of African trypanosomiasis.160b See the Drug Formulary in the Appendix for further information on tinidazole, ronidazole, ipronidazole, and metronidazole. Metronidazole is the most widely used of these compounds. For example, it has no in vitro activity against nonanaerobic protozoa such as Leishmania. It has shown therapeutic benefit, especially in resolution of cutaneous lesions in infected dogs, when used in combination with other drugs such as enrofloxacin.14,17 In addition to protozoa, it is active against obligate spore-forming anaerobes such as Clostridium, some non-spore-forming anaerobes such as Campylobacter, and microaerophilic organisms such as species belonging to the Enterobacteriaceae. Metronidazole is generally preferred for treating giardiasis.150 Giardia infections that are resistant to metronidazole have been effectively treated by combining treatment with quinacrine.113 Metronidazole is the drug of choice for treating invasive amebiasis in humans. Metronidazole has been administered alone and with spiramycin to treat periodontal disease and stomatitis and leishmaniasis124 and in combination with aminoglycosides to treat mixed infections associated with bowel perforation and intra-abdominal sepsis (see Chapter 88). In humans the drug effectively treats intra-abdominal, pelvic, pleuropulmonary, central nervous system, and bone and joint infections. Side effects of metronidazole include gastrointestinal irritation with signs of vomiting and anorexia, glossitis, and stomatitis. Neurologic signs may be seen in dogs and cats after 7 to 10 days of treatment with high dosages (greater than 66 mg/kg/day) and may be resolved when therapy is discontinued.23 Some dogs have developed fatal encephalopathy, persistent seizures, or cerebellar and central vestibular ataxia after therapy; diazepam helped the dogs recover (see the Drug Formulary in the Appendix).38 Metronidazole is also mutagenic,150a as are other members of this class of drugs, and precautions must be taken to avoid their use in pregnant or neonatal animals. Fenbendazole and albendazole are broad-spectrum benzimidazoles that are used to treat a wide range of infections with helminths and selected protozoa. They affect microtubule synthesis in the protozoal cytoskeleton. Both drugs have been effective in the treatment of intestinal giardiasis and are often more potent than metronidazole.56 Fenbendazole is relatively safe, and dosages used for treating helminths (50 mg/kg for 3 days) are effective in treating giardiasis.56,149,149 The drug was not as effective in cats that were co-infected with Cryptosporidium.76 Fenbendazole use was associated with development of granulocytopenia as an idiosyncratic reaction in one dog.45 Myelotoxicity has been caused by albendazole use in dogs and cats157 but can be reversed after treatment is discontinued. Febantel, which is metabolized to fenbendazole, is one component of an anthelmintic combination that is effective against Giardia.10,123 The antifungal drugs ketoconazole, fluconazole, and terbinafine have some antileishmanial activity, because the infecting organism has ergosterol in its cell wall. In experimental animal models, these drugs have been less effective than other antiprotozoal drugs. The newer triazoles, such as posaconazole, have activity against Trypanosoma cruzi, as does a newer more potent derivative, albaconazole, that has been used in infected dogs.58 Another antifungal, amphotericin B (AMB), has been more effective (see Miscellaneous Drugs, later). Sodium stibogluconate and meglumine antimoniate are pentavalent antimony compounds and two of the main agents used in the treatment of leishmaniasis.52,151,160–162 The dosage is based on the amount of antimony compound administered. Treatment with these drugs is not curative, and two or three courses may be necessary. Combination therapy with other drugs has been recommended.154 Side effects include anorexia, vomiting, nausea, myalgia, and lethargy. Electrocardiogram abnormalities and nephrotoxicity can develop at higher dosages. Although these antimonials are often given parenterally, a cyclodextrin formulation was found to have good bioavailability in mice.29 Liposomal formulations have been investigated as a means of improving efficacy and reducing toxicity (see the Drug Formulary in the Appendix).136 Paromomycin (aminosidine) and furazolidone are nonabsorbable antibacterials (previously discussed; see Chapter 30. They are effective in treating some intestinal protozoal infections. Because of potential intestinal absorption and nephrotoxicity, paromomycin—an aminoglycoside—must be administered with caution when treating amebiasis or trichomoniasis when bowel lesions are extensive. Paromomycin has also been used to treat leishmaniasis. Furazolidone and sulfonamides are effective in treating intestinal coccidial infections. Nifurtimox, a nitrofuran derivative, can suppress but not cure T. cruzi infections. Nausea, vomiting, and convulsions may be side effects. Quinolones, such as marbofloxacin and enrofloxacin, have been used, often in combination, to treat dogs with leishmaniasis and babesiosis.88,117 Trimethoprim, an antibacterial diaminopyrimidine compound that inhibits folic acid synthesis, has broad-spectrum antimicrobial activity (see Chapter 30). Combined with sulfonamides, it has been used to treat Pneumocystis and coccidial infections. Pyrimethamine is closely related to trimethoprim but is more effective against protozoa. It has been used in combination with sulfonamides to treat infections with Neospora and Toxoplasma organisms. Several newer antifolate drugs under development may also be active against these two protozoa. Clindamycin, a lincosamide antimicrobial drug, and certain macrolides (azithromycin, clarithromycin) are also active against these two protozoa (see Chapter 79).26a,33 Spiramycin, a macrolide antibiotic, has an antibacterial spectrum similar to that of erythromycin but is less effective. Absorption after oral administration is adequate for therapeutic purposes. It is widely distributed and reaches high concentrations in tissues, from which it is slowly eliminated in the bile and urine. Its usefulness has been limited for treating bacterial infections in veterinary medicine, but it is now marketed in combination with metronidazole, primarily to treat periodontal and oral infections. Spiramycin has been found to be somewhat effective for treating intestinal cryptosporidiosis and has been given to humans to treat acute toxoplasmosis. (See the Drug Formulary in the Appendix.)
Antiprotozoal Chemotherapy
Generic Name (Trade Name)a
Infections Indicated
First Choice
Alternate Choice
AZO-NAPHTHALENE DYES
Trypan blue
None
Babesia
ACRIDINE DYES
Quinacrine hydrochloride (Atabrine, Keybrin)
None
Giardia, coccidia
QUINOLINE AND QUINOLONE DERIVATIVES
Diiodohydroxyquin (iodoquinol; Diodoquin, Yodoxin)
Balantidium
Entamoeba
Iodochlorhydroxyquin (clioquinol; Vioform)
Balantidium
Entamoeba
Decoquinate (Deccox)
Hepatozoon
Coccidia
HYDROXYNAPHTHOQUINONES
Atovaquone (Mepron)
Babesia gibsoni, Cytauxzoon felis
Other Babesia, Pneumocystis, Toxoplasma
AROMATIC DIAMIDINES
Pentamidine isethionate (Lomidine, Pentam, NebuPent); also phenamidine
Babesia, Acanthamoeba
Leishmania, Pneumocystis
Diminazene aceturate (Berenil, Ganaseg)
Cytauxzoon, Babesia, African Trypanosoma
Hepatozoon canis
Imidocarb dipropionate (Imizol)
Babesia
Ehrlichia, H. canis, Cytauxzoon
Amicarbalide (Diampron)
Ehrlichia
None
NITROIMIDAZOLES
Metronidazole (Flagyl, Stomorgylb)
Giardia, Pentatrichomonas
Entamoeba (invasive), Balantidium
Dimetridazole (Emtryl)
Entamoeba, Balantidium
None
Tinidazole (Fasigyn)
Pentatrichomonas
Babesia, Giardia
Ronidazole (Tricho Plus)
Tritrichomonas
None
Benznidazole (Ragonil)
Trypanosoma cruzi
BENZIMIDAZOLES
Fenbendazole (Panacur)
Helminths, Giardia
None
Albendazole (Valbazan)
Giardia, Encephalitozoon
None
Febantel-Praziquantel-Pyrantel pamoate (Drontal-plus)
Helminths
Giardia
IONOPHORES
Monensin (Rumensin, Coban)
Coccidia
Toxoplasma
Lasalocid (Bovatec)
Coccidia
None
Salinomycin (Bio-Cox)
Coccidia
None
ANTIMONIALS
Sodium stibogluconate (Pentostam)
Leishmania
None
Meglumine antimoniate (Glucantime)
Leishmania
None
ANTIBACTERIALS
Paromomycin (Humatin, Aminosidine)
Cryptosporidium, Pentatrichomonas
Entamoeba, Giardia, Leishmania
Furazolidone (Furoxone)
Coccidia
Giardia
Nifurtimox (Lampit)
T. cruzi
Leishmania
Tetracycline, doxycycline (many formulations)
Balantidium
H. canis
Trimethoprim-sulfonamide (Tribrissen, Ditrim, Bactrim, Septra)
Pneumocystis, Coccidia, Cyclospora, Neospora
Acanthamoeba
Pyrimethamine (Daraprim)
Toxoplasma, Neospora
Pneumocystis
Spiramycin (Rovamycin, Stomorgylb)
Cryptosporidium
Toxoplasma
Clindamycin (Antirobe, Cleocin)
Toxoplasma, Neospora
Babesia
Azithromycin (Zithromax)
Toxoplasma, B. gibsoni, C. felis
Other Babesia, Cryptosporidium
Quinolones (Marbofloxacin, Enrofloxacin)
None
Babesia, Leishmania
MISCELLANEOUS
Bismuth N-glycolylarsanilate (Milibis-V)
None
Entamoeba, Giardia
Amprolium (Amprol, Corid)
None
Coccidia
Amphotericin B (Fungizone, Abelcetc)
Acanthamoeba
Leishmania
Phosphocholine (Oleyl-PC, Miltefosine)
Leishmania
Trypanosoma, Toxoplasma
Nitazoxanide (Alinia, Navigator)
Sarcocystis
Cryptosporidium, Giardia
Toltrazuril (Baycox)
Coccidia
Toxoplasma, Hepatozoon
Ponazuril (Marquis)
Neospora
Sarcocystis
Diclazuril (Clinacox, Vegard)
Coccidia
Sarcocystis, Hepatozoon
Ketoconazole (Nizoral)
Leishmania
None
Allopurinol (Zyloprim, Zyloricd)
Leishmania
T. cruzi
Fumagillin
Encephalitozoon
Entamoeba
Suramin (Metaret)
African Trypanosoma
Feline leukemia virus
Interferon-γd
Leishmania
None
Azo-Naphthalene Drugs
Quinoline and Quinolone Derivatives
Aromatic Diamidines
Nitroimidazoles
Benzimidazoles
Azoles
Antimonials
Antibacterials
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


