CHAPTER 21 Antiemetic Therapy
PHYSIOLOGY OF EMESIS
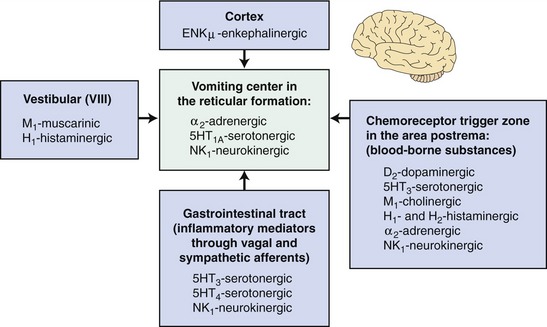
It is crucial to remember these pathophysiological concepts when treating vomiting symptomatically because the efficacy of antiemetic agents depends on the presence of the respective neurotransmitters and their receptors in the brain. Specific receptors of neurotransmitters that have been detected in the brain of cats include dopamine (D2-dopaminergic receptors), norepinephrine (α2-adrenergic receptors), 5-hydroxytryptamine (5-HT-serotonergic receptors), acetylcholine (M1-cholinergic receptors), histamine (H1– and H2-histaminergic receptors), and enkephalins (enkµ- and enkδ-enkephalinergic receptors).1 Currently, there are no data available regarding the presence of neurokinin1 receptors (NK1-receptors) in the brain of cats. However, it is reasonable to assume that NK1-receptors are present in cats because of the documented effectiveness of NK1-inhibitors as antiemetic agents in that species (Figure 21-1).2
ANTIEMETIC AGENTS
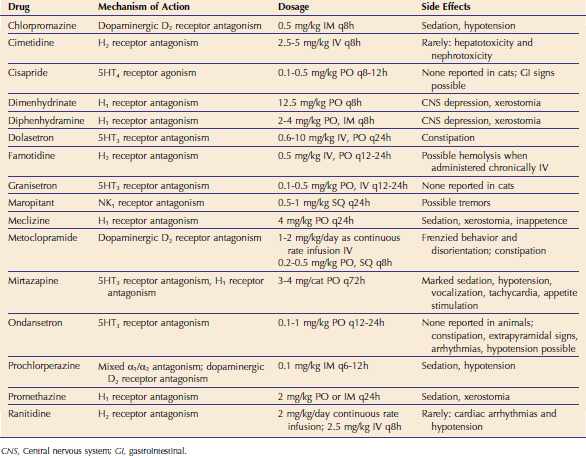
Many antiemetic agents have been used traditionally in cats, and a summary of these agents along with their mechanism of action, recommended dosage, and side effects can be found in Table 21-1. However, it is important to remember that there are species-specific differences in the distribution of receptors in the brain, which may explain why some agents that have been shown to be effective in dogs are not effective in cats. A discussion of the various classes of antiemetics is provided to highlight the rationale for the use of these agents to treat vomiting in cats in different clinical situations.
α2-ADRENERGIC ANTAGONISTS
Xylazine is the classic α2-adrenergic agonist, which has potent emetic effects in cats but not in dogs. Many of the research models used to investigate the efficacy of antiemetic agents in cats are based on triggering vomiting by the administration of xylazine.3–5 Antiemetic agents with good efficacy at the α2-adrenergic receptors in the vomiting center include pure α2-antagonists such as yohimbine, or mixed α1/α2-antagonists such as prochlorperazine and chlorpromazine.3 The latter two are in the drug class of phenothiazines, which also have weak antagonistic effects on H1– and H2-receptors, M1-cholinergic receptors, and D2-dopaminergic receptors. Promethazine is another phenothiazine drug with antiemetic effects. There is evidence that NK1-inhibitors can override the effect of xylazine on α2-adrenergic receptors and provide good antiemetic efficacy.5 Adverse effects possibly associated with drugs in this class include sedation and anticholinergic effects (e.g., dry mucous membranes).
D2-DOPAMINERGIC ANTAGONISTS
Apomorphine is an emetic agent that acts specifically on D2-dopaminergic receptors in the dog brain.3 However, apomorphine is not a very effective emetic agent in cats, which is why it is believed that D2-dopaminergic antagonists, such as metoclopramide, play a minor role as antiemetic agents in that species.3,4 However, peripheral effects of D2-dopaminergic antagonists in the gut, such as improved intestinal motility, may provide some antiemetic effects, but this has not been evaluated properly in cats. The exact action of metoclopramide in the gut is not known, but it appears that it sensitizes the upper gastrointestinal smooth muscle to the action of acetylcholine.3 In cats, adverse reactions to metoclopramide include signs of frenzied behavior, disorientation, and constipation.
H1– AND H2-HISTAMINERGIC ANTAGONISTS
H1– and H2-histaminergic receptors have been demonstrated in the CRTZ in dogs and are believed to play a significant role in emesis in this species.1 Antihistamines, such as dimenhydrinate and diphenhydramine, have been used widely to treat emesis, particularly related to motion sickness. The exact mechanism of action relating histamine receptor antagonism to an antiemetic effect is unknown, but these drugs appear to inhibit vestibular stimulation.3 The presence of histamine receptors in the CRTZ has not yet been demonstrated in cats, and histamine receptor antagonists are not considered very effective in this species. Also, cats are believed to be relatively resistant to the emetic effects of histamine. Adverse reactions seen with antihistamines in general include central nervous system (CNS) depression, anticholinergic effects (e.g., dry mouth, urinary retention), and gastrointestinal disturbances (e.g., vomiting, diarrhea).
Piperazine antihistamines, such as meclizine, are believed to have a separate antiemetic effect in addition to their antihistaminergic effect; however, the mechanism of action is not completely understood.6 It has been proposed that meclizine has central anticholinergic and CNS-depressant activity, particularly in the CRTZ, which may be responsible for its antiemetic effects. Adverse effects include sedation and, less frequently, anticholinergic effects (e.g., dry mucous membranes) and inappetence (especially in cats).
M1-MUSCARINERGIC ANTAGONISTS
M1-muscarinergic receptors and the neurotransmitter acetylcholine both have been demonstrated in the vestibular apparatus of cats.1 Mixed M1/M2-receptor antagonists such as atropine and scopolamine, as well as pure M1-receptor antagonists such as pirenzepine, have been used traditionally for the treatment of motion sickness in cats.1 It is unclear, however, if the main action of these compounds is through muscarinic receptors alone or also through other pathways. This fact, as well as the side effects of sedation, xerostomia, and possible intestinal ileus, makes their use less preferable.1
5HT3-SEROTONERGIC ANTAGONISTS
The central emetic effects of chemotherapeutic agents such as cisplatin are mediated through 5HT3-serotonergic receptors in the CRTZ in cats.1 Additionally, there are 5HT3-receptors found peripherally on vagal nerve terminals.1 It is unclear if the antiemetic effects of 5HT3-antagonists are solely mediated centrally or if there are peripheral effects also. 5HT3-selective antagonists such as ondansetron, dolasetron, and granisetron have been used widely for the treatment of chemotherapy-induced vomiting in cats and are believed to be very effective for this indication.7,8 These agents also are reportedly effective when given preventively before administering the chemotherapeutic drug.7,8 Advantages of some of these agents include infrequent dosing and the potential for parenteral administration.
A newer agent with some 5HT3-serotonergic antagonistic effect is the tetracyclic antidepressant, mirtazapine. The antidepressant activity of mirtazapine appears to be mediated via antagonism of central presynaptic α2 receptors, resulting in a net increase of norepinephrine, and this may contribute to its reported appetite-stimulating effects6 (see Chapter 12). In addition, mirtazapine antagonizes several 5HT receptor subtypes and also histamine receptors (H1). These effects are believed to be responsible for its antiemetic and antinauseant effects. The prominent sedative side effects of mirtazapine are related to its activity at H1 receptors, while activity on peripheral α1-adrenergic antagonism may explain the orthostatic hypotension associated with its use.6 Other reported side effects include vocalization and tachycardia.6 An important feature of mirtazapine metabolism is its dependence on glucuronidation for elimination. Because cats have limited capacity of glucuronidation, particularly when there is hepatic dysfunction, dosing intervals should be no more frequent than once every 72 hours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree