24 Anesthetic Agents
Preanesthetic Medications
Anticholinergics
Atropine Sulfate
Atropine sulfate (0.02 to 0.04 mg/kg) can be administered intramuscularly, subcutaneously, or intravenously. The duration of action is 60 to 90 minutes. Atropine may stimulate vagal nuclei in the medulla and cause an initial bradycardia before the desired effect is seen, particularly when the drug is administered intravenously. Other central effects of atropine include depression, restlessness, and delirium. Atropine administration may cause cardiac arrhythmias and sinus tachycardia. Atropine does cross the placental barrier and may lead to central and peripheral anticholinergic effects in the fetus when administered to the dam. Arrhythmias are more common after intravenous administration and include second-degree atrioventricular block, unifocal ventricular premature contractions, and ventricular bigeminy.1 Atropine is contraindicated in animals with preexisting tachycardia.
Glycopyrrolate
Glycopyrrolate is a synthetic quaternary ammonium anticholinergic. Glycopyrrolate may be given intramuscularly, subcutaneously, or intravenously at a dose of 0.011 mg/kg. The duration of action of vagal inhibition is 2 to 4 hours, significantly longer than with atropine. The antisialagogue effect may persist for up to 7 hours. The cardiovascular effects of glycopyrrolate are similar to those of atropine. Because of its large structure, glycopyrrolate does not cross the blood–brain or placental barrier readily and therefore has minimal central or fetal effects.2
Tranquilizers
Acepromazine
Acepromazine (0.05 to 0.1 mg/kg intravenously, intramuscularly, or subcutaneously, not to exceed a total dose of 3 mg; oral dose is 1 to 2 mg/kg), a phenothiazine tranquilizer, is used commonly as a premedication before general anesthesia in dogs and cats to relieve anxiety. Through depression of the reticular activating system and antidopaminergic actions in the central nervous system (CNS), acepromazine produces mental calming, decreased motor activity, and increased threshold for responding to external stimuli. Acepromazine does not produce analgesia but may act synergistically when administered concurrently with other drugs with analgesic activity. Administration of acepromazine will decrease the dose of subsequent anesthetic agents. Other effects include antiemetic activity and antihistaminergic properties. Hypotension and hypothermia can result from depression of vasomotor reflexes. Acepromazine is metabolized by the liver and should not be used in patients with liver disease. Because of the potential for hypotension, acepromazine should be used cautiously in compromised patients, particularly those with significant cardiovascular disease. Acepromazine may inhibit platelet function and should be avoided in patients with coagulopathies.2
In many veterinary textbooks, authors cautioned against the use of acepromazine in animals at risk for seizures. Recently, this caution is being questioned on account of a lack of references. In two retrospective studies, no evidence was found that acepromazine lowered the seizure threshold in dogs with a history of seizure disorders.3,4 It was further concluded that a controlled prospective study is necessary for a more thorough evaluation of the use of acepromazine both in this patient population and in the general canine population.
Diazepam
Diazepam (0.1 to 0.2 mg/kg intravenously) is a benzodiazepine tranquilizer that possesses muscle relaxant and anticonvulsant properties. Benzodiazepines exert their effect by enhancing the CNS inhibitory neurotransmitters gamma-aminobutyric acid (GABA) and glycine and by combining with CNS benzodiazepine receptors.1 Diazepam may produce a mild calming effect in some patients, but agitation and excitement can also occur. Diazepam is solubilized by mixing with propylene glycol. Diazepam has minimal cardiovascular effects; bradycardia and hypotension may be seen after rapid intravenous administration. Propylene glycol is associated with pain on injection and incompatibility when mixed in the same syringe with other drugs. Clinical uses of diazepam in small animal anesthesia include providing muscle relaxation when given concurrently with dissociative anesthetics and as a co-induction agent with injectable anesthetics (thiopental, propofol, etomidate) to decrease their doses or side effects (or both). The effects of diazepam can be reversed with the benzodiazepine antagonist flumazenil.
Midazolam
Midazolam (0.1 to 0.2 mg/kg intravenously and intramuscularly) is a benzodiazepine tranquilizer with behavioral effects and clinical uses similar to those of diazepam. Midazolam is more potent and has a shorter duration of action than diazepam. Midazolam is water soluble at a pH of 3.5. At a pH above 4, the chemical structure changes to become lipid soluble.5 Unlike diazepam, midazolam can be mixed with other anesthetic agents and can be administered intramuscularly without causing irritation. Flumazenil can be used to antagonize the effects of midazolam.
Opioids
Opioids act by combining with one or more specific receptors in the brain and spinal cord to produce analgesia, sedation, euphoria, dysphoria, and excitement. The mu receptors are thought to mediate supraspinal analgesia, respiratory depression, and euphoria. Kappa receptors mediate spinal analgesia, miosis, dysphoria, and sedation; the sigma receptors mediate hallucinations, psychomimetic activity, and respiratory and vasomotor stimulation. Delta receptors are thought to primarily modify mu receptor activity.1 Opioids are classified as agonists, agonist–antagonists, or antagonists according to their receptor activity.
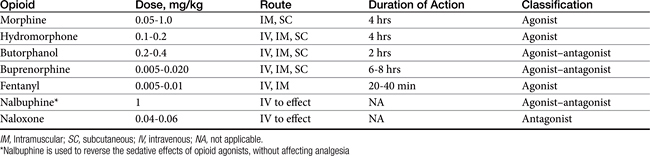
Opioids, agonists or agonist–antagonists, are used before, during, and after surgery in dogs and cats to provide analgesia. Certain opioids may produce sedation in some patients. The antagonists are used to reverse the effects of the agonists or agonist–antagonists. The opioid chosen is based on the degree and duration of expected pain and physical status of the patient. Understanding the differences between the commonly used opioids and their possible side effects are also important when choosing which drug to use. Dose, route, classification, and duration of action of the commonly used opioids in dogs and cats during the perioperative period are shown in Table 24-1.
The most common side effects of opioids preanesthesia include bradycardia and second-degree atrioventricular blockade. These effects may be prevented or treated with an anticholinergic agent. When given as a preanesthetic medication, certain opioids may cause vomiting. It is more commonly seen after administration of a mu agonist (morphine, hydromorphone). Respiratory depression can also occur, especially at high doses. The respiratory depressant effects may be additive to those caused by inhalant anesthetic agents. The user should be prepared to assist or control ventilation if necessary. This is especially crucial in patients with suspected space-occupying masses or lesions of the brain. Hypercapnia resulting from respiratory depression causes cerebral vasodilation and can lead to a life-threatening increase in intracranial pressure. The opioids can cause histamine release and should not be used before intradermal skin testing for allergies.
Alpha2-Adrenergic Agents
The alpha2-adrenergic agonists are used to produce sedation, muscle relaxation, and analgesia in dogs and cats by stimulating presynaptic alpha2-adrenoreceptors and causing a decrease in norepinephrine release both centrally and peripherally. This action leads to a decrease in both CNS sympathetic outflow and circulating catecholamines.2 Cardiopulmonary effects can be significant with these drugs and include respiratory depression, bradycardia, first- or second-degree atrioventricular blockade, decreased cardiac output, and increased peripheral vascular resistance. Because of these effects, careful patient monitoring should be employed after administering these drugs in dogs and cats. Alpha2-adrenergic agonists should not be used in compromised patients. Other effects seen with the use of alpha2-adrenergic agonists include vomiting, hyperglycemia, decreased gut motility, and dieresis. The commonly used drugs are xylazine, medetomidine, and dexmedetomidine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree