Chapter 85Analgesia and Hindlimb Lameness
Technique for Epidural Administration
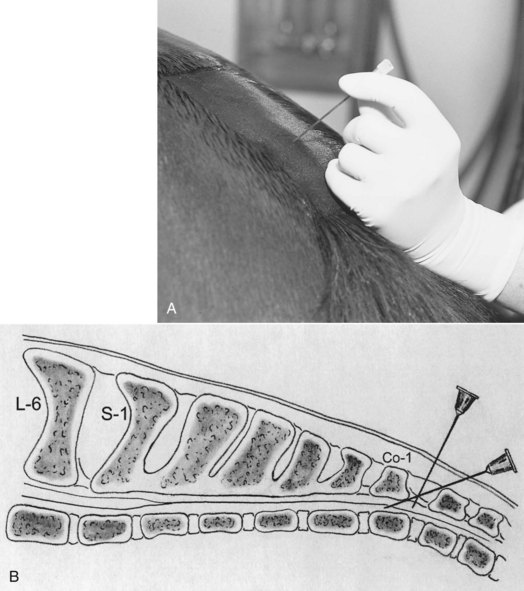
The first coccygeal interspace (between the first and second coccygeal vertebrae) is identified while raising and lowering the tail and palpating for the articulation between these two vertebrae. This space is just caudal to the most angular portion of the bend of the tail, about 5 cm cranial to the first long tail hairs (Figure 85-1). The site should be prepared aseptically. Administration of 2 to 3 mL of 2% lidocaine subcutaneously using a 25-gauge needle helps decrease the response of the horse to placement of the needle for epidural injection. An 18- or 20-gauge, 6.35-cm spinal needle with stylet is recommended for epidural injection in horses, although many clinicians use a standard 18-gauge needle. The bevel of a spinal needle is not as sharp as that of a standard needle and the bevel angle is less acute. This design makes it easier to identify penetration through the interarcuate ligament and the subsequent loss of resistance as the epidural space is entered. The needle is inserted at a 30- to 60-degree angle to horizontal, with the tip pointed cranioventrally, and is advanced until it contacts the floor of the vertebral canal (Figure 85-2). The depth of insertion is 3 to 6 cm, depending on the size of the horse and the angle of the needle. The needle placement can be tested by attempting to inject 2 to 3 mL of air or solution in a 3-mL syringe. Resistance to injection should be little or absent. Appropriate epidural injection of local anesthetic solution and xylazine often is confirmed when anal tone decreases and the tail relaxes, but because the drugs most commonly used for epidural analgesia of the hindlimb (morphine, detomidine) have little or no effect on motor nerves, these responses will be absent.
Epidural Catheter Placement
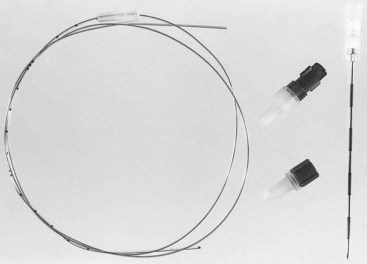
The site for insertion of an epidural catheter is the same as for a single epidural injection. Placement of the catheter requires the use of a needle with a curved point (Tuohy, Becton, Dickinson, Franklin Lakes, New Jersey, United States) that will direct the catheter cranially, along the floor of the vertebral canal (Figure 85-3). The epidural catheter is made of polyamide (nylon) or Teflon, with a closed or open end, and it can be purchased with a wire stylet if desired. I use an 18-gauge, 8.89-cm Tuohy needle and a 20-gauge, 100-cm radiodense, polyamide catheter with a closed tip (bullet tip) without a stylet (Figure 85-4). Epidural catheters have marks every centimeter and multiple marks at 10, 15, and 20 cm from the end. Before needle and catheter placement, slide the catheter inside the needle and note the distance from the tip of the needle to the hub on the catheter. The clinician then should determine which mark on the catheter will be at the hub of the needle once the catheter has been advanced to the desired position.
As with the single epidural injections, strict attention should be paid to aseptic technique, and sterile gloves must be worn. Lidocaine is injected into the subcutaneous tissues at the desired site. A small incision is made through the skin with a No. 11 scalpel, because the Tuohy needle has a blunt tip. Once the needle has been positioned, the bevel should be directed cranially (the notch on the hub of the needle should face cranially). The catheter is threaded through the needle and along the floor of the vertebral canal (Figure 85-5). Provided the needle is positioned in the epidural space, the advancing catheter receives little resistance. If the tip of the needle is angled incorrectly, the catheter tends to bump up against the vertebrae and will not advance. If this occurs, the needle is withdrawn 1 to 2 mm and the catheter is rotated slightly as it is advanced. It is critical that once the catheter has advanced any distance outside of the needle, it never be withdrawn back into the needle. This may result in cutting or shearing off of the catheter. The catheter is advanced 5 to 10 cm past the tip of the needle, and the tip is positioned in the midsacral region. Once the catheter has been positioned, the needle is carefully withdrawn over the catheter and removed (Figure 85-6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree