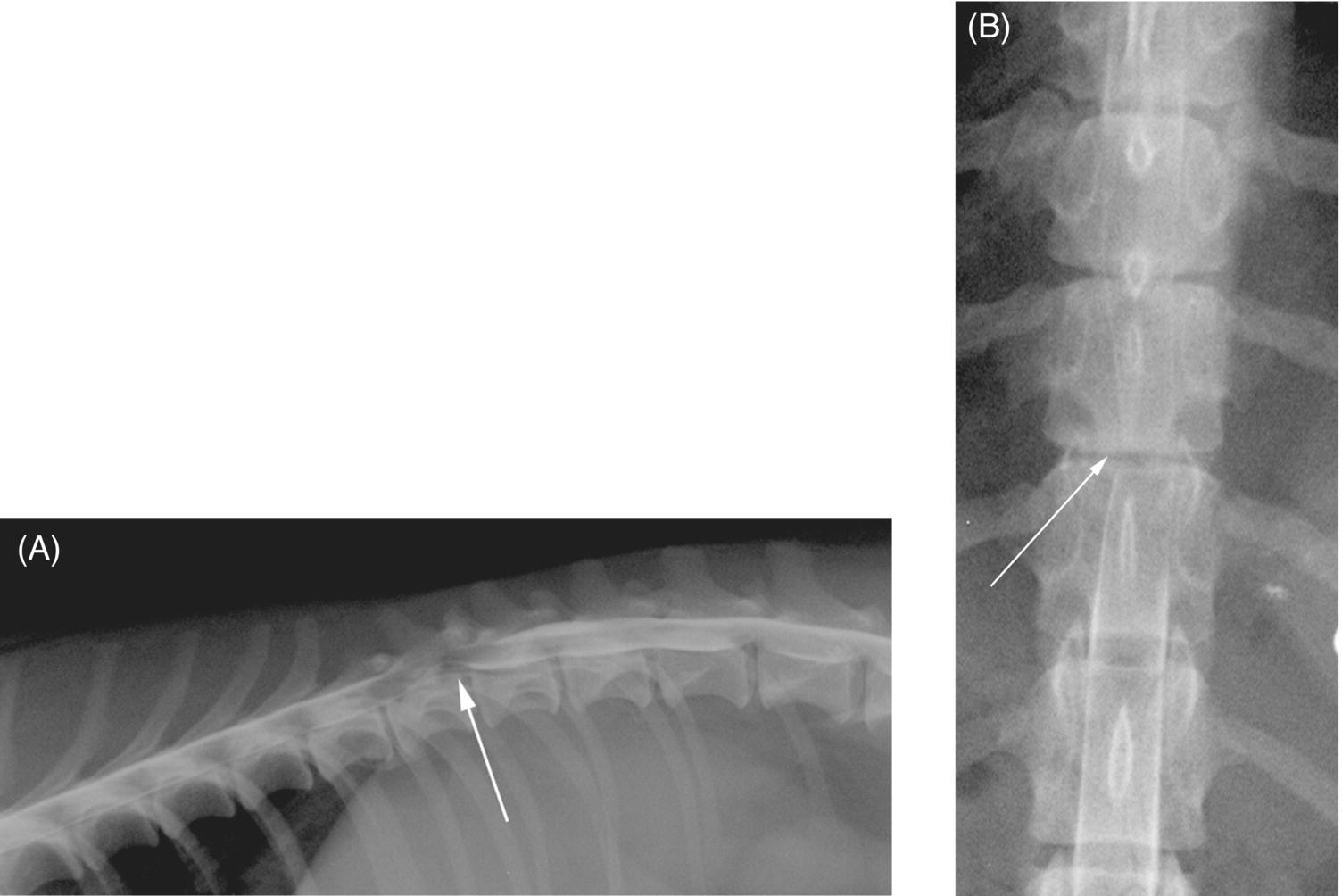
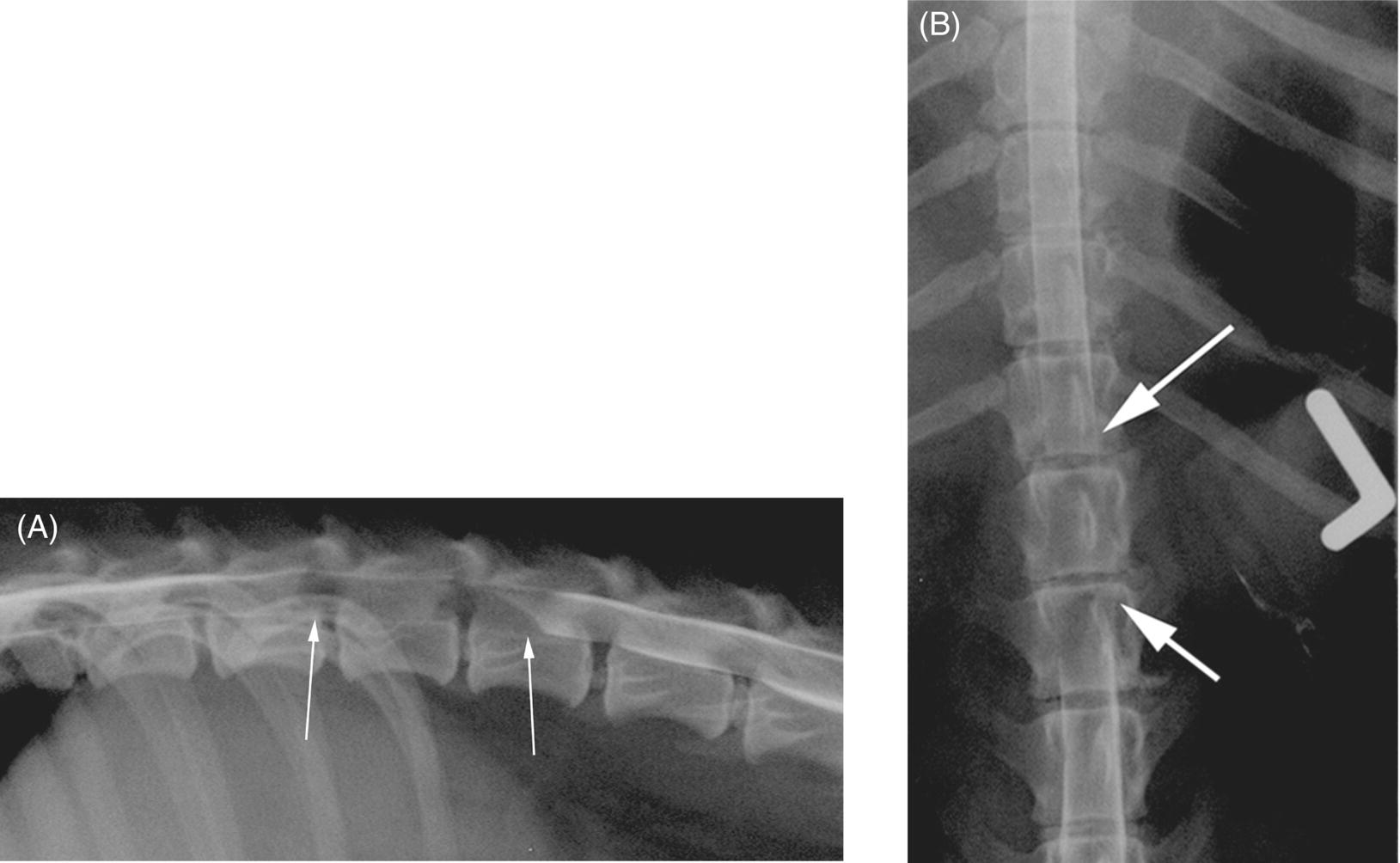
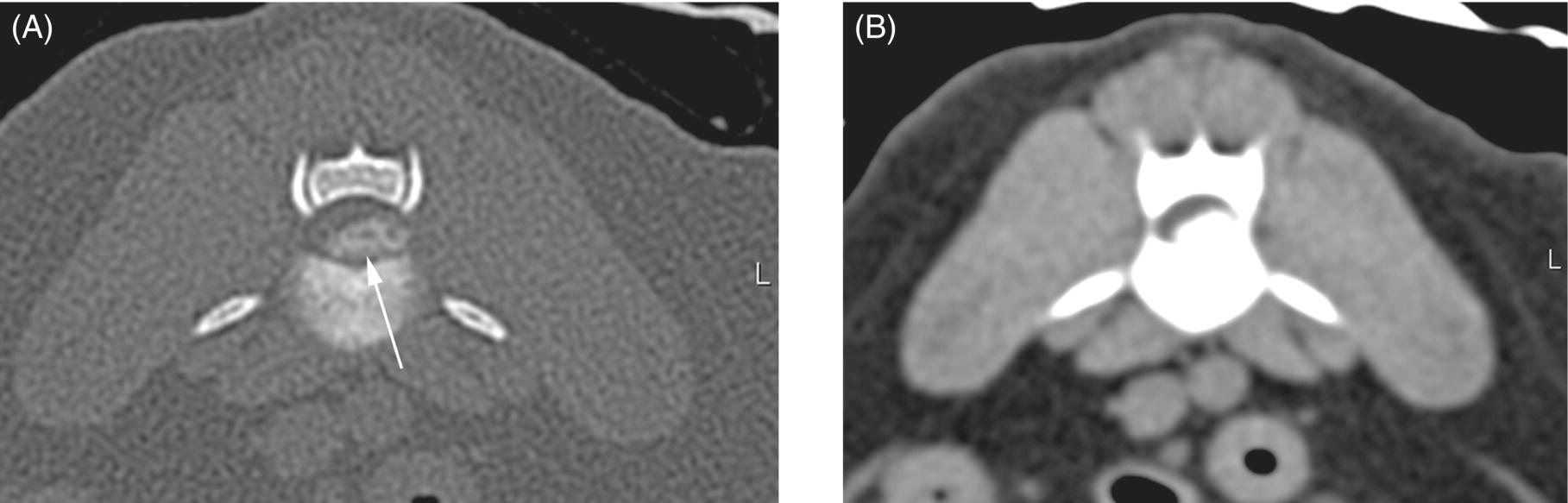
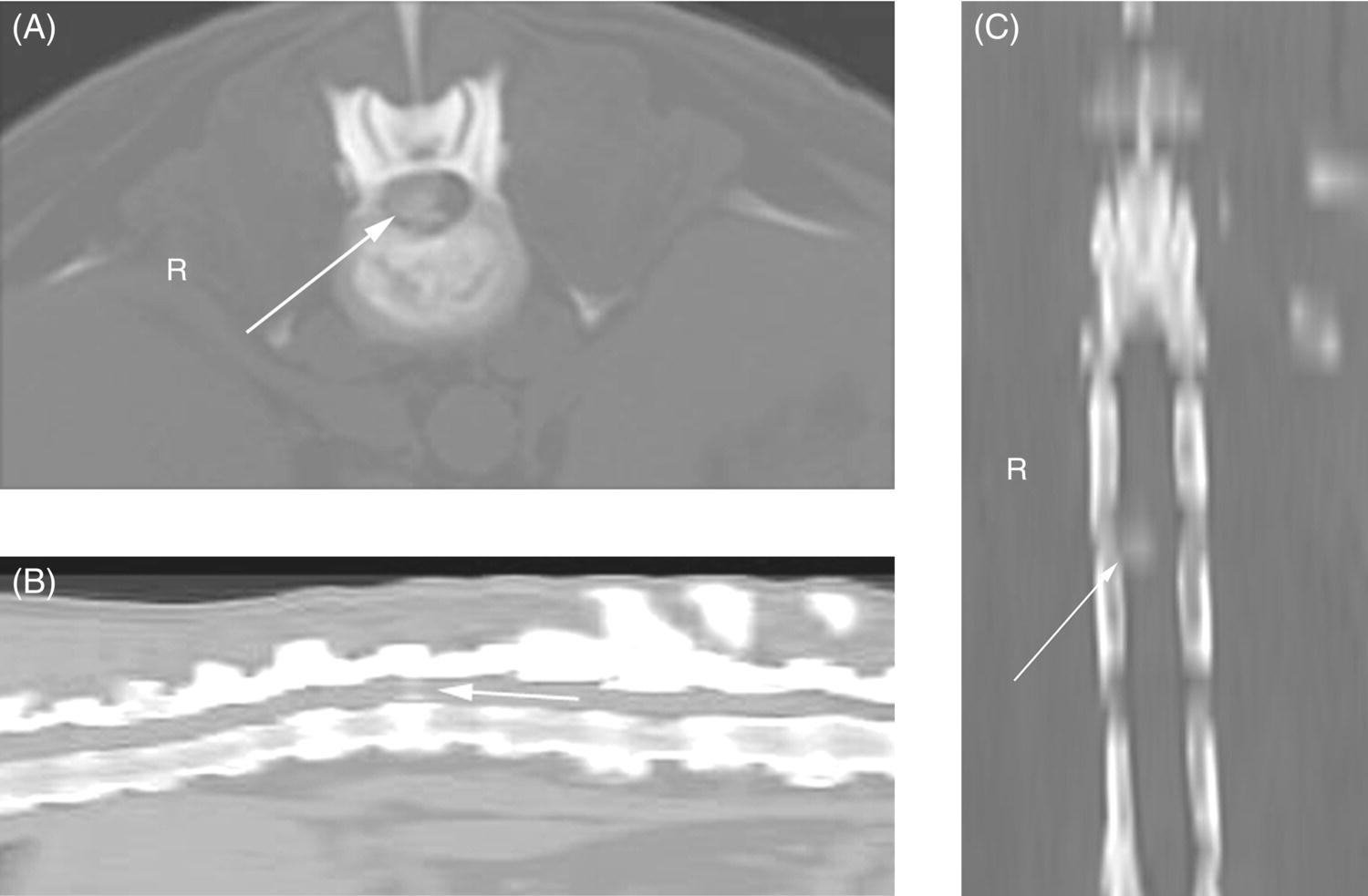
16 Patrick R. Gavin and Jonathan M. Levine As pointed out elsewhere in this text, diagnostic imaging is a necessary step for establishing the cause and options for treatment in all animals with clinical signs consistent with vertebral column pathology. In regard to imaging for suspected intervertebral disc herniation (IVDH), approaches vary depending on whether medical or surgical therapy is deemed most likely. It is critical for clinicians making imaging decisions to understand the limitations of various modalities. For example, radiography is a good, cost-effective screening tool. However, it is not adequate to diagnose IVDH definitively, does not provide sufficient information for planning decompressive surgery, and does not permit imaging of the actual spinal cord. There are various imaging modalities employed for dogs and cats with suspected IVDH. These are reviewed in the following in their order of historical appearance and ascending order of preference. Reviewed elsewhere in this text is the subject of discography for direct imaging of the intervertebral discs (see Chapter 26). Conventional radiography became widely available in the 1950s and 1960s in the veterinary profession. During this time period, radiography was commonly used to definitively diagnose IVDH [1–3]. Currently, many clinicians use vertebral radiography as a means to help exclude diseases such as overt osseous neoplasia, vertebral fracture/luxation, and discospondylitis [4]. The sensitivity of radiographs for detecting vertebral fracture/luxation and discospondylitis approximates 75 and 80%, respectively [5, 6]. Vertebral radiography has relatively poor accuracy for identifying sites of surgical IVDH in the thoracic and even less so in the cervical vertebral column [7, 8]. Additionally, it does not permit the reliable differentiation of multisite IVDH from single-site lesions [9]. Careful attention to positioning and coned-down views to reduce parallax of the image in orthogonal projections facilitate the diagnosis of vertebral column diseases. Accurate positioning requires heavy sedation or general anesthesia. Even with this effort, plain film radiography has been shown to be inaccurate and subject to marked interobserver variation. Radiography can demonstrate increased opacification of discs and in some cases can demonstrate opacified disc material superimposed within the vertebral canal (Figure 16.1). However, the spinal cord and spinal nerves cannot be visualized, thus making it impossible to conclude if there is actual disc herniation resulting in neural compression. While disc space narrowing and collapse of the diarthrodial joints can be identified in some instances, and might possibly be related to underlying IVDD at that level, this radiographic change can be spurious or misleading. Improper positioning can lead to artifactual “narrowing” of disc spaces, and there can be no certainty that any such lesion, even if real (i.e., correlated with disc degeneration at that level), corresponds to the lesion that is responsible for the current clinical signs in the patient that has prompted the imaging investigation in the first place. Hence, plain radiography is neither particularly sensitive nor specific when trying to confirm a diagnosis of disc disease or herniation, and generally cannot be relied on for surgical planning. Figure 16.1 Lateral radiograph. Intervertebral disc narrowing at T12–T13. Arrow indicates the narrowed space. Any opacification of the intervertebral foramina is difficult to judge due to superimposition of the rib. It must be remembered that discs can herniate laterally and ventrally as well as dorsally and narrowed disc spaces cannot be used alone as a determinant of the cause for the animal’s clinical signs. In the 1970s, nonionic iodinated contrast agents were developed. These contrast agents facilitated the use of myelography in the dog. Prior to the nonionic contrast agents, iodinated lipid agents were used in human patients. Due to the small subarachnoid space in dogs and cats, these contrast agents were not useful in veterinary patients. However, the water-soluble nonionic contrast agents were an improvement over plain film radiography [10]. Myelography requires general anesthesia and a degree of skill in the placement of the material within the subarachnoid space. While the atlanto-occipital region (cisterna magna or cerebellomedullary junction) is the easiest place to access the subarachnoid space, most radiologists favor the use of a low lumbar puncture at L5–L6. Cervical puncture requires gravity to distribute the contrast agent along the vertebral column, and swelling of the spinal cord can stop the advancement of the contrast agent before it can demonstrate the level of the actual lesion. A caudal lumbar injection allows pressure to be used to enhance the flow of the material cranially, although this can still be stymied by the presence of severe spinal cord swelling and/or extradural compression. In some instances where flow is blocked subarachnoid injections of contrast can be made both from the cervical end and lumbar end. However, when there is substantial spinal cord swelling, this may still fail to demonstrate the specific site of the lesion, and might only reveal a zone of several segments where contrast cannot be seen. Injection from both ends also increases the total dose of contrast, which could result in higher complication rates (such as seizures). In such instances, the radiologist and surgeon usually interpolate the approximate center of this zone and hypothesize that this is the likely level of disc herniation. Alternatively, discography could be used to try and determine the precise level of the herniation lesion (see Chapter 26) [11]. Another limitation with myelography, especially in those cases where the contrast does not opacify the subarachnoid space at the level of the lesion, is that it may not be possible to determine which side of the vertebral canal the disc material is predominantly lying on [12–14]. This hampers the surgeon from knowing with assurance which side to approach for hemilaminectomy (see Chapter 31). When there is such a multisegmental zone of absent contrast, it is also important to observe whether there is any evidence of contrast centrally, within the area where the spinal cord itself should be lying, and interpret the myelogram in light of clinical deficits, since some of these cases could represent a dog with widespread myelomalacia (see Chapter 12). Another drawback to myelography occurs when the imager is having difficulty accessing the L5–L6 subarachnoid space, either being unable to inject it at all or having only a portion of the contrast actually produce a myelogram, while the balance produces a nonuseful and confounding epidurogram. This sometimes prompts the imager to attempt lumbar puncture at a higher level (e.g., L4–L5 or even L3–L4), and this can result in significant spinal cord trauma and worsened neurologic deficits. While the newer contrast agents offered a large improvement in safety and reduced toxicity, problems still exist with myelography, where the invasive nature of the procedure could result in spinal cord damage. Myelography is limited to the same orthogonal projections as radiographs (with some oblique views being helpful) [15], and myelography only demonstrates the subarachnoid space and not the spinal cord tissues themselves (Figures 16.2 and 16.3). Complications include seizures (especially with cervical injections) and poor studies due to epidural contamination with the contrast agent, failure to access the subarachnoid space, and the aforementioned problems associated with spinal cord swelling and failure of contrast to fill the area of the spinal cord lesion [16]. Figure 16.2 (A) Contrast myelogram. An extradural lesion is seen in the ventral vertebral canal displacing the ventral subarachnoid column and thinning the dorsal subarachnoid column. The arrow indicates the site at T11–T12. (B) Ventrodorsal view of the myelogram of the same patient. The narrowness of the intervertebral disc space on this ventrodorsal film can be seen to be more right sided. Figure 16.3 (A) Sagittal myelogram. (B) Ventrodorsal myelogram. Area of subarachnoid space that is thinned but no definitive extradural compression can be seen (between the white arrows). Thin columns go from caudal T13 to cranial L2 (arrows). Extradural compressions cannot be seen. The spinal cord is obviously not visible. Cause of the thin columns cannot be ascertained. Computed tomography (CT) started to become available to the veterinary profession in the 1980s and currently has widespread acceptance. CT offered improved visualization of tissues due to the ability to manipulate the contrast windows and levels. In chondrodystrophoid dogs, disc extrusions are often mineralized. Plain CT can detect this mineralized disc material as well as hemorrhage in the vertebral canal (Figures 16.4 and 16.5) [17]. It is common practice in some hospitals to perform CT on chondrodystrophoid dogs suspected of having an intervertebral disc extrusion [18]. In many cases, disc-associated spinal cord compressive lesions are readily identified. With the advent of helical scanning, the procedure can be extremely rapid. The study can be reconstructed in multiple planes, improving conspicuity [19]. However, nonmineralized disc extrusions may not be identified. The reported accuracy of noncontrast CT for identifying IVDH in the thoracolumbar vertebral column is roughly equivalent to myelography across several recent studies [18, 20, 21]. CT does appear to more accurately determine the side of disc-associated compression compared to myelography. Figure 16.4 Transverse CT. (A) Bone window. (B) Soft tissue window. High-opacity material (arrow) can be seen in the ventral left vertebral canal (arrow) and compressing the spinal cord. Measuring the density of the material may help indicate the presence of mineralized material versus hemorrhage, but at times, there is overlap between the two tissue densities depending on the degree of mineralization. Figure 16.5 (A) CT showing opaque material in the right parasagittal vertebral canal causing spinal cord compression. Arrow points to the opaque material. (B) Sagittal reconstruction of CT in (A). Again, the arrow points to the compressive material. (C) Dorsal reconstruction showing the compressive material in the right vertebral canal (arrow). By using various images of this reconstruction, the location, in comparison to the last pair of ribs, is easily ascertained. The combination of myelography and CT yields an improved diagnostic capability [22–25]. Change in the subarachnoid space can be seen in the absence of mineralized or hemorrhagic material within the vertebral canal. Nonopaque changes to the epidural, dural, or intramedullary regions may be detected via myelography. It is common practice in many institutions that if the plain CT is nondiagnostic, then it will be followed by a CT myelogram. While there is improved conspicuity, the same toxic problems and other complications associated with myelography exist with CT myelography (Figure 16.6).
Advances in Imaging for Intervertebral Disc Disease
Introduction
Radiography

Myelography
Computed tomography
CT myelography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


