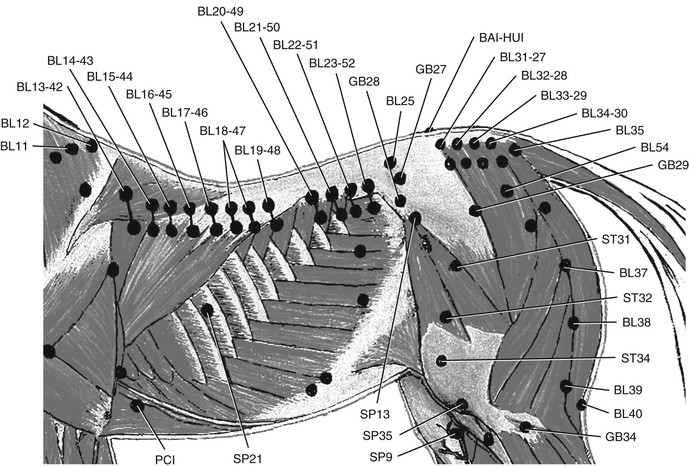
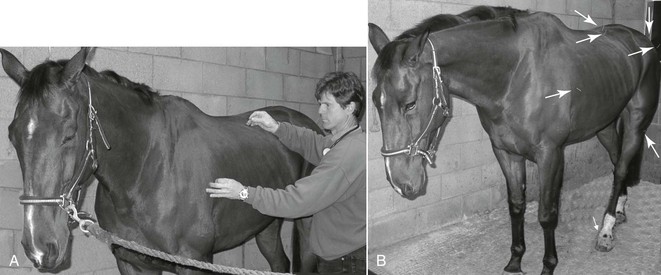
Dietrich Graf Von Schweinitz Historically, Chinese veterinary acupuncture practice differed from human acupuncture practice in the use of different acupoint (acupuncture point) locations and because of the different indications for each animal species treated. In addition, traditional animal acupuncture charts did not associate acupoints with any of the human channels (or meridians). The reasons are not entirely clear, but human patients occasionally report propagated sensation along paths or “channels” during acupuncture, and clearly these could not be recorded in animals. The closest similar phenomenon is the occasional pilomotor response seen in horses during stimulation (Figure 17-1) of acupoints along the Bladder channel (Figure 17-2), which runs along the borders of the iliocostalis and longissimus dorsi muscles in the thoracic to sacral spinal segments. These sites correlate with the neurovascular bundle of each spinal nerve that supplies the superficial tissues. The pilomotor response is one example of a somatovisceral reflex (a sympathetic nerve response) resulting from acupuncture and affecting most of the thoracic, lumbar, and sacral segments even when only a few segments have been stimulated. This response occurs mainly in horses with signs of diffuse myofascial pain of the paraspinal muscles. During the 1970s, many Western veterinarians found the Traditional Chinese Veterinary Medicine (TCVM) acupoints difficult to learn. Because there were established human acupuncture schools in the West, these early veterinary enthusiasts learned the Traditional Chinese Medicine (TCM) human acupuncture system and transposed it onto animals. Problems with this transposition arise because of the anatomic and physiologic differences among the different species (e.g., 18 thoracic vertebrae in horses vs. 12 in humans) and marked differences in limb anatomy, upon which great significance is placed in the human acupoints. The Chinese continue to follow the tradition in equine acupuncture and use charts with approximately 176 points without any channel associations: classical human channel-based acupoints number 360. Learning human point locations and nomenclature is easier because each point is assigned either to one of the 12 paired channels (named after an organ) or to the extra dorsal and ventral midline channels (named as vessels). Each channel is noted by a two-letter code (LU, LI, ST, SP, HT, SI, BL, KI, PC, TH, GB, LR, GV, and CV), and each point is numbered from the first to last along the particular channel (e.g., BL 1 to BL 67). This system offers Western veterinarians an escape from the memorization of Chinese pin yin names of the traditional animal points, but it ignores the historical application of equine acupuncture and has some significant discrepancies, including assigning different spinal segments to a particular internal organ. From a practical viewpoint, it matters little because each organ has four to six overlapping spinal segments and no single spinal nerve supply. Where it matters more is in the application of meridian-based treatment strategies that employ various “command, connecting, alarm, master, influential, generating, controlling, and other special action points,” as described in humans but without historical context for use in animals. For these reasons, the Western style of veterinary acupuncture practice is relatively recent despite claims that TCM or TCVM is being practiced. The dominant Western translations of TCM theories are based on a metaphysical concept of energy or life force circulation in meridians, developed by Soulié de Morant in the early 1900s. According to several eminent sinologists, this model is founded on inaccurate translations of the ancient Chinese medical texts (notably the Huang Di Neijing), and the original theories appear more grounded in anatomically and physiologically recognizable phenomena. A more recent view of acupuncture is that it is a physiology-based type of medicine progressively made more understandable through the emerging neurohumoral sciences. This is often referred to as Western medical acupuncture (WMA), which has been defined as an adaptation of Chinese acupuncture with current knowledge and principles of evidence-based medicine. The conflicting philosophies and practices of WMA and TCM/TCVM should be considered when a veterinarian is selecting course providers. In some countries, this process is further complicated by acupuncture practice being legally permitted by lay practitioners (as occurs in human practice). To appreciate the research advances in acupuncture physiology, one must have a reasonably current understanding of pain physiology, which has been largely ignored in equine medicine for the past 25 to 30 years. The traditional model of inflammation-based pain arising from demonstrable tissue damage is grossly inadequate. To appreciate acupuncture’s role in pain relief, the reader should study a recent review of current pain physiology centered on the equine species. Among the ancient Chinese physicians’ most astonishing discoveries are the viscerosomatic and somatovisceral reflexes, and their recognition of the interrelationships of yin and yang, which in the medical context correlate in part with the parasympathetic and sympathetic nervous systems, respectively. These reflexes are not fully understood but are believed to result from the convergence of somatic afferent and visceral-autonomic nerves in the spinal cord and brainstem. Approximately 2000 years ago, Chinese physicians described certain tender locations on the body related to diseases of particular organs (referred to as Shu and Mu points). These points are very closely correlated with the independent palpation findings of Sir Henry Head, published in the 1890s, which became known as Head zones. The tender points, which act as diagnostic aids and are a treatment source, form the basis for the acupuncture point charts. Stress activates the sympathetic nervous system, increases pain sensitivity, and suppresses parasympathetic functions. Acupuncture modulates and normalizes autonomic functions. Many studies have demonstrated acupuncture-associated inhibition of the sympathetic system in observations of skin warming and its correlation with reduced pain. Thermography of horses with regional allodynia (pain in response to a nonnociceptive stimulus) or hyperalgesia (increased pain sensitivity) and poor performance performed before and after acupuncture can result in significant sustained warming of regions that were previously abnormally cool (see Color Plate 17-1). This warming indicates relief of the excessive sympathetically mediated vasomotor tone in the affected dermatomes. The horses with normalized vasomotor control also demonstrate relief of pain signs. Acupuncture-induced parasympathetic stimulation has also been documented. Aside from its importance in the control of visceral functions, a cholinergic antiinflammatory pathway has been discovered wherein vagal stimulation activates the reticuloendothelial system and inhibits the release of tumor necrosis factor and other proinflammatory cytokines. Other important aspects of acupuncture analgesia were recently reviewed (Han, 2011), and some key points are summarized below. Local effects are mediated by needle trauma–induced release of adenosine, which inhibits nearby nociceptive afferent nerve endings. Needle stimulation inhibits nociception traffic to the brain through gate control, which is mediated through activation of serotonergic descending inhibitory pathways. Most acupuncture studies and reviews are flawed because of false assumptions regarding the sham and placebo controls. Sham points needled are often within a centimeter of the “true” points, and therefore one should expect that, where there are Aδ and Aβ nerve fibers in the appropriate spinal segments, an acupuncture effect will be seen, with only slight differences in sensitivity as a consequence of differing nerve-ending densities. Manual needle manipulation (e.g., rotation, lifting, thrusting, depth, and eliciting “de qi”) is a key aspect of treatment and is part of the art of practice, but is difficult to quantify and control from a scientific perspective, including in the design of suitable sham procedures. Aδ and Aβ nerve fibers are stimulated in most manual acupuncture approaches, but C fibers are also stimulated in more aggressive needle manipulation. Electroacupuncture has a similar range of nerve fiber stimulation, depending on intensity, and because electroacupuncture stimulation can be quantified, it has become a favored method for use in scientific studies. Involvement of endogenous opioids in the acupuncture response has long been established, and electroacupuncture studies have found that low-frequency stimulation (1 to 4 Hz) preferentially increases enkephalins and endorphins, whereas high-frequency electroacupuncture (80 to 100 Hz) increases dynorphin release. Most therapeutic electroacupuncture now incorporates alternating low- and high-frequency stimulation (often called dense disperse electroacupuncture) for 10 to 30 minutes, which induces synergistic effects and improves analgesia. Different mechanisms allow for both local and distant analgesia. Prolonged stimulation, however, can cause tolerance, which diminishes the analgesic effects. Intensity of stimulation necessary to relieve pain seems to vary with the physiologic status of the patient (recognition of which is another factor in the art of practice). Generally, the greater the inflammation or pain score, the lesser the intensity needed to induce the optimal level of analgesia. Intensity is normally selected to be between sensation and pain thresholds, and excessive painful stimulation may also cause acupuncture tolerance. Experimental studies indicate that approximately 30 minutes of stimulation is needed to achieve maximal analgesia, and 1 to 2 hours of stimulation tends to elicit a loss of analgesic effects. This tolerance is related to the release of central cholecystokinin (CCK), an opioid antagonist. High CCK release largely accounts for nonresponders to acupuncture. Hereditary factors partially control the potential for upregulation of CCK release and endogenous opioids. In humans, perioperative acupuncture decreases postoperative pain, nausea, and vomiting and decreases analgesic demand and, consequently, drug toxicosis. For treatment of some types of experimental pain in rats, acupuncture once per week is more effective than twice-weekly acupuncture, and five-times-weekly acupuncture has no therapeutic effect. One session weekly for 3 to 5 weeks is normally required for long-lasting effects in chronic pain. This is another variable involving individual differences in susceptibility with regard to pain thresholds, intensity of pain, and levels of anxiety. Functional magnetic resonance imaging studies of humans performed during acupuncture have provided evidence of responses in specific brain areas. Acupuncture often causes deactivation of the limbic system (emotional center) and accounts for the sedative effect often seen. In horses and most other species, this effect is obvious (Figure 17-3). Research indicates that this limbic deactivation effect mediates other effects, including analgesia, relief of anxiety, and integration among the autonomic, endocrine, immunologic, and sensorimotor functions.
Acupuncture for Pain Control
Theoretical Basis of Equine Acupuncture
Acupuncture Charts
TCM, TCVM, and Western Medical Acupuncture
Current Research in Acupuncture Analgesic Mechanisms
Viscerosomatic and Somatovisceral Reflexes
Autonomic Effects
Descending Inhibition and Endogenous Opioids
The Limbic System
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Acupuncture for Pain Control
Chapter 17
Only gold members can continue reading. Log In or Register to continue