CHAPTER 5. Transrectal Ultrasonography in Broodmare Practice
OBJECTIVES
While studying the information covered in this chapter, the reader should attempt to:
■ Acquire a working understanding of the principles and equipment used for performing ultrasonographic examination on the mare reproductive tract.
■ Acquire a working knowledge of the ultrasonographic appearance of the reproductive organs of the mare.
■ Acquire a working understanding of the ultrasonographic appearance of the mare reproductive tract and conceptus during the estrous cycle and early pregnancy.
■ Acquire a working understanding of the ultrasonographic appearance of ovarian and uterine abnormalities of the mare reproductive tract.
STUDY QUESTIONS
1. List the components and characteristics of an ultrasound machine suitable for use in examination of the mare reproductive tract.
2. Describe the technique for safely performing a transrectal ultrasonographic examination of the mare reproductive tract. Emphasize the importance of a systematic approach to ensure thorough scanning of the uterus of a mare for early pregnancy diagnosis.
3. Describe the ultrasonographic appearance of:
a. The anestrous ovaries
b. A preovulatory follicle
c. An ovulatory follicle (within 24 hours after ovulation)
d. The developing corpus luteum
e. The mature corpus luteum
f. The estrous uterus
g. The diestrous uterus
h. An anovulatory follicle
i. An ovarian hematoma
j. A granulosa cell tumor
k. Uterine lymphatic cysts
l. Intrauterine fluid accumulation associated with endometritis
In 1980, real-time ultrasonography was first reported as a potentially valuable diagnostic modality in the discipline of equine reproduction. Since this original report, applications of diagnostic ultrasonography in equine reproduction have expanded to the point that ultrasound has become a fundamental, indispensable tool for both veterinary clinicians and research scientists.
The two-dimensional grayscale image produced with B-mode (brightness-modality) real-time ultrasonography provides a detailed cinematographic view of the structure being studied. With this modality, the observer can actually visualize “hidden” reproductive organs and follow various reproductive events in a noninvasive manner, with no apparent adverse biologic effects incurred by the patient. More recently, color Doppler ultrasound has been used to assess blood flow in the uterus, ovary, and uterus of the mare. Transvaginal ultrasound has also been used for aspiration of oocytes from ovarian follicles, twin reduction, and deposition of embryos into the uterus. Although the technology behind real-time ultrasonography is quite complex, operation of the unit is relatively simple for the trained theriogenologist, requiring only a basic knowledge of ultrasound principles and ultrasonic anatomy of the reproductive tract.
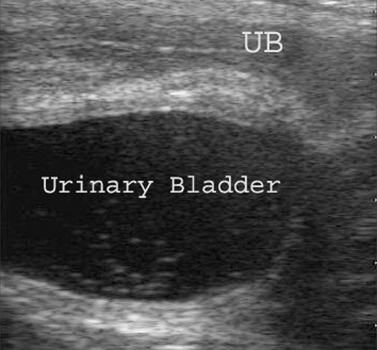
INSTRUMENTATION
A B-mode real-time ultrasound system consists of a transducer that is connected by a long cord to a base unit containing a display monitor and control panel (Figure 5-1). The transducer transmits and receives high-frequency sound waves to produce images of soft tissues and organs on the display monitor. Tissues vary in echogenicity (i.e., the ability to propagate or reflect sound waves); therefore, the proportion of reflected sound waves is dependent on the innate characteristics of the tissues or fluids being examined. For instance, fluids readily propagate sound waves, whereas air and dense tissues reflect most or all sound waves. Reflected sound waves that are received by the transducer are then converted to electronic impulses and subsequently displayed on the monitor. The monitor consists of a two-dimensional array of closely aligned dots. The brightness of the dots is directly proportional to the amplitude of the echoes (or reflected sound waves). Hence, highly echogenic tissues (e.g., bone or connective tissue) appear white on the ultrasound monitor whereas nonechogenic (anechoic) fluids are black. A continuum of gray shades between white and black allows one to distinguish tissues of intermediate echogenicity. The control panel of the ultrasound unit allows the operator to adjust the quality of the image and label or measure structures of interest. Because air interrupts the transmission of ultrasound waves, when air is present within a viscus, bright echogenic lines or spots are seen on the monitor. When sufficient blockage of ultrasound waves occurs, artifactual shadows or reverberations may be produced below the initially sound-impacted echogenic structure or tissue on the monitor. For example, dark shadows are visible on the monitor below sound-impacted bone, such as fetal ribs. Reverberation echoes are bright artifacts repeated at even intervals, but with lesser reverberation, because blocked sound waves are bounced back and forth between the probe and a gas-filled viscus. Artifacts not only interfere with the ability of the examiner to visualize surrounding tissue but may be falsely interpreted to be pathologic structures.
Linear-array 5-MHz transducers are amenable to most needs encountered in equine reproduction. The higher resolving power of 7.5-MHz transducers allows a more detailed study of structures, but the tissue-penetrating capacity of these transducers is more limited. Transducers with lower sound wave frequencies (e.g., 2.5 to 3.5 MHz) permit greater tissue penetration, so they may be more useful for evaluation of the uterus and its contents during advanced pregnancy; however, image resolution is reduced accordingly. Curvilinear transcutaneous probes available for thoracic or abdominal imaging can be useful for monitoring fetal viability (e.g., heartbeat, fetal activity), character and amount of amniotic or allantoic fluid, uteroplacental thickness, and separation of the placenta.
Color Doppler ultrasound is becoming available in less expensive, often portable, machines. This field of study could increase diagnostic information available to the theriogenologist. The basis for the technology is in the shift in ultrasound frequency of echoes from red blood cells in motion as they move toward or away from the transducer. This allows pictorial assessment of blood flow, which can be seen on the monitor in color-flow mode. Characterizing changing blood flow (perfusion) may be an important indicator of viability of transitional follicles, corpora lutea, and pregnancy, providing information that would otherwise not be available. Many of the portable Doppler ultrasound units use linear or curvilinear probes that are easily used within the rectum or vagina.
PROCEDURAL CONSIDERATIONS
Ultrasound evaluation of the mare’s reproductive tract is generally performed with a transrectal approach. Usefulness of transcutaneous ultrasonography is limited to evaluation of the uterus and fetus during more advanced (3 to 4 months to term) pregnancy.
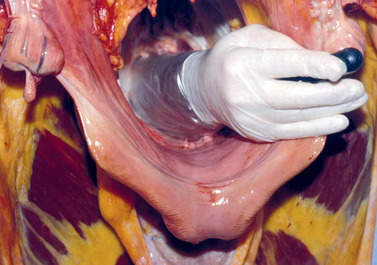
Precautions regarding mare restraint and reproductive examination per rectum are similar to those issued for palpation per rectum. Minimal but effective restraint of the mare greatly reduces the likelihood of equipment damage or injury to the mare or operator during the examination process. When examining the mare’s reproductive tract via transrectal ultrasonography, the following steps should be taken:
1. All manure is removed from the rectum with a well-lubricated arm. Care is taken to avoid entry of air into the rectum during the manure-evacuation process because air effectively prevents transmittance of ultrasound waves into surrounding structures.
2. The internal genital organs are palpated in their entirety and in a systematic manner.
3. Palpation per rectum is followed by an ultrasonographic examination, with the transducer well shielded by the examiner’s hand to avoid undue trauma to the wall of the rectum. A methodical approach should be used during the examination.
4. The transducer should be well lubricated and should have good contact with the rectal wall. Manure or air should not be interposed between the transducer and the tissue of interest.
5. If the mare resists excessively, the examination should be discontinued, or the mare should be sedated, given a tocolytic (e.g., Buscopan, Boehringer Ingelheim Pharmaceuticals, Ridgefield, Conn.), an infusion of intrarectal lidocaine, or epidural anesthetic, before continuing. If so treated, the mare’s reproductive tract should be examined as soon as deemed prudent to prevent pneumorectum from developing as anal sphincter relaxation occurs. Pneumorectum increases the risk of injury to the rectum during the examination and also interferes with transducer contact with the rectum, thereby reducing ultrasound image clarity.
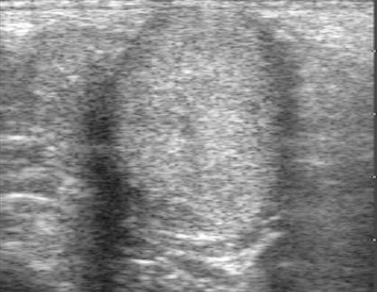
For ultrasound examination of the mare reproductive tract per rectum, we prefer to advance the transducer over the cervix and body of the uterus until the bifurcation of the uterus is visualized (Figure 5-2, Figure 5-3, Figure 5-4 and Figure 5-5). The transducer is slowly moved toward the tip of one uterine horn, with care taken to ensure the image of the uterine horn in cross section remains in the center of the monitor screen. As the transducer moves beyond the tip of the uterine horn, the ovary is scanned (Figure 5-6) in its entirety. The transducer is then moved slowly back down the uterine horn to the bifurcation, and the opposite uterine horn and ovary are scanned in a similar manner. After scanning the opposite ovary, the transducer is moved slowly back to the bifurcation and is rotated slightly in a back-and-forth motion across the uterine body and cervix as it is withdrawn from the rectum. This systematic scanning procedure ensures that the entire reproductive tract is examined twice, permitting accurate identification of the location of singleton or multiple pregnancies and uterine pathologic conditions, and provides confidence that no conceptus was overlooked during the examination process.
Transabdominal ultrasonography allows maximum visualization of the fetus and placenta, sometimes beginning as early as 60 to 80 days of gestation. Lower frequency (2.5 to 3.5 MHz) curvilinear transducers in various configurations are used for this purpose (Figure 5-7) and may allow assessment of the uterus in the inguinal area in some cases. In later gestation, maximal penetration into the ventral abdomen is necessary. Application of ultrasound gel or alcohol is helpful for improving contact between the transducer (ultrasound probe) and skin, allowing underlying structures to be more easily visualized. Because hair traps air, which interferes with sound wave propagation, it may be necessary to clip the hair closely, from the xiphoid-sternum to the udder, and on the lower flanks on either side of the midline, to improve transducer contact and thus image clarity. For advanced pregnancy, the transducer is initially placed between the sternum and the mare’s udder (Figure 5-8), followed by slow movement from side to side and cranial to caudal, until the fetus is located. Fluid within a viscus (especially the nongravid horn) is searched for to locate the uterus. Fetal structures (e.g., skull, foot, ribs) or membranes are often visualized, which aids in identification of the gravid uterus. Locating the fetal skull or thorax is helpful for orientation. Fetal heart rate, movement, amount and character of fluid (amniotic/allantoic), uteroplacental thickness, and evidence of separation between the uterus and placenta are typically evaluated by the examiner to determine normalcy (see Chapter 9). Examination for two fetuses is also possible if a question about twin status exists.
Per vagina ultrasonography has recently been used in horses for transvaginal aspiration of oocytes (follicular aspirations) and transvaginal aspiration or injection of the yolk sac or allantois of an early twin conceptus (see Figure 8-26). A common apparatus uses a stainless steel needle guide installed in an elongated plastic probe extension handle that accommodates a small curvilinear ultrasound probe in the tip (Figure 5-9). After sterilization and assembly, a 24-inch, 12- to 16-gauge, single- or double-port needle is inserted into the needle guide in the probe handle. The handle is used to insert the ultrasound probe into the cranial vagina; the operator uses the other hand in the rectum to position the structure of interest immediately next to the probe held in the vagina (Figure 5-10). Some ultrasound machines have software installed that delineates a dotted line on the ultrasound monitor and indicates where the needle will pass once inserted through the vaginal tissue. While the structure of interest (ovary with follicle, portion of uterine horn containing the twin conceptus) is held firmly against the ultrasound probe, the needle is forced through the cranial vagina, retroperitoneal fascia, and peritoneum into the structure of interest.
Diagnostic ultrasonography is used in the broodmare for (1) evaluation of ovarian activity, (2) detection and evaluation of pregnancy, and (3) diagnosis of pathologic changes in the reproductive tract. Although transrectal ultrasonography is emphasized in this chapter, transabdominal ultrasonographic images are shown in Chapter 9.
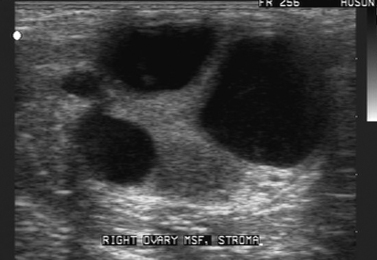
EXAMINATION OF THE OVARIES
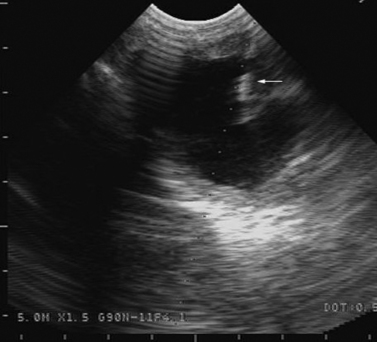
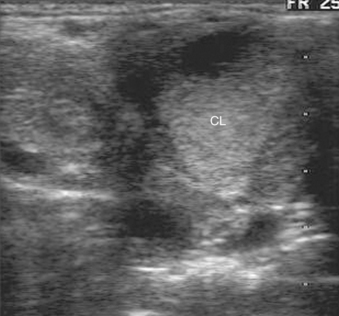
The ovaries of the mare are easily visualized with transrectal ultrasonography. The connective-tissue stroma is uniformly echogenic (white). Follicles are fluid-filled and, hence, represented as circular or irregularly shaped anechoic (black) images on the ultrasound monitor (see Figure 5-6). The ultrasonographic appearance of a corpus luteum is variable and ranges from a uniformly hyperechoic image (Figure 5-11) to a heterogeneous or mottled image, in which only a portion of the gland contains echogenic material (Figure 5-12). Because of the distinct border, many corpora lutea can be distinguished from the surrounding stroma throughout their life span.
Estimating the Stage of the Estrous Cycle by Ovarian Characteristics
Because of the ease with which follicles and corpora lutea can be detected with transrectal ultrasonography, this technique can be used to approximate the stage of the estrous cycle in mares. One can also distinguish those mares that exhibit reproductive cyclicity from those that are seasonally anestrous or are in transitional estrus.
The advent of high-quality real-time ultrasound imaging has permitted detailed study of follicular dynamics in mares throughout the estrous cycle. Mares tend to have either one or two follicular waves during the estrous cycle, with one follicular wave being the most common pattern. In either case, the ovulatory follicle becomes ultrasonically identifiable approximately 10 to 12 days before ovulation (see Chapter 2). Diestrous follicles (i.e., large follicles detected while a functional corpus luteum is present) sometimes become quite large (e.g., ≥35 mm in diameter), although the preovulatory follicle of estrus is generally the largest follicle of the estrous cycle.
Follicles destined to ovulate tend to grow rapidly (approximately 3 to 5 mm per day increase in mean diameter) beginning approximately 7 days before ovulation, with corresponding atresia of other follicles within the same follicular wave. If a 5-MHz transducer is used for the examination, corpora lutea tend to be identifiable throughout their functional life span (generally about 13 to 14 days). Occasionally, the gland remains ultrasonically visible through the following ovulation. Unless a clear border is visible around the corpus luteum, differentiation between a corpus luteum (CL) and ovarian stroma may be difficult, as both are echogenic. “Mare-side” progesterone assays can be of help in such cases. If progesterone concentration in the blood is high (>2 ng/mL), a functional CL must be present. If progesterone concentration is low, the echogenic tissue in the ovary is more likely to be stroma or a regressed CL. When all of the ultrasonographic features of the ovarian structures are used in conjunction with echotexture of the uterus and palpable characteristics of the cervix, the stage of the estrous cycle can be predicted much more accurately than with palpation per rectum alone.
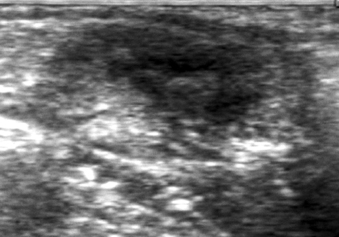
Ovarian inactivity (i.e., small ovaries with minimal or no follicular activity and no luteal structures) is typical of mares in seasonal anestrus (Figure 5-13). Transitional estrus has typically been characterized as protracted, sometimes irregular, estrous behavior with pronounced follicular activity (i.e., multiple follicles of varying size) in the absence of a detectable corpus luteum. However, English workers recently showed that as many as seven waves (average, three) of follicular growth with development of uterine edema can occur during transitional estrus before the first ovulation of the year finally occurs.
 Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|