CHAPTER 5. Diagnostic Imaging
Laura Jean Armbrust
GENERAL PRINCIPLES OF IMAGING
I. Image formation
A. X-rays are produced by an x-ray tube and are controlled by the milliamperage (mA) and kilovoltage peak (kVp) settings
B. Differential absorption of the x-rays within the body allows for differences in opacities on the radiograph
C. Multiple forms of imaging are available
1. Conventional film-screen radiography
2. Digital radiography: Computed radiography (CR) and direct digital radiography (DDR)
II. Image interpretation
A. Check for correct patient labeling, positioning, and inclusion of the entire area of interest
B. At least two (orthogonal, at right angles) or more images should be made to correlate a two-dimensional (2-D) radiograph with a three-dimensional (3-D) patient
C. There are five basic radiographic opacities. From least to most opaque these include air, fat, water or soft tissue, bone, and metal or contrast material
D. Describe abnormalities in terms of the following: size, number, opacity, contour or shape, and location
SMALL ANIMAL ORTHOPEDICS
I. Normal. There is variation in the physeal closure time among animals. Radiograph the opposite limb when there is a question
II. Appendicular skeleton
A. Traumatic disease
1. Fracture detection and description
a. Fractures are defined by the following:
(1) Limb and bone involved
(2) Fracture type
(3) Direction of displacement
(4) Articular involvement
(5) Soft tissue changes
b. Special classifications in animals with open physis: Salter-Harris classification
2. Fracture healing
a. Evaluate initial postoperative radiographs using the 4 A’s:
(1) Apposition
(2) Alignment
(3) Appliance
(4) Articular surface
b. Healing is usually through secondary bone healing that is seen on radiographs as the following:
(1) First week: Increase in the width of the fracture gap
(2) At 10 to 14 days, variable amount of callus begin to appear
(3) At 4 to 8 weeks, fracture is less distinct with larger amounts of relatively smooth callus
3. Fracture complications
a. Nonunion: Lack of progression of healing after 16 weeks
b. Malunion: Fracture healed in abnormal alignment
c. Osteomyelitis: Variable osteoproductive and lytic
d. Implant failure: Broken or migration of implants
e. Angular limb deformity: Common in premature closure of the distal ulnar physis
f. Sequestrum formation: Portion of bone lacking vascular supply is not incorporated in healing process
g. Fracture associated sarcomas: Rare, approximately 5 years after fracture
B. Aggressive bone disease
1. Define by type of periosteal reaction, type of bone lysis, and zone of transition between normal and abnormal bone
2. Types of periosteal reaction from least to most aggressive: Smooth, lamellar, irregular, sunburst, amorphous
3. Types of bone lysis from least to most aggressive: Geographic, moth eaten, permeative
4. The longer the zone of transition, the more aggressive the disease
5. Neoplasia
a. Variable degree of osteolysis and production
b. Primary bone: Osteosarcoma most common (away from the elbow and toward the knee plus distal tibia). Usually does not cross joints
c. Metastatic neoplasia to bone
6. Infectious disease will have a variable degree of osteolysis and osteoproduction
a. Granulomatous or fungal disease
b. Osteomyelitis
7. A bone biopsy is often required to get a definitive diagnosis
C. Congenital
1. Polydactyly: One or more extra digits
2. Syndactyly: Bony fusion of one or more digits
3. Many types of dwarfisms and skeletal dysplasia occur but are uncommon. These usually result in abnormal ossification and shape/length of the skeleton
D. Developmental
1. Panosteitis: Disease of young, large to giant breed dogs (Figure 5-1)
 |
| Figure 5-1 Stages of panosteitis. A, Early stage in a femur. Circumscribed increased opacity is visible in the mid-diaphysis and the proximal diaphysis. B, Middle stage in a humerus. Diffuse increased opacity of the entire diaphysis and a continuous periosteal new bone formation on the diaphysis are present. C, Later stage in radius and ulna. Less intense but still apparent increased opacity is visible, primarily in the proximal radius and ulna. Mild periosteal new bone formation is present on the cranial radius ( arrow). (From Thrall DE. Textbook of Veterinary Diagnostic Radiology, 5th ed. St Louis, 2007, Saunders.) |
a. Radiographs: Increased intramedullary opacity of long bones
b. Most common in the German shepherd (can be seen in older shepherds) and basset hound
2. Hypertrophic osteodystrophy (HOD): Disease of young large to giant breed dogs. Radiographs – abnormal lucent lines (double physeal line) in the metaphysis (most commonly the distal antebrachium) (Figure 5-2)
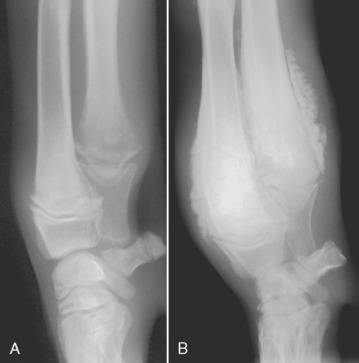 |
| Figure 5-2 Hypertrophic osteodystrophy. A, Acute phase. Irregular radiolucent regions are evident in the distal radial and ulnar metaphyses, proximal to the physis. B, Chronic phase. An irregular, pallisading periosteal productive response surrounds the radial and ulnar metaphyses. The physes are relatively unaffected. (From Thrall DE. Textbook of Veterinary Diagnostic Radiology, 5th ed. St Louis, 2007, Saunders.) |
E. Hypertrophic osteopathy (HO) generally affects older dogs secondary to a thoracic (and less commonly abdominal) mass
1. Radiographs: Palisading periosteal reaction and soft tissue swelling of multiple long bones; bilaterally symmetrical
2. The periosteal reaction starts distally and eventually progresses up the limb
3. Always take thoracic radiographs to check for a mass
III. Axial skeleton: Spine
A. Atlantoaxial subluxation
1. Congenital malformation or hypoplasia of the dens
2. Young small and toy breeds
3. Be careful to avoid excessive flexion of the neck in these patients during radiography
4. Radiographic findings
a. Widening of the space between the atlas and spinous process of the axis
b. Abnormal or absent dens
B. Cervical spondylopathy (wobbler syndrome, cervical vertebral instability)
1. Young Great Danes and older Doberman pinschers
2. Radiographic findings:
a. Malformation of the vertebral bodies (C5-C7)
b. Malalignment of the vertebral bodies
c. Intervertebral disk space narrowing
d. Spondylosis deformans
e. Sclerosis of the vertebral end plates
f. Degenerative changes of the articular facets
3. Often need myelography for a definitive diagnosis
C. Lumbosacral instability
1. Radiographic findings (note these same findings are found in dogs with degenerative disease that do not have signs of neurologic disease)
a. Narrowing of intervertebral disk space at L7-S1
b. Spondylosis deformans at L7-S1
c. Sclerosis of the end plates at L7-S1
d. Malalignment of the sacrum and L7
2. Often need computed tomography (CT) or magnetic resonance imaging (MRI) to confirm
1. Most common in chondrodystrophic breeds (dachshund)
2. Radiographic findings
a. Narrowing or wedging of the intervertebral disk space
b. Narrowing of the intervertebral foramina
c. Increased opacity in the spinal canal
d. Narrowing of the joint space at the articular facets
3. Myelography is performed to confirm a lesion prior to surgery
E. Spondylosis deformans
1. Degenerative change of the spine
2. Radiographic findings. Smooth new bone formation that may be bridging at the ventral (and sometimes lateral) vertebral endplates
F. Neoplasia
1. Primary bone tumors generally affect one vertebra
2. Spinal cord tumors usually cannot be detected without myelography
3. Extension of neoplastic disease from the caudal abdomen and perineal tissues can result in osteolytic and osteoproductive changes at L5 through the sacrum and caudal vertebrae
G. Diskospondylitis
1. Infection of the intervertebral disk space and adjacent vertebral endplates
2. Radiographic findings
a. Osteolysis of the vertebral endplates
b. Multiple sites may be affected
c. Widening or collapse of the intervertebral disk space
H. Trauma
1. Compression fractures
2. Subluxation and luxation
IV. Axial skeleton-skull
A. Ear disease
1. Otitis externa: Thickening and mineralization of the external ear canals, with partial to complete occlusion of the normally air filled canals
2. Otitis media: Soft tissue or fluid opacity of the tympanic bulla with occasional changes in the bulla wall in severe cases
3. Nasopharyngeal polyps: May see increased soft tissue opacity of tympanic bulla and nasopharynx
B. Nasal disease: Usually divided into destructive or nondestructive rhinitis
1. Destructive rhinitis
a. Causes
(1) Neoplasia: Adenocarcinomas most common
(2) Fungal rhinitis
(3) Chronic foreign bodies
(4) Chronic inflammatory disease
b. Radiographic findings
(1) Increased soft tissue opacity in the nasal passages and frontal sinuses
(2) Destruction of the nasal turbinates
(3) Destruction of the bones surrounding the nasal passages, usually most severe with neoplasia
2. Nondestructive causes
a. Inflammatory disease
b. Bacterial rhinitis
c. Foreign bodies
C. Dental disease: Peridontal disease is most common. Radiographic findings include the finding:
1. Widening of the periodontal space
2. Loss of the radiopaque lamina dura
3. Root resorption
4. Tooth loss
D. Other
1. Cranial mandibular osteopathy (CMO)
a. Affects terrier breeds
b. Radiographic findings:
(1) Irregular new bone involving the mandibles and occasionally parietal, frontal, and maxillary bones
(2) Can result in temporomandibular joint (TMJ) ankylosis
2. Neoplasia: Can occur anywhere on the skull. Osteosarcoma is most common, with a variable degree of osteolysis and osteoproduction
V. Joint disease
A. Traumatic
1. Luxations and fractures
2. Stress radiographs may be helpful to demonstrate instability
B. Degenerative
1. Commonly stifle secondary to cranial cruciate rupture, coxofemoral joints secondary to hip dysplasia, and elbow and shoulder joints
2. Radiographic findings
b. Decreased joint space width
c. Periarticular osteophyte formation
d. Enthesopathy: New bone at soft tissue attachment sites
e. Subchondral bone sclerosis
f. Subchondral cystic changes in severe cases
g. Mineralization of soft tissues: Intra articular or periarticular
C. Neoplastic. Synovial cell sarcoma is most common
1. Destruction of subchondral bone
2. Soft tissue swelling
D. Inflammatory
1. Infectious
a. Hematogenous
b. Direct: Wounds, surgery, injections
c. Radiographic findings
(1) Subchondral bone lysis
(2) Intraarticular soft tissue swelling
2. Noninfectious: Immune mediated
a. Erosive
(1) Rheumatoid arthritis
(2) Greyhound polyarthritis
(3) Feline polyarthritis
(4) Radiographic findings
(a) Joint effusion
(b) Variable degree of subchondral bone lysis
(c) Decreased joint space width
(d) Variable degree of periarticular new bone
b. Nonerosive: Radiographs usually normal or show joint effusion
(1) Systemic lupus erythematosus (SLE)
(2) Idiopathic
E. Developmental
1. Osteochondrosis (OC) or osteochondritis dessicans (OCD)
a. Large and giant breed, young dogs
b. Failure of endochondral ossification
c. Common sites: Caudal humeral head, humeral condyle (medial aspect), stifle, tarsus (medial or lateral trochlear ridges)
d. OC has no flap; OCD has a mineralized flap or joint mouse
e. Radiographic findings
(1) Concave or flattened defect of the subchondral bone with adjacent bone sclerosis
(2) With or without bone flap at the site or within the joint
(3) Joint effusion
(4) Secondary degenerative joint disease
2. Hip dysplasia
a. All breeds of dogs and cats are affected, but it is most common in large- and giant-breed dogs
b. Radiographic findings:
(1) Incongruency or subluxation of the coxofemoral joints
(2) Poor coverage (less than 60%) of the femoral head by the dorsal acetabular rim
(3) Signs of degenerative joint disease (osteoarthrosis):
(a) Osteophytes at the cranial acetabulum
(b) Shallow acetabulum
(c) Remodeling of the femoral head and neck
(d) Enthesopathy at the joint capsule attachment
c. OFA (Orthopedic Foundation for Animals) and PennHIP are the two most commonly used regeristries
3. Elbow dysplasia
a. Ununited anconeal process: Anconeal process should fuse by 20 weeks (5 months)
b. Fragmented medial coronoid process: Often see the degenerative changes rather than the actual fragment
c. OC at the medial aspect of the humeral condyle
4. Avascular necrosis of the femoral head (Legg-Calves Perth disease)
a. Small and toy breed, young dogs affected
b. Radiographic findings
(1) Flattening/misshapen femoral head
(2) Increased and decreased opacity of the femoral head and neck
(3) Increased joint space width
(4) Fractures of the femoral head can occur
5. Patellar luxation
a. Most common in small and toy breeds
b. Medial luxation is more common than lateral
c. Lateral luxations usually occur in larger breeds
d. The luxation may be intermittent so may not always see on radiographs
SMALL ANIMAL THORACIC
I. General principles. Always take at least two orthogonal (i.e., lateral and dorsoventral [DV] or ventrodorsal [VD] views). When checking for pulmonary metastatic disease, both lateral views and the DV or VD should be taken. This is because the nondependent lung will be better aerated
II. Upper respiratory
A. Laryngeal
1. Laryngeal paralysis: Radiographs are usually normal
2. Laryngeal mass: Increased opacity in the laryngeal region. Can be caused by neoplasia, inflammatory disease, or foreign bodies
B. Tracheal
1. Tracheal collapse: Narrowing of portions of the trachea. Most common in toy to small breeds. Collapse of the intrathoracic trachea and mainstem bronchi is best seen on expiratory films. Fluoroscopy or endoscopy is useful for dynamic changes
2. Tracheal hypoplasia: Congenital narrowing of the entire trachea
4. Tracheitis: Usually radiographs are normal. Occasionally irregularity or thickening of the tracheal wall is present in severe cases
III. Pulmonary
A. Evaluate the overall pulmonary opacity. Increased, decreased, or normal
B. Pay close attention to distribution and location of disease: Focal, multifocal, diffuse, perihilar, cranioventral
C. Types of lung patterns (often combinations of the following patterns are present):
1. Interstitial: Can be divided into structured (nodular) or unstructured (results in diffuse increase opacity without nodular form)
2. Bronchial: Thickening of the bronchial walls and increased opacity within the lumen. Defined on radiographs as donuts in cross-section and tram lines in longitudinal section
a. Bronchiectasis: Defined as lack of normal tapering of the bronchi
b. Bronchial pattern is typically seen with inflammatory disease (either allergic or infectious). With feline lower airway disease, about 20% of patients will have collapse of the right middle lung lobe (right middle lung lobe syndrome)
3. Alveolar: More severe increase in pulmonary opacity than that seen with interstitial disease. Will cause border effacement (results in loss of visualization of the margin) of pulmonary vessels and structures adjacent to the affected lung (diaphragm, heart, etc.). Can occur with fluid or cells. Distribution and duration of disease are important as discussed with specific diseases listed below.
4. Vascular: An increase or decrease in the size of pulmonary arteries and veins. Most common abnormalities are listed below:
a. Heartworm disease: Increase in the size of the pulmonary arteries. Arteries become tortuous and blunted. Caudal lobar arteries are most commonly affected
b. Left-sided heart failure: Results in pulmonary venous distention; often concurrent pulmonary edema
c. Congenital diseases discussed below
D. Patterns typical for specific disease
1. Benign disease or artifacts
a. Pulmonary microlithiasis (pulmonary osteomata, pulmonary osseous metaplasia, dystrophic mineralization): Mineral opacities (smaller than 3 mm) throughout the lung
b. Artifacts include structures on the surface of the skin (e.g., debris, ticks), nipples, skin-fold artifact, and costochondral junctions
2. Pneumonia
a. Viral pneumonia: Normal to an unstructured interstitial pattern that is diffuse (sometimes most easily seen dorsally in the caudal lung lobes)
b. Bacterial: Typical distribution is cranioventral alveolar disease
c. Fungal: Structured interstitial pattern (miliary to nodular) that is diffuse. May see concurrent lymphadenopathy
d. Parasitic: Multifocal ill-defined nodular opacities
3. Metastatic neoplasia: Most common pattern is a nodular pattern. Occasionally can see a somewhat unstructured interstitial pattern (lymphoma and mammary carcinoma)
4. Primary neoplasia: Solitary lung lobe mass or diseased lung lobe. Caudal lung lobes most commonly affected but can occur anywhere
5. Pulmonary edema (cardiac): Left-sided heart failure results in pulmonary edema that can have an interstitial to alveolar pattern. In dogs the distribution starts perihilar and spreads as severity increases. In cats there is no typical pattern of pulmonary edema
6. Pulmonary edema (noncardiac). There are numerous causes, such as neurogenic (post-seizure), electric cord shock, chocolate toxicity, vasculitis
7. Pulmonary hemorrhage
a. Contusions can occur with trauma. Distribution is highly variable with and interstitial to alveolar pattern. Usually most severe within 24 hours of trauma
b. Anticoagulant toxicity: Distribution is variable
8. Pulmonary abscess: Uncommon. May be focal or multifocal and either solid or cavitary
9. Cavitary lesions. Differentials should include abscess, neoplasia, parasitic disease, and granulomas if the walls are thick and irregular. Smooth, thin-walled structures are cysts, bulla, blebs, or pneumatoceles. These are most commonly congenital or traumatic origin
10. Lung lobe torsion: Increased opacity of the lung lobe with concurrent pleural effusion. May see abnormal location of the bronchus
11. Pulmonary thromboembolic disease: Variable radiographic findings (often normal). Very early may see hyperlucency and lack of terminal vessel. Much more common to see increased opacity (focal interstitial to alveolar disease in caudal dorsal lung)
12. Pulmonary infiltrates with eosinophilia (PIE): Multifocal, patchy interstitial to alveolar disease. Often seen with heartworm disease or other allergic or infectious causes
IV. Cardiac
A. Congenital
1. Patent ductus arteriosus (PDA) (left-to-right shunt): Ductus bump (enlargement of the proximal portion of the descending aorta) is the classic finding. May also see enlargement of the main pulmonary artery and left atrium or left auricle. Left-sided to generalized cardiac enlargement with pulmonary overcirculation (enlarged arteries and veins) may be present
3. Pulmonic stenosis: Enlargement of the main pulmonary artery and right ventricle. Pulmonary vessels are normal to decreased in size
4. Aortic stenosis: Elongation of the heart with prominence of the aortic arch and left ventricular enlargement
5. Endocardial cushion defects (ventricular or atrial septal defects): Variable radiographic findings dependent on size of shunt. May range from normal to severe cardiomegaly
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


