CHAPTER 44. Reproductive Disorders
Rebecca S. McConnico
MARE REPRODUCTIVE DISORDERS
I. Breeding history
A. Sequential year-by-year account of the mare’s entire career
B. Mare background: Before breeding years
C. Record of known problems
1. Abortions
2. Early embryonic death
3. Twinning
4. Neonatal deaths
D. Complete list of live foals
1. Live foals
2. Sires
3. Foaling dates
E. Detailed records of foaling years
1. Teasing date
2. Breeding date
3. Short cycles (if any)
4. Prolonged diestral patterns (if any)
5. Time of year bred
6. Age of mare at breeding
7. Young mares may have experienced abnormal cycles from training management practices
F. Mulitparous mares
1. May have reproductive conformational problems
2. Stallion knowledge
3. Management level for breeding
II. Physical examination
A. Detect any problems in other systems that could affect fertility
B. Determine behavioral issues, if any
C. Determine mare’s body condition
1. Debilitation
2. Obesity
D. Feeding and management
E. Dental care
F. Parasite control
III. Reproductive tract examination: Restrain with twitch or lip chain
A. External genitalia and perineum
1. Best evaluated during estrus
2. Conformational defects: Dorsal commissure of the vulva should be at least 4 cm dorsal to the pelvic floor
B. Vaginal vestibule
1. Windsucking: An intact vulvovaginal sphincter is present in a mare when the labia can be spread slightly without air entering the vestibule. Tone is important in preventing contamination of the cranial vagina and is absent in a chronic windsucker
2. Estrus = vaginal vestibule is pink to red in color
3. Anestrus = vestibule is pale with dry mucosa
4. Inflamed vestibule = dark red or muddy color
C. Rectal palpation of internal reproductive tract
1. Be careful to guard against trauma to the rectal mucosa
2. Do not counter against tenesmus or peristaltic waves
D. Evaluate the ovaries
1. Cup the body of the uterus with the hand, retract the uterus caudally, grasp the ovary (will need to reach laterally and dorsally). A large ovary may not be able to be grasped, but it can be stabilized for palpation
2. Mesovarium attaches to the cranial half of the ovary; locate the ovulation fossa
3. Follicles are fluid-filled structures that tend to project above the ovarian surface as they mature. Measure follicles in inches or centimeters. Collapse of the follicle is assumed to be ovulation; crater or pit formation. Corpus hemorrhagicum: Spongy but fills the crater left by the ovulation
4. Mature corpus luteum (CL) = 5 days post ovulation
E. Nonpregnant uterus palpation
1. Size, tone, consistency, and general conformation and detailed examination of abnormalities
2. Increased uterine tone indicates progesterone effects
3. Tubularity = diestrus, whereas softening = estrus and anestrus
4. Circulating estrogens cause tissue edema (uterine)
5. Anestrus: The uterine wall is flaccid, thin, and quite indistinct
6. Endometrial atrophy = anestrus
7. Use the index finger to estimate the size of the uterine horn
F. Cervical palpation
1. Estrogen causes cervical relaxation and progesterone causes turgid/firm cervix
2. Diestrus cervix is long, tubular, and readily palpable
3. Anestrus: Cervix is soft and indistinct
1. Dilation of the vagina with air. Tail should be wrapped and perineal area carefully washed with a nonirritating soap. Moist cotton is used to wipe the inner edge of the labia. Asepsis is important to prevent uterine contamination
2. Cervix is pale and dry in diestrus and soft and pink in estrus
3. Abnormalities detectable: Mucosal hyperemia, suppurative exudates, persistent hymen, urine pooling, rectovaginal defects (Figure 44-1)
 |
| Figure 44-1 Urine and debris pooled in the anterior vaginal vault of a mare with urovagina. (From Brinsko S, et al. Manual of Equine Reproduction, 3rd ed. St Louis, 2011, Mosby.) |
H. Endometrial ultrasound examination
1. Ultrasound examination
2. Visual examination of the cervix and vagina
I. Additional aids
1. Cytologic examination: Presence of neutrophils in the uterine lumen is suggestive of inflammation
2. Endometrial samples and biopsies
3. Uterine culture
4. Fiberoptic inspection
5. Dorsal commissure of the vulva
a. No more than 4 cm dorsal to the pelvic floor
b. Pneumovagina
c. Contamination
d. Wind-sucking test: Apply uniform pressure with the hands on each side of the labia
IV. Ovarian diseases
A. Gonadal dysgenesis
B. Pathologic abnormalities of the ovaries
1. Aberration of chromosomal segregation
2. Chromosomal mosaics
3. Most common abnormality: 63,X0 (missing sex chromosome)
4. Other chromosomal abnormalities: 63,X0; 64,XX
C. Testicular feminization
1. Male pseudohermaphroditism: 64,XY
2. Inherited defect consistent with either autosomal dominant sex-linked mutation or sex-linked recessive mutation
3. Major complaint is infertility
4. Barren maiden mare with stallion-like behavior
5. History of anestrus
6. May be smaller in stature
7. Teasing behavior may be agitated to passive avoidance
8. Vulva and vagina may be hypoplastic but usually normal
9. Flaccid cervix
10. Underdeveloped uterus
11. Very small ovaries
12. Ultrasound of ovaries = lack of anechoic structures (no follicular activity)
13. Does not respond to hormones
14. Plasma estrogen levels are low
15. Endometrial hypoplasia (endometrial biopsy)
16. Plasma luteinizing hormone is high due to lack of negative feed back from estrogen
17. Larger for their breed
18. Appearance of stallions
19. Small, firm inactive ovaries
20. Diagnosis
a. Clinical observation and examination
b. Rectal palpation
c. Determine sex chromatin appendages (drumsticks)
21. Prognosis and treatment: Injectable or oral progesterone may eliminate unwanted behavior
D. Ovarian hypoplasia
1. Phenotypically normal mare with infertility
2. Occasional or very irregular heat cycles
3. May allow a stallion to mount
4. External genitalia are normal
5. Uterus may be normal or undeveloped
6. Ovaries are smooth, small, with no follicular activity
E. Ovarian hematoma (post-ovulation) (Figure 44-2)
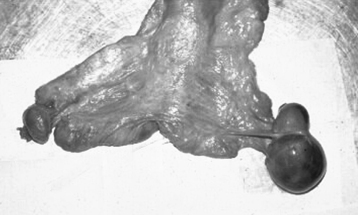 |
| Figure 44-2 Ovarian hematoma of a mare. Mares with ovarian hematomas usually continue to have regular estrous cycles and do not have contralaterally atrophied ovaries. The enlarged ovary shrinks over time. Hormone assays reveal no abnormalities in hormone concentrations. (From Brinsko S, et al. Manual of Equine Reproduction, 3rd ed. St Louis, 2011, Mosby.) |
1. Post-ovulation: Postovulation follicular hemorrhage beyond normal limits in the postevacuation phase of ovulation leads to an ovarian hematoma
3. May range in size of 5 to 12 cm but may become as large as 50 cm
4. Main differential for an enlarged ovary
5. Usually do not have abnormal behavior (compared with a mare with a testosterone-producing ovarian tumor)
6. Differences from other ovarian hematomas
a. Identification of an ovulation fossa
b. Contralateral ovary is normal in size and has follicular activity
c. Normal estrus is displayed
d. Luteinization and subsequent fertilization should occur normally
e. Ultrasound architecture: Diffuse echogenic mottling
f. May look similar via ultrasound to ovarian hematoma or normal corpus hemorrhagicum
7. Diagnosis
a. Palpate a normal ovulation fossa
b. Palpate a normal-sized and active contralateral ovary
c. Observe normal estrus behavior associated with regular estrus cycle
d. Rule out the possibility of a seasonal cause
8. Treatment
a. Most resolve spontaneously after a variable time (usually two or three estrus cycles)
b. Rarely the hematoma lasts and destroys ovarian germinal tissue
F. Ovarian abscess: Rare
1. Caused by three routes
a. Hematogenous spread
b. Ascending infection from the tubular reproductive tract
c. Local extension from surrounding infected organs (perimetritis, etc.)
2. Clinical and diagnostic findings
a. Diagnostic challenge
b. Initially, enlarged ovary; elevated rectal temperature, increased white blood cell count (WBC)
c. Chronic: Small and fibrotic; normal temperature and WBC count
d. Transrectal ultrasound
3. Treatment
a. Surgical removal
b. Broad-spectrum antibiotics
G. Ovarian cysts
1. Anovulation: Anovulatory follicles are common during transitional periods
2. Rare during the ovulatory season
3. Normal anovulation and follicular cysts
4. Pituitary and circulating levels of luteinizing hormone not produced in enough quantity for an ovulatory surge
H. Ovarian neoplasm
1. Sex chord stromal origin
a. Granulosa thecal cell tumors
(1) Benign
(2) Most common ovarian tumor
(3) Behavior: Anestrus, irregular estrus, nymphomania, stallion-like behavior
(4) Consistency: Firm and smooth or loculated, may be fluid filled, multiple follicular-like
(5) Opposite ovary: Generally small and hard with no follicular activity
(6) Endocrine: Serum testosterone is generally increased (stud-like behavior if greater than 100 pg/mL); estrogen variable; progesterone less than 100 pg/mL
b. Arrhenoblastoma
(1) Benign
(2) Extremely rare
(3) Stallion-like
(4) Smooth and firm mass on ovary
(5) Opposite ovary is generally hard with no follicular activity
(6) Serum testosterone is elevated
(7) Estrogen and progesterone are low
2. Epithelial (capsule): Adenocarcinoma (cyst)
a. Malignant
b. Extremely rare
c. Normal behavior
d. Unilobular or multilobular: Cyst adenomas and carcinomas have multiple cysts
e. Opposite ovary has normal size and activity
f. Generally nonsteroidal activity
3. Germ cell origin
a. Teratoma
(1) Benign
(2) Second most common ovarian tumor
(3) Normal behavior
(4) Consistency of tumor: Firm or multiple follicular-like with bone or cartilage palpable
(5) Irregular surface (points and edges)
(6) Usually nonsteroidal
b. Dysgerminoma
(1) Malignant
(2) Extremely rare
(3) Normal behavior
(4) Smooth surface
(5) Soft or solid, lobulated, and multicycle
V. Uterine fluid
A. A cause for reduced fertility
B. Diagnosis
1. History of breeding-associated fluid retention
2. Ultrasound diagnosis of fluid retention is most useful
3. Signs suggestive of endometritis
a. Glandular alterations
b. Failure of lymphatic drainage
c. Delay in physical clearance
d. Decreased reabsorption of lymphatic vessels
e. If greater than 1 cm identified during estrus, it should be drained
C. Treatment
1. Uterine lavage: 2 to 3 L of warmed buffered physiologic saline or lactated Ringer’s solution using a large-bore (30 French) catheter
a. It is safe to perform uterine lavage 4 hours after breeding and up to 2 days from ovulation, provided isotonic fluids are used
b. Transrectal massage of the fluid is unnecessary. Use of intravenous (IV) oxytocin (20 international units single) will help with uterine clearance
2. Use of intrauterine antibiotics or plasma is controversial yet remains under investigation
3. Summary of treatment for intrauterine fluid accumulation resulting from mating-induced endometritis:
a. Clears within 1-2 days
b. Problems more serious in older mares
c. Breeding should occur at the optimum time
d. Ultrasound examination is useful
VI. Uterine infections
A. Caused by a mixture of the following:
1. Semen
2. Bacteria
a. Streptococcus zooepidemicus (β-hemolytic)
b. Escherichia coli
c. Staphylococcus spp.
d. Klebsiella pneumoniae
e. Pseudomonas aeruginosa
f. Tayloriella equigenitalis (causative agent of contagious equine metritis [CEM])
g. Bacteroides fragilis
3. Considered contaminants
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


