CHAPTER 38. Nervous System Disorders
Rebecca S. McConnico
NEUROLOGIC EVALUATION
I. Patient profile and history
A. Signalment: Age, sex, breed, use (pasture pet, pleasure, athlete, breeding)
B. Time course of events
C. Initial problem: Peracute, acute, insidious, subtle, mild, moderate, severe
D. Associated events: Thunderstorm, trailering, breeding, history of disease, introduction of new animals, veterinary procedures
E. Vaccination status: Equine herpesvirus types 1 (EHV-1) and 4 (rhinopneumonitis), influenza, eastern equine encephalitis (EEE), western equine encephalitis (WEE), Venezuelan equine encephalitis (VEE), West Nile virus (WNV), Streptococcus equi equi, rabies
F. Feeding program
G. Abnormalities observed by the owner, such as changes in attitude at rest or work, appetite, interaction with other animals (aggressive actions, avoidance)
II. Physical and neurologic examination
A. Routine physical examination: Includes several basic neurologic tests that will usually tell the examiner whether a further detailed assessment of the neurologic system is necessary
1. Attitude
2. Eyes: Menace, pupillary light reflex (PLR), fundoscopic examination
3. Head: General symmetry (bony and soft tissues), tongue inspection, laryngeal adductor-abductor test (external “slap” test, performed by palpating the dorsolateral larynx while slapping the opposite side of the withers)
4. Neck, trunk, and limbs: Observe for normal bony and soft tissue symmetry
5. Tail and anal tone (can be done at the time of rectal temperature determination or rectal examination)
6. Evaluation of gait and posture at the walk
B. Specific neurologic examination (three parts = head + body + posture or gait)
1. Behavior: Input from owner, trainer, groom, rider (distinguish between bad habits and changes suggestive of neurologic disease)
2. Mentation: Depression
a. Systemic illness
b. Cerebrum
c. Reticular activating system (limbic system)
3. Head posture and movement
a. Standing still
(1) Head tilt (poll deviated from the muzzle), vestibular
(2) Head turn: Forebrain or cervical injury
(3) Intention tremors: Cerebellar
b. Moving to prehend food (offer handful of grass, sweet feed, or alfalfa hay)
c. Moving during gait evaluation
4. Cranial nerves (CNs)
a. Eyes
(1) Menace = positive blinking; intact vision in respective eye (ipsilateral eye and optic nerve; contralateral optic tracts and lateral geniculate nucleus)
(2) PLR: Use a strong, focused light held about 18 inches in front of the horse and perform swinging light techniques
(3) Elevate head to observe normal eye drop; then, while head is elevated, move head from side to side to induce normal vestibular nystagmus
(4) Symmetric positioning of the eyes: CN III (oculomotor), IV (trochlear), VI (abduscens), VIII (vestibulocochlear connection with the brainstem)
b. Head and face
(1) Symmetry of bones and soft tissue
(2) CN V (trigeminal): One of the largest nuclei in the brainstem: innervates muscles of mastication and sensory to the face and nostrils. Injury leads to dropped jaw and ipsilateral loss (or partial loss) of sensation to the face and inside the nares
(3) Voluntary movement of the ears, eyelids, lips: CN VII
(4) Touch: Ear → ear movement; eyelid → lid closure; lip commissure → induced smile; evaluation of sensory/trigeminal (CN V) and motor-facial (CN VII) reflexes
c. Nostrils, mouth, throat
(1) Stimulate each surface of the nasal septum = asymmetric response; suggests possible CN V (trigeminal)
(2) Tongue: Weakness and fine muscle fasciculation; hypoglossal and glossopharyngeal (CN XI and IX)
d. Horner syndrome: Cranial sympathetic denervation characterized by various symptoms in the head and cervical region
(1) Blepharoptosis
(2) Enophthalmos
(3) Prolapse of the third eyelid: Retraction of the eyeball due to paralysis of the orbital smooth muscle
(4) Miosis: Removal of sympathetic innervation of the dilator papillary muscle
(5) Increased secretion of lacrimal or nasal glands
(6) Increased cutaneous temperature: Direct results of hyperemia in denervated regions; lack of sympathetically-induced vasoconstriction which is normally mediated by α-receptors in cutaneous blood vessels
(7) Local sweating: Sweat-induced vasomotor activity of circulating epinephrine
(8) Laryngeal hemiplegia: Vasosympathetic trunk and recurrent laryngeal nerve (“slap test”)
5. Body
a. Neck and thoracic limbs or trunk and pelvic limbs
(1) Body and muscular symmetry
(2) Evidence of localized sweating, focal muscle atrophy, decreased pain response, localized pain response (variability)
(3) Cutaneous trunci reflex: Cervicothoracic reflex (panniculus); stimulates vertebral column movements
b. Tail and anus
(1) Tail tone
(2) Anal reflex
(3) Rectal examination
6. Posture and gait: Evaluated at rest, walking, trotting, turning, on an incline, freely moving in a confined pasture, paddock, or arena
a. General proprioception (conscious proprioception [CP] deficits or CP deficits)
b. Backing: Resistance to movement, lack of coordinated leg lifting
c. Negotiating obstacles (stepping over curbs)
d. Tight circling
e. Weakness
(1) Low arc and longer stride length
(2) Toe dragging
(3) Muscle tremor buckling
(4) Tail-pull resistance
(5) Hopping
f. Ataxia: Inability to control muscle coordination
g. Spasticity dysmetria
(1) Hypometria: L4-S5
(2) Hypermetria (spasticity): T3-L3 → pelvic limb
(3) Degrees of mild ataxia may be expressed with other postural movements
(4) Elevating the head and walking and tight turning
h. Paralysis or paresis (loss or partial loss of motor function)
(1) Paraplegia: Pelvic limb lesion = T3-S5; lower motor neuron (LMN) L4-S5
(2) Tetraplegia: Thoracic and pelvic limb; upper motor neuron (UMN) pelvic limb
i. Grading neurologic gait deficits
(1) 0 = no gait deficits
(2) 1 = difficult to observe but consistently observed
(3) 2 = mild to moderate deficit; exaggerated on the slope or in circles
(4) 3 = obvious to all observers when the horse moves
(5) 4 = manipulations may cause the horse to fall
(6) 5 = recumbency
7. Specific neuroanatomic diagnosis
a. Cerebrum: Abnormal behavior, seizures, depression, blindness, pseudocranial nerve changes
b. Brainstem and peripheral CNS: Depression, ataxia and weakness, specific CN deficits
c. Cerebellum: Menace deficit without blindness, intention tremor, base-wide ataxia with dysmetria
d. Spinal cord: Degrees of ataxia and weakness
e. Peripheral spinal nerves: Localized weakness, muscle atrophy, sensory loss
f. Muscular: Stiff and weak gait, local painful response elicited by palpation
C. Ancillary diagnostic tools
1. Blood and serum analysis
a. Serum chemistry
(1) Muscle: Alkaline phosphatase, creatinine phosphokinase
(2) Liver: Alkaline phosphatase, sorbitol dehydrogenase, aspartate amino transferase, γ-glutamyltransferase (GGT)
(3) Kidney: Blood urea nitrogen (BUN), creatinine
b. Serum electrolytes
c. Total white blood cell count (WBC)
d. Red blood cell (RBC) indices
e. Serology: Titers (EEE, WEE, WNV, VEE, equine infectious anemia [EIA], EHV-1, equine protozoal myelitis [EPM])
2. Imaging
a. Standing survey: Sagittal spinal column measurements
b. Nuclear scintigraphy
c. Myelography
3. Cerebrospinal fluid (CSF) analysis
a. Atlanto-occipetal (AO) cisternal space (requires general anesthesia)
(1) Landmarks are the cranial borders of the atlas and the external occipital protuberance on the dorsal median plane
(3) Key: Aim for the lower lip with the head in a very flexed position
b. Lumbosacral space, standing; requires tranquilization or recumbent patient (Figure 38-1)
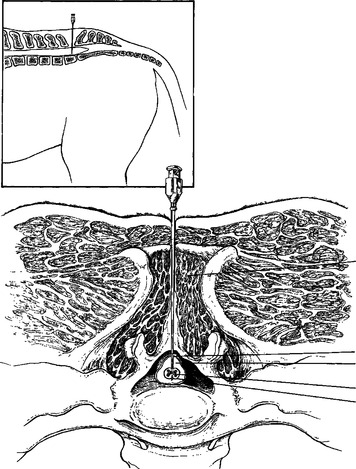 |
| Figure 38-1 Lumbosacral spinal fluid collection from a horse showing the various tissue layers that the spinal needle must pass through to obtain a sample. The spinal fluid is collected ventral to the spinal cord in the subarachnoid space. Inset, Lateral view of spinal needle placement in the lumbosacral space for collection of cerebrospinal fluid. (From Andrews FM, Adair HS III. Anatomy and physiology of the nervous system. In Auer JA, editor. Equine Surgery. Philadelphia, 1992, Saunders; modified from deLahunta A. Veterinary Neuroanatomy and Clinical Neurology, 2nd ed. Philadelphia, 1983, Saunders; From Reed SM, Bayly WM, Sellon DC. Equine Internal Medicine, 2nd ed. St. Louis, 2004, Saunders) |
(1) Landmarks are the caudal borders of the tuber coxae, the caudal edge of L6, the cranial edge of the second sacral spine, and the cranial edge of tuber sacrale
(2) Needle passes through skin → lumbosacral fascia → interarcuate ligament → dorsal dura mater → arachnoid → subarachnoid space
4. Electrodiagnostics
a. Electromyelography (EMG) for LMN disease
b. Electroencephalography for cerebral-cerebellar-brainstem lesions
c. Auditory: Evoked potentials; hearing pathways
5. Necropsy
ADULT NEUROLOGIC DISORDERS
I. Cervical vertebral instability (CVI), cervical vertebral malformation (CVM), cervical vertebral stenosis (CVS), cervical static stenosis (CSS)
A. Pathophysiology
1. CSS: Static lesion usually seen at C5-6 or C 6-7
2. CVI: Dynamic lesion usually seen at C 3-4 and C 4-5. Stenosis of vertebral canal, malformed articular processes, angular fixations; pathologic impingement on the cervical spinal cord, osteochondral lesions, focal cervical contusions; damage to white, gray matter (ventral and lateral tracts); secondary white-matter fiber degeneration; ascending pathway above lesion descending pathway below lesion; blood-brain barrier alterations; demyelination, remyelination, long-lasting ischemia, and venous occlusion
B. Signalment
1. Young, rapidly growing males
2. Age 4 months to 4 years
3. Rare in older horses unless it has gone unrecognized
4. Breed predilection: Thoroughbred, standardbred, warmblood
5. Both males and females can be affected
C. History
1. Subtle gait abnormalities in weanling or yearlings
2. Usually presented for lameness or wobbliness soon after athletic training begins; often presented after a fall → acutely ataxic
3. Neurologic examination: Localized to the cervical vertebrae
D. Clinical signs
1. Various degrees of spinal ataxia
2. UMN: Dysmetria, spasticity, and paresis of pelvic, thoracic limbs
3. Neurologic examination: Localized to cervical vertebrae
E. Differential diagnosis
1. Lameness
2. EHV-1 myelitis
3. Cerebellar hypoplasia (Arabians)
4. Equine degenerative myeloencephalopathy (EDM)
5. Fracture
6. EPM
7. Verminous arteritis
8. Mass (abscess)
F. Diagnosis
1. Neurologic examination
2. Survey radiography
a. Overgrowth of cranial articular process (C2-C6)
b. Narrowing of cervical vertebral canal
c. Enlarged vertebral epiphysis
d. Enlarged dorsal prominence of caudal epiphysis (ski slope)
e. Dorsal displacement, subluxation of vertebral head (neck flex)
3. Myelogram
a. Natural, extended, and flexed
b. Narrowing of dorsal and ventral dye column (at least 50% or greater narrowing of the dorsal contrast column is necessary for a diagnosis)
4. CSF
a. Usually normal, occasionally xanthochromic (yellow), normal pressure
b. EMG: May have LMN abnormalities in neck muscles
G. Treatment
1. Rest
2. Restrict energy intake
3. Early weaning (in early recognized cases)
4. Medical decompression (nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, dimethyl sulfoxide [DMSO])
5. Surgical decompression
II. Equine protozoal myelitis (EPM)
A. Introduction
1. Debilitating equine neurologic disease of horses
2. Affects the brain, brainstem, spinal cord, or any combination of these three areas of the central nervous system (CNS)
B. Cause
1. Caused by Sarcocystis neurona
2. Life cycle: S. neurona (Figure 38-2)
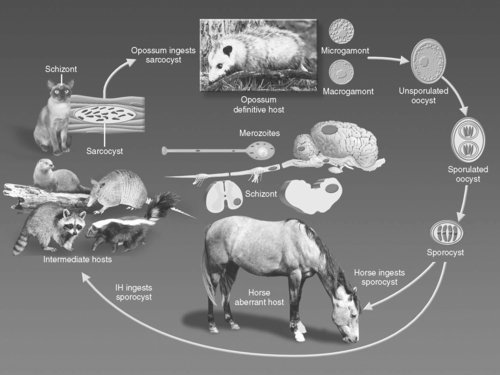 |
| Figure 38-2 Life cycle of Sarcocystis neurona. (Photo courtesy of Dr. William J.A. Saville, The Ohio State University, Columbus, Ohio.) (From Reed SM, Bayly WM, Sellon DC. Equine Internal Medicine, 2nd ed. St. Louis, 2004, Saunders) |
a. Horse is a dead-end aberrant host
b. Infectious forms of the parasite are not passed from horse to horse or from horse to the definitive or true intermediate hosts
c. Definitive host: Opossum, and other mammalian species feces (definitive host) are the source of the infection for horses
d. Opossums acquire the infection by eating infected birds (intermediate hosts)
e. Most infections come from contaminated pasture, hay, grain, and water with opossum feces. Contamination of feed and water with opossum feces may occur indirectly through other mechanisms such as birds and insects
3. Most horses in North America test positive for S. neurona antibodies
a. Exposure to the parasite, not necessarily the presence of disease, the incidence of which is much lower



