CHAPTER 33. Dermatology
Elizabeth Rustemeyer May
PRURITIC SKIN DISORDERS OF HORSES
I. Parasitic disorders
A. Mites
1. Chorioptic mange (leg mange)
a. Chorioptes equi
b. Common surface-inhabiting mite
c. Transmission via direct contact; not zoonotic
d. Clinical signs
(1) Pruritus of fetlocks and pasterns
(2) Can extend to involve the tail and perineum
(3) Typically a primary papular eruption
(4) Secondary pyoderma is extremely common resulting from self-trauma associated with pruritus
e. Diagnosis
(1) Compatible clinical signs
(2) Skin scrapings, superficial and deep (Figure 33-1)
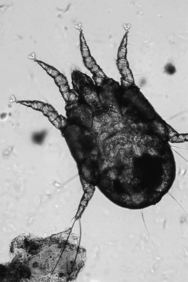 |
| Figure 33-1 Chorioptes mite (100×). (From Scott DW, Miller WH. Equine Dermatology. St Louis, 2003, Saunders.) |
f. Treatment
(1) Lime sulfur, organophosphate dips, selenium sulfide
(2) Ivermectin
(3) Fipronil spray
(4) Treat contact animals
(5) Control pruritus and treat secondary infections with appropriate antibiotic therapy
2. Sarcoptic mange
a. Sarcoptes scabiei var. equi mite
b. This is a reportable disease in the United States
c. Clinical signs
(1) Extremely pruritic
(2) Intense mane and tail pruritus
d. Treatment: Systemic therapy
(1) Ivermectin
(2) Lime sulfur dip
3. Psoroptic mange. Pruritic dermatitis or pruritic otitis
a. Non-burrowing mites
b. Live on skin surface, under crusts
c. Begins as mane and tail pruritus but can become generalized
d. Treatment: Ivermectin
B. Pediculosis (lice infestation)
1. Lice are species specific
a. Anoplura
(1) Haematopinus asini—sucking louse
(2) Favor the mane, tail, and fetlock
b. Mallophaga
(1) Bovicola equi—biting louse
(2) Prefer the dorsolateral trunk
2. Transmitted via direct contact
3. Clinical signs consistent with pruritus and chronic self-trauma
4. Easily diagnosed with direct visualization or tape cytology and microscopic examination
5. Treatment
a. Provide sound nutrition and avoid overcrowding
b. Most parasiticides will kill lice
c. Treat all in-contact animals
C. Culicoides hypersensitivity
1. Very common
2. Type I hypersensitivity—thought to be hereditary
3. Many species exist; all feed at night
4. Occurs seasonally
a. Symptoms may worsen each subsequent year
b. Lesions secondary to pruritus
5. Diagnosis: Clinical signs, intradermal allergy testing
D. Insect hypersensitivity
1. Simulium spp. = blackfly
2. Tabanus spp. = horse fly
3. Stomoxys calcitrans = stable fly
4. Haematobia spp. = horn fly
II. Atopy (atopic dermatitis)
A. Inherited predisposition for the development of hypersensitivities to environmental allergens associated with the production of allergen-specific immunoglobulin E (IgE) antibodies
B. Type I hypersensitivity disorder
C. Not well documented in the horse
D. Development of clinical signs requires a second exposure (the challenge) following the initial exposure (sensitization). Allergen-specific IgE is produced in response to exposure to a previously encountered allergen
E. Clinical signs
1. Seasonal to nonseasonal pruritus
2. Most lesions secondary to self-trauma
F. Diagnosis: Pruritus is the hallmark of this disease
1. Rule out other pruritic causes of skin disease
2. This is a diagnosis of exclusion
3. Allergy testing (intradermal testing) is used to determine any allergies the animal has, not to diagnose atopy
G. Treatment
1. Avoid the allergen if possible
2. Hyposensitization vaccine therapy
3. Corticosteroids are very effective when used correctly and judiciously
4. Antihistamines can be used in combination with fatty acids or corticosteroids to use lower doses of corticosteroids in some animals
5. Topical antipruritic and bathing therapy will help decrease allergen exposure
III. Adverse reaction to food (food allergy)
A. Mechanism of disease is not currently known
B. This is not well documented in the horse
C. Diagnosis
1. Elimination diet trial
2. Decrease in pruritus of 50% or greater
3. Diagnosis confirmed by increase in pruritus with food challenge
D. Treatment
1. Avoid the offending dietary allergen
2. Some animals will respond to antihistamine or fatty acid therapy
IV. Focal ventral midline dermatitis
A. Seasonal: Spring to fall
B. Mechanical irritation from biting flies. Haematobia spp. = horn fly
C. Well-demarcated area of lichenification, ulceration, crusts around the umbilicus
D. Diagnosis
1. History and clinical signs
2. Rule out other causes
E. Treatment
1. Treat secondary infections
2. Prevent fly exposure
SCALING AND CRUSTING DISORDERS
I. Infectious disorders
A. Bacterial causes
1. Dermatophilosis (rain rot)
a. Common in horses
b. Dermatophilus congolensis
c. Only known source is other animals; however, this is not considered a highly contagious disease
d. For an infection to develop must have
(1) Moisture
(2) Skin microtrauma
e. Clinical signs
(1) Thick crusts with matted hair (paintbrush crusts)
(2) Eroded skin surface below crusts when removed
(3) Lesions are often painful but can also become pruritic
(4) Photodermatitis in nonpigmented areas
f. Diagnosis
(1) Cytology of crust material
(2) Branching organism can be identified microscopically (Figure 33-2)
 |
| Figure 33-2 Dermatophilosis. Coccoid organisms are present as branching filaments (“railroad tracks”). (From Scott DW, Miller WH. Equine Dermatology. St Louis, 2003, Saunders.) |
(3) Culture may be required
g. Treatment
(1) Systemic antibiotic therapy
(2) Topical antiseborrheic and antimicrobial shampoos
2. Bacterial folliculitis and furunculosis
a. Typically caused by Staphylococcus aureus or Staphylococcus pseudintermedius
b. Secondary to skin microtrauma
c. Classifications
(a) Papules to nodules beginning in the saddle area
(b) Typically occurs during warmer weather
(2) Pastern folliculitis
(a) Restricted to the pasterns and fetlocks
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


