CHAPTER 22. Orthopedic Disorders
Patricia A. Schenck
FRACTURES OF THE SKULL
I. Zygomatic arch fracture
A. Preoperative considerations
1. Perform a neurologic examination
2. Confirm that the optic nerve and vision is intact before surgery
3. Computed tomography (CT) provides the best assessment
B. Surgical procedure: Reduce fractures that cause compression of the eye
C. Postoperative care and complications: Monitor neurologic function. Degenerative joint disease (DJD) of the temperomandibular joint (TMJ) may result long-term. Prognosis is good
II. Extracranial fractures: Fractures of the nuchal crest, sagittal crest, or frontal sinus
A. Preoperative considerations: Perform neurologic examination
B. Treatment: Most are managed conservatively. Surgery is performed if displacement is severe
C. Postoperative care and complications: Monitor neurologic function. Subcutaneous emphysema may occur secondary to frontal sinus fracture
III. Intracranial fractures
A. Preoperative considerations
1. Perform a neurologic examination
2. Most are closed fractures
3. Calvarial fractures are usually associated with central nervous system (CNS) compromise
B. Surgical procedure: Elevate depressed calvarial fractures, and remove comminuted pieces
C. Postoperative care and complications: Monitor neurologic function. Prognosis is guarded for neurologic recovery
FRACTURES AND DISLOCATIONS OF THE MANDIBLE
I. Anatomy
A. About 15% of all fractures in cats are of the mandible
B. The mandibular canal contains the mandibular artery and vein and the mandibular alveolar nerve
II. Clinical signs: Asymmetry of the jaw, oral hemorrhage and pain, crepitus, concurrent head and thoracic trauma
III. Diagnosis: Based on history and radiographs; CT can provide a three-dimensional (3-D) impression
IV. Surgical procedures
A. Preoperative considerations: Monitor neurologic function, and check for diaphragmatic hernia, pneumothorax, and other conditions
B. Anesthetic considerations: Place an endotracheal tube through a pharyngotomy incision. Give antibiotics because most mandibular fractures are open
C. Surgical principles: Restore normal dental occlusion. Intramedullary pinning is not recommended
D. Postoperative care: Maintain nutrition with an esophagostomy or gastrostomy feeding tube. If not using a feeding tube, feed a soft gruel for 4 weeks post surgery. Flush the mouth daily with dilute chlorhexidine solution
E. Complications: Malocclusion is the most important complication; osteomyelitis occurs rarely
V. Mandibular symphyseal separations
A. Occurs often in cats
B. Wire stabilization is the technique of choice
VI. Mandibular body fractures
A. Create a muzzle using tape (Figure 22-1)
 |
| Figure 22-1 Procedure for creating a tape muzzle. (From Birchard SJ, Sherding RG, editors. Saunders Manual of Small Animal Practice, 3rd ed. St Louis, 2006, Saunders.) |
1. Can be used if there is minimal displacement of fragments
2. Difficult to do in cats or in brachycephalic breeds
3. Feed soft gruel
B. Maxillary-mandibular fixation: Either wire the maxilla to the mandible or use acrylic bonding of the canine teeth to keep the mouth closed
C. Interfragmentary wiring: For fracture fragments that are stable without loss of bone or comminution
D. Intraoral acrylic splint
E. External skeletal fixation: Best used for fractures that are open, comminuted, or involve bone loss
F. Bone plating
VII. Mandibular ramus fractures
A. Usually do not require surgical treatment because displacement is minimal
B. Condylectomy can be performed in those that develop an inability to open the mouth
VIII. TMJ dislocations
A. Usually occurs from trauma
IX. TMJ dysplasia
A. Jaw locks in the open position. Reported in Irish setters, cocker spaniels, and basset hounds
B. May require condylectomy or resection of the zygomatic arch
FRACTURES OF THE MAXILLA
I. Etiology
A. Most are the result of trauma
B. More likely in young dogs and cats
II. Clinical signs include asymmetry of the maxilla, oral pain and bleeding, nasal hemorrhage
III. Diagnosis
A. History and radiographs. More than one fracture may be present
B. CT gives a 3-D view
IV. Preoperative considerations
A. Manage concurrent head, airway, and thoracic trauma. Maintain an airway and treat shock
B. Complete a neurologic examination
V. Anesthetic considerations
A. Place endotracheal tube through a pharyngotomy incision
B. Give antibiotics because many maxillary fractures are open
VI. Surgical fixation
A. Restore dental occlusion
B. Maintain patent nasal passages
C. Midline maxillary separations (traumatic cleft palate)
1. Occurs frequently in cats
2. Wide defects should be surgically closed
D. Maxillary body fractures: Most do not require surgical treatment. Stabilization techniques used for mandibular fractures can be used for maxillary body fractures
E. Postoperative care: Maintain adequate nutrition. Use gastrostomy or esophagostomy feeding tube. If not using a feeding tube, feed soft gruel
F. Complications include dental malocclusion and osteomyelitis
NEOPLASIA OF THE MAXILLA AND MANDIBLE
I. Causes
A. The oropharyngeal region is the fourth most common site of malignant neoplasia in the dog
B. The most common oral neoplasms in the dog are malignant melanoma, squamous cell carcinoma (SCC), fibrosarcoma, and epulides. SCC is the most common in cats
C. Boxers, golden retrievers, and cocker spaniels are predisposed to oral tumors. Small-breed dogs are more prone to develop malignant melanomas, and large-breed dogs are more prone to SCC and fibrosarcoma
D. Surgical resection is the first line of therapy for all oral tumors
II. Diagnosis
A. History includes drooling, halitosis, and dysphagia. Deformity of the muzzle may be present. Most are painful, so anorexia is common
B. Physical examination: Consider sedation. Most metastasize via the lymphatic system so examine lymph nodes
C. Diagnostic evaluation includes complete blood cell count, chemistry profile, radiographs of skull and chest. CT and magnetic resonance imaging (MRI) are helpful in evaluating the extent of invasion. Biopsy is important in determining treatment
III. Tumor types
A. Benign nonodontogenic neoplasms
1. Epulis
a. Fibrous tumor originating from the periodontal ligament
b. Rare in cats, common in dogs. The boxer is predisposed
2. Other tumors include fibroma, hemangioma, lipoma, chondroma, osteoma, and histiocytoma
B. Malignant nonodontogenic neoplasms
1. Malignant melanoma
a. Often is locally invasive with early metastasis
b. May be pigmented or nonpigmented
c. Usually ulcerated, so oral bleeding and halitosis are common
d. Treatment is complete surgical resection. Radiation therapy has moderate success. Chemotherapy is not effective
a. Second most common oral tumor in dogs, most common tumor in cats
b. Nontonsillar SCC is locally invasive and slow to metastasize. Tonsillar SCC is very aggressive, with early metastasis to lymph nodes and lungs
c. Wide surgical resection is the treatment of choice, with or without radiation therapy. Chemotherapy may be added to treatment
d. Prognosis is guarded as recurrence is high
3. Fibrosarcoma
a. Third most common oral tumor in dogs; second most common in cats
b. Slow-growing, locally aggressive, late to metastasize
c. Local recurrence is common
d. Surgical resection is the treatment of choice. Radiation and chemotherapy can also be used in conjunction
4. Other malignant nonodontogenic neoplasms include osteosarcoma (OSA), adenocarcinoma, transmissible venereal tumor, mast cell tumor, hemangiosarcoma, and tonsillar lymphosarcoma
5. Malignant odontogenic neoplasms
a. Ameloblastoma arises from the dental laminar epithelium. Rare tumors but more common in younger dogs
b. Odontomas can invade all dental tissues and are rare
c. Surgical resection is the treatment of choice
IV. Surgery
A. Preoperative considerations
1. Knowledge of anatomy is necessary
2. Maxillectomies are associated with significant blood loss, so have a source of blood replacement
3. Administer nonsteroidal antiinflammatory drugs (NSAIDs) and fentanyl patches to minimize postoperative pain
4. Use cuffed endotracheal tube
5. Give antibiotics
B. Objectives are to resect completely the neoplasm and preserve local blood supply
C. Procedures for surgery include maxillectomy (unilateral or bilateral), hemimaxillectomy, and mandibulectomy
D. Postoperative care
1. Pain control
2. Elizabethan collar to prevent self-mutilation
3. Feed soft gruel for 1 month post surgery. Flush the oral cavity after eating. Maintain nutrition
4. Reevaluate every 3 months for the first year. Watch for metastasis
E. Complications
1. Transient facial edema resolves after a few weeks
2. Nasal discharge, facial swelling, noisy respiration, and inappetence often occur
3. The most common complication is dehiscence
FRACTURES AND DISLOCATIONS OF THE SPINE
I. Atlantoaxial instability
A. Anatomy
1. A pivot joint that allows the head to rotate around an axis
2. The dens is on the ventral surface of C2 (the axis) that projects into the floor of C1 (atlas)
B. Causes
1. Congenital causes are most common and are seen in young, small and toy-breed dogs. Instability arises from malformation of the dens, lack of ligamentous support, or congenital absence of the transverse or atlantoaxial ligaments
2. Acquired causes are the result of trauma and can happen at any age or breed of dog or cat
C. Clinical signs
1. Vary from pain to ataxia or tetraplegia. The severity is dependent on the degree of subluxation
2. If the dens luxates dorsally into the spinal cord, the signs are more severe
3. If the spinal cord suppression is severe, respiratory arrest and death can occur
D. Diagnosis
1. Radiographs are necessary and reveal a widened space between the dorsal arch of C1 and the dorsal spine of C2
2. CT and MRI are not required
E. Surgical procedures
1. Do not flex the spine, which can exacerbate cord compression
2. Objectives are to remove the fractured or ununited dens, stabilize the C1-C2 articulation, and prevent spinal cord injury
3. A dorsal approach or ventral approach can be used. The ventral approach is more difficult but has a higher success rate
4. Complications include infection, dysphagia, laryngeal paralysis, or surgical failure
5. Manage pain, administer antibiotics, and place an Elizabethan collar for 2 weeks. Restrict exercise for 4 to 6 weeks
II. Caudal cervical spondylomyelopathy (wobbler syndrome)
A. Anatomy
1. The dorsal components that play a role include the dorsal vertebral lamina, the articular facets and joint capsule, and the ligamentum flavum
2. The ventral components that play a role include the vertebral bodies, the dorsal fibers of the annulus fibrosus of the intervertebral disc, and the dorsal longitudinal ligament
B. Causes
1. Two populations of dogs get wobbler disease. About 10% to 15% are young Great Danes with osseous malformations of the cervical spine. The remainder are middle-aged to older dogs with acquired disease secondary to cervical vertebral instability. Doberman pinschers make up about 80% of this group. Labradors and dalmatians are also predisposed.
a. With congenital osseous malformation, there is malformation or malarticulation of the articular facets and vertebral bodies, which causes dorsal and lateral stenosis of the spinal canal. C3 to C7 bodies are most often affected. Stenosis is seen and gets worse with age. Heredity, nutritional imbalance, or trauma may play a role
b. Vertebral tipping is seen in middle-aged to older patients. There is a malposition of the vertebral body caudal to the affected intervertebral disc. The cranial aspect of the affected vertebra is displaced dorsally, causing spinal compression. The C5 to C6 and C6 to C7 spaces are most commonly affected
c. Chronic degenerative disc disease with cervical vertebral instability occurs most in Doberman pinschers and is caused by concurrent dorsal annulus and dorsal longitudinal ligament hypertrophy. The caudal cervical intervertebral disc spaces are affected most commonly
d. Ligamentum flavum hypertrophy causes dynamic dorsal spinal canal compression and is associated with vertebral arch abnormalities
e. Hourglass compression is associated with dorsal, ventral, and lateral compression and occurs most commonly in young Great Danes
C. Clinical signs
1. A chronic, progressive history of neck pain, hypermetria, ataxia, and tetraparesis is common
2. Compression worsens with neck extension
3. The clinical signs may wax and wane; occasionally there will be an acute deterioration
4. Ataxia is usually worse in the rear limbs. Proprioceptive deficits are present, with paraparesis progressing to tetraparesis. In the thoracic limb, there is usually muscle atrophy of the spinatus muscle of the shoulder
D. Diagnosis
1. Differentials include degenerative spinal cord disease, ischemic myelopathy, discospondylitis, congenital spinal cord disease, inflammatory CNS disease, spinal neoplasia, brachial plexus tumor, subarachnoid cysts, and trauma. Ischemic myelopathy is not associated with cervical pain, however
2. Myelography is helpful in identifying the site of compression
3. CT may be helpful in identifying dorsal arch abnormalities and osseous malformations in the Great Dane
4. MRI is the gold standard for imaging of the spine because MRI gives the greatest detail of soft tissue structures
E. Surgical procedures
1. The three primary decompressive surgeries are ventral decompression using a ventral slot technique, ventral distraction and fusion using a polymethylmethacrylate (PMMA) plug, and dorsal decompression using a dorsal laminectomy
2. The choice of procedure is based on where the compression is located (dorsal or ventral), the number of spaces involved, and whether it is dynamic or static
F. Postoperative care and complications
1. Manage pain (Fentanyl patch); give NSAIDs
2. Administer antibiotics for 5 days post surgery
3. Provide nursing care for the recumbent patient
4. Restrict activity for 3 to 6 months post surgery. Use a harness rather than a collar for a dog
5. Obtain radiographs monthly until there is complete bony fusion at the atlantoaxial joint (usually in 8-12 weeks)
6. There is usually about an 80% return of function, but about 30% have recurrences within 2 years
III. Spinal fractures and dislocations
A. Introduction
1. Most are due to trauma
2. Repair depends on the region of the lesion, amount of neurologic dysfunction, body size, and other injuries
3. The thoracolumbar and lumbosacral junctions are prone to fracture and luxation
B. Causes
1. Hyperextension is due to direct trauma to the dorsal spine, with collapse of the dorsal compartment
2. Hyperflexion results in a wedge compression fracture of the vertebra, sparing the dorsal compartment. These fractures are usually stable
3. Compression occurs with an axial load force, and fragments and extruded nucleus pulposus can be driven into the spinal cord
4. Rotation is usually associated with hyperextension, and disruption of both ventral and dorsal compartments occur
C. Clinical signs may range from pain or proprioception loss to loss of motor function
D. Diagnosis
1. Perform a complete physical examination, including a neurologic examination
2. Obtain thoracic and abdominal radiographs. Myelography is not indicated. CT is best for identifying bony pathology; MRI is best for soft tissue visualization
3. Most important for prognosis is the presence of deep pain. If deep pain sensation is intact, there is an 85% to 90% chance of recovering normal neurologic function. If deep pain is absent, there is only a 15% chance of neurologic function recovery
4. Immobilize the patient to prevent additional spinal cord damage
E. Preoperative considerations
1. If the fracture is stable with minimal displacement and the patient has good motor function, the patient can be managed without surgery
2. Surgery is indicated if the fracture is unstable or significantly displaced, if motor function is diminished, or there is evidence of declining neurologic function
1. For cervical fractures, most occur at the dorsal spine or body of C2. A ventral approach to the cervical spine provides the best bone structure for fixation
2. The thoracolumbar junction and lower lumbar-lumbosacral space are the most common locations of fracture or luxation in the thoracic and lumbar spine. The most common techniques are dorsal spinous process plating using plastic spinal plates and pin and PMMA fixation
3. Fractures of L6, L7, and the sacrum are common; signs are related to sciatic, femoral, and sacral nerve deficits. A dorsal approach is used for fixation
G. Postoperative care and complications
1. Minimize pain, begin antibiotic therapy, and provide nursing care for the recumbent patient
2. Begin physical therapy soon after surgery
3. Make sure there is urinary control; if not, express the bladder every 6 hours. Avoid indwelling urinary catheters
4. If deep pain sensation is present, about 85% will regain near-normal neurologic function
NEOPLASIA OF THE AXIAL SKELETON
I. Causes
A. OSA and chondrosarcoma are the most common neoplasms
B. Hemangiosarcoma and fibrosarcoma should also be considered
C. Multilobular osteoma is the most common tumor of the skull
II. Clinical signs
A. Usually presented for a swelling over a bone
B. Neoplasias of the rib may lead to respiratory signs
C. Skull tumors may lead to neurologic signs
D. Pelvic tumors may result in constipation
III. Diagnosis
A. Radiographic signs may range from primarily lytic to proliferative lesions
B. Polyostotic lytic lesions are seen with lymphoma and multiple myeloma
C. Determine whether metastases are present; especially check regional lymph nodes and lungs
D. OSA or multilobular osteoma of the cranium appears as proliferative bony lesion of flat bones
E. Cerebrospinal fluid evaluation is usually normal but may reveal increased levels of protein and elevated pressure with vertebral neoplasia
F. Myelography and CT can determine the exact site of the tumor and how much spinal cord compression is present
G. Bone biopsy is necessary for a histopathologic diagnosis
IV. Treatment
A. Rib neoplasia
1. Completely remove the mass with wide normal margins
2. Prevent abnormal chest wall movement
3. Prevent pneumothorax
4. Monitor for hemorrhage, seroma formation, and pneumothorax. Manage pain
5. Neoplasms are usually malignant. Consider chemotherapy if excision was not complete
6. Metastases may have occurred even if the tumor has been resected
B. Pelvic neoplasia
1. The ileal wing can be resected for localized tumors. Avoid hemorrhage and nerve damage
2. Monitor for seroma formation and infection
3. Manage pain
4. Consider chemotherapy if the tumor is malignant
C. Vertebral neoplasia
1. Remove as much of the tumor as possible and decompress the spinal cord
2. Administer dexamethasone prior to surgery to minimize spinal cord edema from manipulation
3. Perform multiple neurologic examinations
4. Monitor for urine retention
5. Consider chemotherapy
6. The prognosis for malignant vertebral tumors is poor
FRACTURES OF THE SHOULDER
I. Anatomy
A. Fractures are often associated with brachial plexus injuries or soft tissue injury
B. Suprascapular nerve crosses the scapular neck beneath the acromion
C. Cephalic vein is on the superficial craniolateral aspect of the greater tubercle of the humerus
D. Circumflex humeral vessels are distal to the teres minor, beneath the deltoideus muscle
II. Diagnosis
A. Clinical signs include lameness of the forelimb and pain or crepitus on palpation of the scapulohumeral joint
B. Radiography is required for diagnosis. CT is useful because of the 3-D views
III. Fractures of the scapula
A. Fracture of the scapular body is most common
B. If there is minimal displacement, treat with strict cage confinement
C. Because there are many tendons and muscles around the scapulohumeral joint, osteotomy of the acromion or greater tubercles may be required. These can then be reattached by screws
D. Scapular body fractures are often transverse or oblique. Because the scapula is thin, treat with cage rest if at all possible
E. Fractures of the spine of the scapula do not require surgery
F. Fractures involving the acromion require surgery with tension band or lag screw fixation
G. Fractures of the scapular neck require surgery for fixation. Be careful to protect the suprascapular nerve
H. Supraglenoid tubercle fractures require surgical fixation. In immature animals, the secondary center of ossification of the supraglenoid tubercle can be confused with a fracture
J. The prognosis is good for healing and normal function if there is good stabilization
K. Restrict activity for about 8 to 12 weeks
L. Complications include suprascapular nerve injury, osteoarthritis (OA), and decreased limb function. Suprascapular nerve injury results in atrophy of the supraspinatus muscle
IV. Proximal humeral fractures
A. These fractures are uncommon but occur mostly in immature animals (Salter-Harris type I, II, or III fractures). The physis of the proximal humerus is radiographically closed by 10 months of age
B. If there is a proximal humeral fracture in an older dog, evaluate for bone lysis or cortical thinning, which could indicate OSA
C. Surgery is required. Repair is usually with Steinmann pins and wire
D. Avulsion fractures of the greater or lesser tubercle occasionally occur in immature animals
E. For Salter-Harris I or II fractures, do a craniolateral approach. In young animals, use Steinmann pins and Kirschner wires. In older animals, use lag screws and Kirschner wire
F. For Salter-Harris III fractures, in young animals, use lag screws and Kirschner wire. In older animals, screws and a T plate can be used
G. Fractures of the humeral neck occur in older animals. Stabilize with a T plate or with Rush pins or Kirschner wires. Restrict to cage rest until signs of healing are seen on radiographs. Malunion occurs rarely. If there is good stabilization, these fractures heal rapidly
SCAPULOHUMERAL LUXATION
I. Causes
A. Occurs uncommonly
B. Medial luxation is most common, especially in small-breed dogs
C. Lateral luxation occurs in larger dogs
II. Clinical sign is forelimb lameness
III. Diagnosis is based on physical examination and radiography
IV. Closed reduction
A. Medial luxation
1. Flex elbow and pull limb laterally while exerting pressure on the scapular spine
2. Use general anesthesia
3. Place in a Velpeau sling for 2 weeks
4. Restrict exercise for another month. Swimming is a good exercise
B. Lateral luxation
1. Use general anesthesia
2. Flex elbow and extend the shoulder while rotating the humeral head upward
3. Use spica splint for 2 weeks
V. Open reduction
A. Use general anesthesia
B. Open reduction can be challenging and involves surgery to stabilize the joint
C. Postoperative care involves pain control, minimizing postsurgical inflammation, and encouraging movement of the distal extremity. Provide strict crate confinement for 3 weeks with leash walks
D. The prognosis is good if stabilization is adequate
FRACTURES OF THE HUMERUS
I. Anatomy
A. The radial nerve lies within the musculospiral groove of the humerus
B. On the lateral side, identify the lateral head of the triceps, the brachialis, the brachiocephalicus, and acromial head of the deltoid muscles. The radial nerve is also more lateral
C. On the medial side, identify the medial head of the triceps, the biceps brachii, and the median and ulnar nerves
II. Causes. Most are due to trauma (hit by a car) or a fall from excessive heights
III. Diagnosis
A. Diagnosis is based on radiographic findings
B. Check for other thoracic trauma such as pneumothorax, diaphragmatic hernia
IV. Proximal humeral physeal fractures
A. Seen in young dogs before physeal closure takes place
B. Surgery is usually required for fixation
C. Use a cranial approach and fix with Kirschner wires or Steinmann pins
D. Restrict activity but encourage range of motion activity
V. Proximal diaphyseal fractures
A. Least common diaphyseal fracture
B. Evaluate brachial plexus and radial nerve
C. Many occur secondary to metabolic bone disease
D. Surgery is necessary
E. Use a cranial approach. A single intermedullary pin may not provide rotational stability. Can use two Rush pins, Steinmann pins, or a bone plate
F. Encourage early range of motion with restricted exercise
VI. Diaphyseal fractures
A. These fractures are often spiral and can entrap the radial nerve
B. Muscle contraction causes overriding of fragments
C. Closed reduction can be attempted early after injury
D. For surgery, use a lateral approach
E. In small breeds, a combination of pins, wires, or external fixation can be attempted. When using pins, retrograde the pins into the proximal fragment from the fracture site
F. In large breeds, interlocking nails have been used. Plate fixation can be successful but is difficult because of the vessels and nerves present. Medial plate placement is easier
G. If external fixation is used, remove it in 4 to 6 weeks. Remove intramedullary pins following fracture healing
VII. Supracondylar fractures
A. Rigid internal fixation is necessary
B. Steinmann pins or double Rush pins can be used. In larger dogs, small bone plates can be used
VIII. Condylar fractures
A. Most condylar fractures involve the lateral portion of the condyle, which carries most of the force through the elbow joint because of the articulation with the radial head
B. Spaniels and rottweilers have a heritable defect in which the humeral condyle does not completely ossify. This predisposes them to this fracture
C. Surgery is usually necessary
D. Transcondylar lag screws with Kirschner wire are used. Using crossed Kirschner wires is not recommended
E. Arthritis and reduced range of motion are common complications
IX. Intercondylar fractures of the humeral condyles
A. These are very difficult to repair, as the condyles are split, in addition to the supracondylar fracture
B. Fix the two condyles together first, then fix the supracondylar fracture
C. Lameness and OA are common complications
FRACTURES AND GROWTH DEFORMITIES OF THE RADIUS AND ULNA, LUXATION OF THE ELBOW
I. Fractures of the radius and ulna
A. Introduction
1. Commonly seen
2. Usually the result of trauma or from falling or jumping
3. Open fractures of the distal part of the radius and ulna are common
B. Anatomy
1. The radius is the main weight-bearing bone of the forelimb and is shorter than the ulna. The ulna is the longest bone in the body
2. The radial and interosseous arteries provide the main arterial supply. The radial, median, and ulnar nerves supply the antebrachium and paw
C. Preoperative considerations
1. Evaluate for concurrent injuries
2. Evaluate neurologic function
D. General objectives of surgery
1. Allow early return to weight bearing
2. Preserve neurovascular structures
E. General postoperative care and complications
1. Use a soft padded bandage for 3 to 10 days to reduce postoperative swelling
2. Reevaluate with radiographs every 3 to 4 weeks. Restrict activity until the fracture has healed
3. Complications include delayed healing and nonunion. If the fracture has not been stable, DJD can occur. If the animal is immature, there may be premature closure of the growth plates
F. Olecranon fractures
1. The triceps attached to the olecranon. Counteract the forces of the triceps by using the tension band principle and converting it into a compressive force
2. Use small intramedullary pins or K-wires across the fracture, then place wire around the pins in a figure-eight fashion
G. Trochlear notch fractures
1. Because this is an articular fracture, there must be good alignment of the fracture with rigid fixation
2. Counteract the forces of the triceps by using the tension band principle
3. Use intramedullary pins, K-wires, or bone plates. Contour the bone plate to the caudal or caudolateral side of the ulna
H. Radial head fractures
1. Precise reduction with rigid fixation is necessary
2. Use K-wires and lag screws to fix
I. Radial neck and proximal physeal fractures
1. In immature animals, stabilize without compression to prevent premature closure of the growth plate
2. Stabilize so that the radial head articulates properly with the humeral condyle
3. Use K-wires. Do not penetrate the articular surface of the radius
4. Remove the K-wires in 3 to 4 weeks
J. Monteggia fractures
1. Refers to a fracture of the ulna with a radial head luxation
2. Stabilize the ulnar fracture and reduce the radial head luxation
K. Mid-shaft radial and ulnar fractures
1. Maintain proper angulation, rotation, and length of the limb
2. Prevent synostosis of the radius and ulna in immature animals
3. Closed reduction and cast fixation
a. Used for minimally displaced transverse fractures
b. Flex the elbow in a functional angle, and place the carpus is a slight varus position
c. Apply a fiberglass cast, working from distal to proximal
4. External fixation is used for comminuted fractures and simple fractures
a. Reduce the fracture closed if possible
b. Place three or four pins on each side of the fracture line
L. Plate fixation for distal metaphyseal fractures
1. Occur primarily in small dogs
2. High incidence of nonunion if the fracture is not stable
3. Align the fracture with compression, and insert a cancellous bone graft
M. Fractured styloid process of the ulna
1. Reduce and stabilize the fracture with K-wires and wire in a figure-eight configuration
2. Splint for 3 to 4 weeks postoperatively
II. Growth deformities of the radius and ulna
A. Anatomy
1. Deformities result from trauma and disruption of the blood supply to the physis, with synostosis of the radius and ulna
2. The physes of the radius and ulna close at about 7 to 9 months of age in dogs
4. The distal radial physis contributes about 60% and the proximal radial physis contributes 40% to the longitudinal growth of the radius
5. The radius and ulna must grow in a synchronous fashion to attain a normal shape
B. Preoperative considerations
1. Early recognition and treatment are important
2. Obtain radiographs and determine whether physes are open or closed
C. General postoperative care and complications
1. In immature dogs, splint the limb, and reevaluate radiographically every 3 weeks
2. The prognosis is guarded, especially for mature dogs with severe deformities
D. Surgical procedure to correct premature closure of the distal ulnar physis
1. In immature dogs, remove a section of the ulna to allow unrestrained growth of the radius, and prevent regrowth by placement of a fat graft
2. In mature dogs, there is cranial or medial bowing, carpal valgus, limb shortening, and malalignment of the radius/ulna in the elbow
3. Objectives are to correct the angular deformities, and maintain as much limb length as possible
4. Perform an osteotomy of the radius at the point of maximal curvature
E. Surgical procedure to correct premature closure of the proximal radial physis
1. Usually not recognized until after the bone growth of the radius is finished
2. There is distal luxation of the radial head from the humerus, and the leg is straight
3. The objective is to articulate the radial head with the humerus and ulna
F. Surgical procedure to correct premature closure of the distal radial physis
1. In the immature dog with complete closure, there is distal luxation of the radial head, and the limb is shortened. The leg remains straight, and the radius and ulna bow rarely. The objective is to remove a section of the radius to allow unrestricted growth of the ulna
2. In the immature dog with partial lateral closure, there is carpal valgus with external rotation, cranial and medial bowing of the forelimb, and shortening of the limb. The objective is to remove the closed portion of the distal radial physis and prevent bony bridging of the removed physis
3. In mature dogs, the objective is to reestablish congruity to the elbow joint and to correct the angular deformity of the limb
III. Traumatic luxation of the elbow
A. Lateral luxation is common because the medial condyle of the humerus is larger which prevents medial luxation
B. Clinical signs include acute non-weight-bearing lameness; the foot and antebrachium are abducted, and flexion and extension of the elbow are not possible
C. Diagnosis is via radiography
D. Most elbow luxations can be treated by closed reduction if treatment is initiated within the first 3 days after the injury (Figure 22-2)
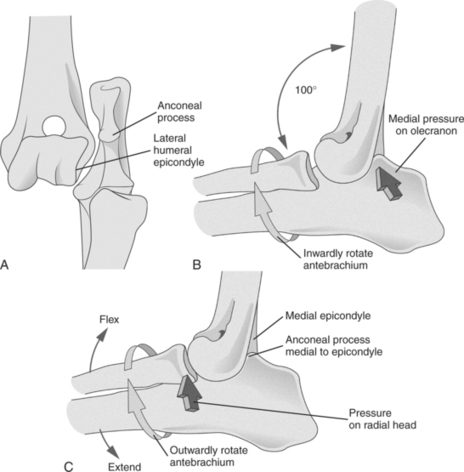 |
| Figure 22-2 A, For closed reduction of a laterally luxated elbow (B), flex the elbow and inwardly rotate the antebrachium to hook the anconeal process into the olecranon fossa. C, Then extend the elbow slightly and abduct and outwardly rotate the antebrachium while placing pressure on the radial head. (From Fossum TW. Small Animal Surgery, 3rd ed. St Louis, 2007, Mosby.) |
E. If elbow fractures are present, then surgery is indicated. Surgical reduction is difficult
F. Keep the elbow extended to maintain reduction, obtain radiographs to confirm reduction. Put in a lateral splint to maintain elbow extension. Maintain the splint for 2 weeks, then allow leash walks for another 2 weeks
FRACTURES AND DISLOCATIONS OF THE CARPUS
I. Introduction
A. Usually the result of trauma. Isolated fractures of the carpus are rare, usually occurring in greyhounds or working dogs
B. Fractures usually involve the articular surface so rigid fixation is necessary
II. Anatomy
A. Osseous structures
1. The seven bones are arranged in two rows. The proximal row includes the radial, ulnar, and accessory carpal bones. The distal row consists of the C1, C2, C3, and C4 carpal bones
2. The radial bone is the largest, is located medially, and articulates with the radius proximally, and with C1, C2, C3, and C4 distally
3. The ulnar carpal bone is lateral and articulates with the radius and ulna proximally, the accessory carpal bone on the palmar side, and with C4 and the 5th metacarpal bone distally
4. C4 is the largest bone of the distal row, and it articulates with the 4th and 5th metacarpal bones
B. Articulations
1. The antebrachiocarpal joint is between the distal radius and ulna and the proximal row of carpal bones. It provides about 70% of the range of motion
2. The middle carpal joint is between the proximal and distal row of carpal bones, and it provides about 25% of the range of motion
3. The carpometacarpal joint is between the distal row of carpal bones and the metacarpal bones, and it provides only about 5% of the range of motion
4. The intercarpal joints are those between the carpal bones. There is little motion in these joints
C. Ligamentous structures
1. There is no continuous collateral ligament that spans all three joints
2. The radial collateral ligament spans from the styloid process of the radius to the radial carpal bone
3. The ulnar collateral ligament spans from the styloid process of the ulna to the ulnar carpal bone
4. The flexor retinaculum supports the palmar part of the carpus
II. Fractures of the radial carpal bone
A. Most often occur in working dogs resulting from jumps or falls. Fractures may be chip fractures, slab fractures, or avulsion fractures rarely. Lameness is noted immediately following the injury. Bone fragments rarely reattach
B. Nondisplaced fractures can be treated with a splint for 6 to 8 weeks
C. Surgery is indicated to remove small fracture fragments. Larger fragments can be fixed using screws or Kirschner wires. A splint is used for several weeks postoperatively. Restrict exercise for 6 to 8 weeks. OA is a common sequel
III. Fractures of the accessory carpal bone
A. Uncommon except in racing greyhounds
B. These are usually avulsion fractures and need internal fixation
C. Use screws and Kirschner wires
D. Splint for 4 to 6 weeks postoperatively, and restrict exercise for 12 to 16 weeks
IV. Fractures of the ulnar carpal bone and C1, C2, C3, or C4
A. Very rare
B. Most are small chip fractures from hyperextension injury
C. Treatment is fragment removal, splinting, and exercise restriction
V. Luxations, subluxations, and hyperextension injuries of the carpus
A. Clinical signs and diagnosis
1. Most common injury of the carpus in nonworking dogs; usually the result of a fall or jumping from a height. Tears or the palmar joint capsule, ligaments, and fibrocartilage also occur with the fracture
2. Most have acute, non–weight-bearing lameness, with soft tissue swelling. Carpal hyperextension is present, so the carpal pad touches the ground when standing
B. Treatment
1. Splinting is not usually successful because there are soft tissue injuries present with little support for the carpus
2. Arthrodesis is the treatment of choice. If the antebrachiocarpal joint can be preserved, there will be little gait alteration after surgery
C. Postoperative complication
1. Soft tissue swelling is common for a few days post surgery. Monitor the tightness of the bandage and splint
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


