CHAPTER 17. Hematology
Patricia A. Schenck
ERYTHROCYTE DISORDERS
I. Anemias
A. Blood loss anemia
1. Causes include trauma, surgery, parasites (external and internal), gastric ulcers, gastrointestinal (GI) tumors, urinary tract tumors, splenic rupture, coagulation disorders
2. Treatment is administration of whole blood if packed cell volume (PCV) drops acutely below 20% in the dog or 25% in the cat
B. Hemolytic anemia
1. Congenital
a. Pyruvate kinase (PK) deficiency
(1) Autosomal recessive in basenji, beagle, West Highland white terrier, Cairn terrier, American Eskimo dog, miniature poodle, Chihuahua, pug; Abyssinian, Somali, and domestic short hair (DSH) cats
(2) Young animals
(3) Anemia, exercise intolerance, tachycardia, splenomegaly; death by 4 years of age usually
(4) Intense reticulocytosis, frequent nucleated red blood cells (RBCs)
(5) Polymerase chain reaction (PCR) genetic test available for some breeds
b. Phosphofructokinase deficiency
(1) Autosomal recessive in English springer spaniels and American cocker spaniels
(2) Increased intracellular pH increases fragility of RBCs
(3) Hypoxia, intravascular hemolysis, hemoglobinuria, bilirubinuria, persistent reticulocytosis
(4) Lethargy, hepatosplenomegaly, myopathy, fever. May live a normal lifespan
(5) PCR genetic test available
c. Hereditary stomatocytosis
(1) Autosomal recessive in Alaskan malamutes in association with chondrodysplasia
(2) Mild anemia with slight reticulocytosis
d. Feline porphyria
(1) Enzyme deficiency affects synthesis of heme
(2) Pink urine, pink-brown teeth, severe anemia, skin photosensitization
(3) RBCs lyse when exposed to sunlight
e. Hereditary nonspherocytic hemolytic anemia
(1) Autosomal dominant in poodles
(a) Resembles PK deficiency
(b) Persistent macrocytic hypochromic anemia; moderate reticulocytosis
(c) Fatal by 3 years of age
(2) Autosomal recessive in beagles
(a) Can remain undetected for years
(b) Short RBC lifespan
2. Immune-mediated hemolytic anemia (see below)
3. Infectious causes of hemolysis
a. Hemoplasmosis (hemobartonellosis)
(1) Caused by Mycoplasma haemocanis in dogs and Mycoplasma haemofelis in cats
(2) Transmitted by ticks and fleas or from queens to newborn kittens
(3) Immunosuppression or splenectomy predisposes
(4) Clinical signs are associated with anemia
(5) Epicellular organisms are found on blood smears; dogs usually have linear chains of organisms, whereas cats usually have coccoid or ring shapes. PCR tests are available for cats (Figure 17-1)
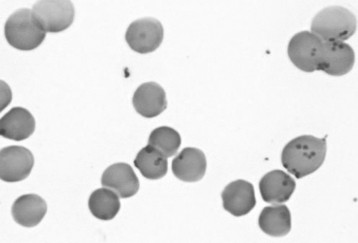 |
| Figure 17-1 This blood smear from a domestic cat shows a high proportion of the red blood cells with single scattered or short chains of basophilic cocci or faint rings on the cell membrane that are characteristic of Mycoplasma haemofelis organisms. (Diff-Quik stain, original magnification 400×.) (From Cowell RL, Tyler RD, Meinkoth JH, DeNicola DB. Diagnostic Cytology and Hematology of the Dog and Cat, 3rd ed. St. Louis, 2008, Mosby.) |
(6) Treat with doxycycline. Prednisolone may be needed to suppress the destruction of RBCs. Enrofloxacin can be used in cats if they do not tolerate doxycycline. May need blood transfusions. Cats may become latent carriers
b. Babesiosis
(1) Caused by Babesia canis or Babesia gibsoni in dogs. Babesia felis affects cats (but has not been found in North America). B. canis has been associated with greyhounds, and B. gibsoni has been associated with pitbulls and American Staffordshire terriers
(2) Transmitted by ticks
(3) Clinical signs are associated with anemia and range from an acute hemolytic crisis to subclinical signs
(4) Large teardrop-shaped organisms are seen in RBCs on blood smear. Smaller signet ring-shaped forms suggest B. gibsoni. Immunofluorescent antibody (IFA) and PCR tests are available (Figure 17-2)
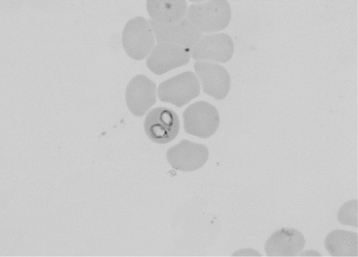 |
| Figure 17-2 Peripheral blood from a dog with a Babesia canis infection. Two piroplasms are seen in a single red blood cell in this field. (Wright’s stain, original magnification 330×.) (From Cowell RL, Tyler RD, Meinkoth JH, DeNicola DB. Diagnostic Cytology and Hematology of the Dog and Cat, 3rd ed. St. Louis, 2008, Mosby.) |
(5) Treat with imidocarb dipropionate
4. Chemical or toxic injury of erythrocytes
a. Heinz body anemia
(1) Produced by oxidant agents that precipitate hemoglobin; this leads to accelerated RBC destruction
(2) Agents responsible include acetaminophen, methylene blue, onions, zinc, vitamin K 3, methionine, and propylene glycol
(3) In cats, Heinz bodies may be associated with hyperthyroidism, lymphoma, and ketoacidosis
(4) Clinical signs include hemoglobinemia, hemoglobinuria, moderate to severe anemia, and icterus
(5) Heinz bodies appear as a large pale-staining area in RBCs or may appear as a blunt projection bulging from the RBC membrane surface. Eccentrocytosis has been associated with onion and garlic ingestion in dogs (Figure 17-3)
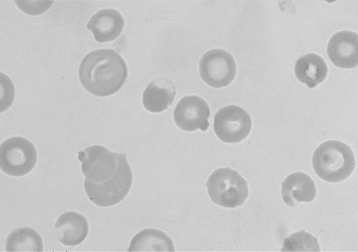 |
| Figure 17-3 Three canine erythrocytes with large Heinz bodies and an eccentrocyte (center) can be seen in this field. (Wright’s stain, original magnification 330×.) (From Cowell RL, Tyler RD, Meinkoth JH, DeNicola DB. Diagnostic Cytology and Hematology of the Dog and Cat, 3rd ed. St. Louis, 2008, Mosby.) |
(6) Treatment is to remove the source of oxidant; give blood transfusions and supportive care. Acetominophen toxicity is treated with acetylcysteine
b. Snake venom (coral snakes, rattlesnakes) can cause hemolysis. Echinocytosis may be observed
c. Zinc toxicity can cause intravascular hemolysis in dogs. Sources of zinc include galvanized wire (from kennel cages), fishing sinkers, and pennies (since 1983). Regenerative anemia results, sometimes with Heinz bodies and spherocytosis
5. Mechanical ragmentation of erythrocytes
a. Heartworms obstruct blood flow, resulting in anemia from intravascular hemolysis. Schistocytosis, hemoglobinemia, and hemoglobinuria are noted. (See section on cardiovascular disorders)
b. Disseminated intravascular coagulopathy (DIC) causes a microangiopathic hemolytic anemia from fibrin deposition in damaged small blood vessels. Thrombocytopenia, decreased clotting factors, and increased fibrin degradation products are noted
c. Hypophosphatemia associated with feline diabetes mellitus and hepatic lipidosis may cause hemolysis
C. Nonregenerative anemia
1. Infectious agents
a. Feline leukemia virus (FeLV) causes a normochromic, normocytic to macrocytic anemia. Severe RBC hypoplasia is common
b. Other viruses, such as feline infectious peritonitis (FIP), feline immunodeficiency virus (FIV), feline panleukopenia virus, canine parvovirus, and canine distemper virus, can cause mild to moderate anemia because of the suppression of erythropoiesis
d. Leishmaniasis may cause a mild to moderate normocytic, normochromic anemia
e. Cytauxzoonosis causes moderate anemia, leukopenia, and thrombocytopenia, and is highly fatal
2. Nutritional deficiencies
a. Iron deficiency causes a poorly regenerative anemia from deficient hemoglobin synthesis
(1) Caused by neoplasia, trauma, parasites, coagulopathies, and GI diseases causing blood loss
(2) RBCs show hypochromasia and poikilocytosis
(3) Thrombocytosis is common
b. Cobalamin (vitamin B 12) deficiency causes normocytic, normochromic, nonregenerative anemia
c. Folate deficiency produces a macrocytic anemia
3. Inflammatory diseases frequently cause nonregenerative anemia
a. Cytokine release leads to decreased erythropoiesis, reduced iron availability, and decreased RBC survival
b. Bone marrow is hypocellular
4. Organic diseases
a. Chronic renal disease may be accompanied by normocytic, normochromic, nonregenerative anemia
b. Liver disease is associated with normocytic, nonregenerative anemia. Poikilocytosis is common
5. Endocrine diseases
a. Hypothyroidism may cause mild anemia
b. Hyperestrogenism causes moderate to severe anemia with thrombocytopenia and leukopenia
c. Hypoadrenocorticism may cause a nonregenerative anemia
6. Drug and toxin-induced diseases
a. Drugs inducing anemia include estrogens, phenylbutazone, antineoplastic agents, trimethoprim-sulfadiazine, thiacetarsamide, quinidine, meclofenamic acid; decreased erythropoiesis and aplastic anemia
b. Lead toxicity
(1) Mild anemia; basophilic stippling observed
(2) Large numbers of nucleated RBCs with normal or decreased PCV
7. Myelophthisis occurs when abnormal cellular infiltrates crowd the bone marrow, suppressing hematopoiesis
a. Neoplasia from primary hemolymphatic tumors or metastatic tumors
b. Myelofibrosis occurs when bone marrow is damaged by inflammation, necrosis, neoplasia, toxic agents. It is also associated with myelodysplastic syndrome and acute myelogenous leukemia in cats. Bone marrow aspirate produces only blood, with few to no marrow particles
c. Myelonecrosis results from direct injury to endothelium or occlusion of microcirculation
d. Osteopetrosis is an inherited condition resulting in obliteration of marrow cavities by bone, with resulting anemia or pancytopenia in young dogs
8. Irradiation can result in pancytopenia and aplastic bone marrow
9. Pure erythrocyte aplasia is a significant reduction in erythroid stem cells, with no effect on granulocytic or megakaryocytic lines
II. Polycythemia
A. Relative polycythemia
1. Usually due to dehydration or hemoconcentration. Splenic contraction from excitement can also cause a transient increase in PCV. Greyhounds normally have a higher PCV (about 60%)
2. Mucous membranes are dark red and have a slow capillary refill time
B. Absolute polycythemia
1. Primary erythrocytosis (polycythemia vera) results from a stem cell defect, with low serum erythropoietin concentrations
2. Secondary erythrocytosis is a result of overproduction of erythropoietin resulting from hypoxia, erythropoietin-producing tumors, or pyelonephritis
III. Methemoglobinemia
A. Occurs from oxidation of iron in hemoglobin. Oxidized hemoglobin cannot bind oxygen, resulting in hypoxia. Blood appears dark red or chocolate-colored
B. Results from exposure to oxidant drugs and chemicals. Methemoglobinemia often occurs at the same time as Heinz bodies appear, but methemoglobinemia usually occurs first
C. Treatment is similar to Heinz body anemia
LEUKOCYTE DISORDERS
I. Congenital disorders
A. Pelger-Huet anomaly
1. Inherited disorder of granulocyte maturation
2. Nuclei of neutrophils often look like band cells, metamyelocytes, or myelocytes
3. No clinical signs; treatment not necessary
B. Feline Chediak-Higashi syndrome
1. Rare; occurs in blue-smoke Persian cats with yellow eyes
2. Neutrophils contain large pink cytoplasmic inclusions
3. Abnormal lysosomal granule formation in granulocytes and monocytes
C. Lysosomal storage disease
1. Mucopolysaccharidosis and gangliosidosis
a. Inherited; caused by enzyme deficiency
b. Neutrophils contain coarse, red-purple granules when stained. Must distinguish these from toxic neutrophils
2. Other disorders cause lymphocyte vacuolation abnormalities. Affected lymphocytes have multiple cytoplasmic vacuoles
D. Abnormal granulation syndrome in Birman cats
1. Pink-purple granules within neutrophil cytoplasm
2. No clinical signs
II. Neutrophil disorders
A. Neutrophilia
1. Physiologic resulting from the release of epinephrine (transient increase). More common in cats
2. Corticosteroid administration
3. Inflammation
a. Infectious
b. Noninfectious such as in pancreatitis, tissue necrosis, thrombosis, and burns
c. Neoplasia such as metastatic fibrosarcoma or renal tubular carcinoma
d. Severe abscessation such as pyometra
e. Immune-mediated such as systemic lupus erythematosus
f. Granulocytopathy syndrome in Irish setters. Neutrophils have impaired bactericidal activity as a result of adhesion defects
4. Paraneoplastic syndrome
B. Neutropenia
1. Congenital cyclic neutropenia
a. Inherited disorder of gray collies
b. Cyclic decrease of neutrophils, platelets, and monocytes in 12-day intervals
2. Infection causes a degenerative left shift with an increase of immature cells
a. Gram-negative bacteria
b. Toxoplasma
c. Systemic fungal disease
d. Viruses such as FeLV, FIV, feline panleukopenia virus, canine parvovirus
e. E. canis
3. Drugs: Many antibiotics (e.g., chloramphenicol, trimethoprim-sulfadiazine), antineoplastic agents, and nonsteroidal antiinflammatory drugs (NSAIDs) can cause neutropenia
4. Endotoxins from gram-negative bacteria
5. Immune-mediated neutropenia is due to destruction of antibody-coated neutrophils by macrophages. Drugs responsible include methimazole and cephalosporins
III. Monocytosis
A. From corticosteroid administration (along with neutrophilia, lymphopenia, and eosinopenia)
B. Inflammatory processes that cause a demand for macrophages
C. Neoplasia (see leukemic disorders below)
IV. Eosinophils
A. Eosinophilia
1. Parasites in skin, respiratory tract, or GI tract
2. Parasites include Ancylostoma, Trichuris vulpis, Toxocara canis, Dirofilaria immitis, Dipetalonema reconditum, lungworms, and Paragonimus kellicotti
3. Allergies result in the production of immunoglobulin E (IgE) with mast cell degranulation and attraction of eosinophils
4. Tumors such as fibrosarcoma, mammary carcinoma, mast cell tumors, and T-cell lymphomas (cats)
5. Feline hypereosinophilic syndrome
a. Infiltration of eosinophils into organs
b. Cause unknown
c. Resembles leukemia of well-differentiated eosinophils
d. Clinical signs include anorexia, weight loss, fever, vomiting, diarrhea, and lymphadenopathy
e. Death results from organ infiltration
B. Eosinopenia from exogenous or endogenous corticosteroids
V. Basophilia
A. Parasites such as heartworms or hookworms
B. Allergies cause IgE production with increased mast cells and basophils
C. Hyperlipemia can result in basophilia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


