CHAPTER 12. Cardiovascular Disorders
Ashley B. Saunders
CARDIOVASCULAR PHYSIOLOGY DEFINITIONS
I. Afterload: The force or tension on the ventricular myocardium during contraction
II. Preload: The volume of blood present in the ventricle at the end of diastole
III. Chronotropy: Heart rate
A. Positive chronotropy designates an increase in heart rate
B. Negative chronotropy designates a decrease in heart rate
IV. Inotropy: Myocardial contractility
A. Positive inotropy designates an increase in contractility
B. Negative inotropy designates a decrease in contractility
V. Systole: Contraction of the heart chambers
VI. Diastole: Period of relaxation of the heart chambers
VII. Cardiac output: The combination of stroke volume and heart rate
VIII. Systemic vascular resistance: Resistance to blood flow through the systemic arterioles
IX. Blood pressure: The combination of cardiac output and systemic vascular resistance
X. Eccentric hypertrophy: Dilated atrial or ventricular chambers with normal to decreased wall thickness caused by a volume overload. Examples of heart diseases that result in eccentric hypertrophy include the following:
A. Dilated cardiomyopathy
B. Valvular endocardiosis
C. Patent ductus arteriosus (PDA)
D. Ventricular septal defect
E. Atrial septal defect (ASD)
XI. Concentric hypertrophy: Ventricular wall thickening caused by a pressure overload. Examples of heart diseases that result in concentric hypertrophy include the following:
A. Systemic hypertension
B. Pulmonary hypertension
C. Pulmonic stenosis
D. Aortic stenosis
XII. Heart failure: Occurs when the hearts ability to supply adequate blood flow is reduced
A. Congestive: Occurs when reduced cardiac function results in elevated venous pressures and fluid accumulates in organs or body cavities
B. Backward: Congestive
C. Forward: Reduced cardiac output
D. Left-sided: Results in pulmonary edema
E. Right-sided: Results in hepatomegaly, ascites, pleural effusion, pericardial effusion
F. Neuroendocrine consequences of heart failure
1. Activation of the renin angiotensin aldosterone system (RAAS): A decrease in cardiac output is detected by the kidneys. Renin is released and converts angiotensinogen to angiotensin I in the liver. Angiotensin I is converted to angiotensin II in the lungs. Angiotensin II stimulates constriction of vascular smooth muscle, and increased blood volume. Angiotensin II stimulates aldosterone, which leads to increased sodium chloride retention, and increased blood volume
2. Activation of the sympathetic nervous system. Norepinephrine levels increase in response to a decrease in cardiac output and results in tachycardia and vasoconstriction
DIAGNOSTIC TESTS
I. Echocardiography: Ultrasound of the heart used to evaluate structure and function
II. Electrocardiography: Records the electrical activity of the heart for analysis of heart rate and rhythm, conduction abnormalities, and chamber enlargement patterns
III. Holter monitor: Records an electrocardiogram (ECG) over an extended period
IV. Thoracic radiographs: Used to evaluate heart size and shape, to assess pulmonary and mediastinal structures, and to evaluate for congestive heart failure (CHF)
V. Blood pressure: Systolic; mean and diastolic systemic arterial pressure can be measured invasively (direct) or noninvasively (indirect)
VI. Cardiac catheterization and angiography: Catheters placed into peripheral vessels are used to evaluate hemodynamics and to perform contrast studies of the heart and vessels
VII. Nuclear cardiology: First-pass nuclear angiocardiography studies assess the direction and magnitude of shunts, and gated radionuclide studies evaluate ventricular function
CONGENITAL HEART DISEASE
I. The most common congenital heart diseases in dogs are PDA, subaortic stenosis, and pulmonic stenosis
II. The most common congenital heart diseases in cats are septal defects (ASD, ventricular septal defect, endocardial cushion defect) and atrioventricular valvular dysplasia
III. Most common defects resulting in cyanosis
A. Tetralogy of Fallot
B. Right-to-left shunting PDA. Creates differential cyanosis, cyanosis of the caudal mucous membranes
C. Right-to-left shunting ventricular septal defect
IV. Aortic stenosis
A. Most often occurs as a result of a ridge or ring of tissue below the aortic valve (subvalvular)
B. Severity can increase until a dog reaches mature body weight
C. Heritable
D. Common breeds: Newfoundland, golden retriever, Rottweiler, German shepherd, boxer, bull terrier
E. Clinical signs: May be normal; exercise intolerance, lethargy, syncope, cough, dyspnea, sudden death
F. Physical examination (Table 12-1)
| Defect | Murmur Location | Murmur Timing | Pulse Quality |
|---|---|---|---|
| Patent ductus arteriosus | Left base | Continuous | Bounding |
| Pulmonic stenosis | Left base | Systolic | Normal |
| Subaortic stenosis | Left base | Systolic | Normal to decreased |
1. Systolic left basilar murmur
2. Diastolic left basilar murmur
3. Normal to weak pulse quality
4. Dyspnea
G. Diagnosis
1. Echocardiogram
a. Left ventricular hypertrophy
b. Left atrial enlargement
c. Subvalvular narrowing
d. Poststenotic dilation of aorta
e. Thickened aortic valve leaflets
f. Aortic regurgitation
g. Elevated transaortic velocities
2. Electrocardiography
a. Tall R waves in lead II suggestive of left ventricular enlargement
b. Wide P wave in lead II suggestive of left atrial enlargement
c. ST segment depression
d. Ventricular arrhythmias
3. Thoracic radiographs (Figure 12-1)
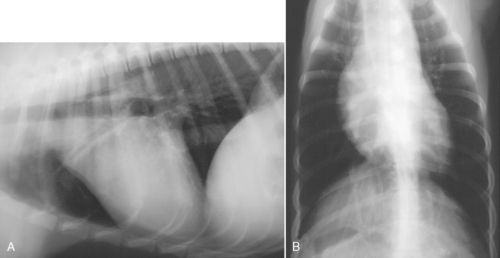 |
| Figure 12-1 Lateral (A) and dorsoventral (B) radiographs from a young dog with subaortic stenosis. Prominent bulge in the cranial waist on the lateral view and widening of the cranial mediastinum on the dorsoventral view are consistent with poststenotic dilatation of the ascending aorta. (From Ettinger, SJ, Feldman, EC. Textbook of Veterinary Internal Medicine, 2-Vol Set, 6th ed. Philadelphia, 2004, Saunders.) |
a. Normal in dogs with mild disease
b. Left ventricular enlargement
c. Left atrial enlargement
d. Poststenotic dilation of aorta
H. Treatment
1. Balloon valvuloplasty
a. Variable success rate
b. No additional benefit compared with β-blocker therapy alone
2. Surgery
a. Resection of subvalvular lesion and replacement with patch graft
b. High degree of difficulty
c. Requires special equipment
d. Costly
e. Not readily available
3. Medical management
a. β-Blocker therapy
b. Antibiotic therapy to prevent valvular endocarditis during periods of bacteremia
c. CHF
(1) Oxygen
(2) Diuretics
(3) Nitroglycerin ointment
(4) Angiotensin-converting enzyme (ACE) inhibitor
I. Prognosis
1. Mild: Favorable; rarely develop clinical signs
2. Moderate: Favorable; may develop clinical signs
3. Severe: Develop clinical signs, shortened life span, risk of sudden death
V. ASD
A. Occurs in dogs and cats
B. Typically shunts left to right
C. Common breeds: Boxer, standard poodle
D. Clinical signs: May be normal; exercise intolerance, lethargy, syncope, right heart-sided heart failure with large defects, ascites
E. Physical examination
1. Systolic left basilar murmur
2. Split second heart sound
3. Normal pulse quality
4. Right-sided heart failure with large defects: Ascites, jugular venous distension, positive hepatojugular reflex
F. Diagnosis
1. Echocardiogram
a. Right ventricular enlargement
b. Right atrial enlargement
c. ASD
2. Electrocardiography
a. Deep S waves in leads I, II, III, aV f are suggestive of right ventricular enlargement
b. Right axis deviation
c. Tall P waves in lead II suggestive of right atrial enlargement
3. Thoracic radiographs
a. Normal in dogs with mild disease
b. Right atrial enlargement
c. Right ventricular enlargement
d. Main pulmonary artery dilation
e. Pleural effusion
G. Treatment
1. Interventional catheterization. Device used to close large ASDs
2. Surgery
a. Patch graft
b. High degree of difficulty
c. Requires special equipment
d. Costly
e. Not readily available
3. Medical management. Congestive right heart failure
a. Oxygen
b. Diuretics
c. Positive inotropic support
d. ACE inhibitor
e. Pleurocentesis
f. Abdominocentesis
H. Prognosis
1. Small defects: Favorable; rarely develop clinical signs
2. Moderate to large defects: Develop clinical signs, shortened life span without defect closure
VI. PDA
A. Common congenital heart defect in dogs
B. More common in females
C. Heritable
D. Results from a congenital lack of ductal smooth muscle
E. Typically left to right shunting
F. Common breeds: Miniature poodle, Maltese, German shepherd, Yorkshire terrier, Shetland sheepdog, collie, Pomeranian, Labrador retriever, bichon frise
G. Clinical signs: May be normal; exercise intolerance, lethargy, cough, dyspnea
H. Physical examination
1. Continuous left basilar murmur
2. Systolic left apical murmur of mitral regurgitation
3. Increased (hyperkinetic) pulse quality results from a large difference in systolic and diastolic pulse pressure
4. Dyspnea
I. Diagnosis
1. Echocardiogram
a. Left ventricular enlargement
b. Left atrial enlargement
c. Continuous color flow within the main pulmonary artery
d. Visualization of the PDA. Typically funnel shaped with narrowing at the pulmonary artery side
e. Mitral regurgitation
2. Electrocardiography
a. Tall R waves in lead II suggestive of left ventricular enlargement
b. Wide P waves in lead II suggestive of left atrial enlargement
3. Thoracic radiographs
a. Normal in dogs with mild disease
b. Left atrial enlargement
c. Left ventricular enlargement
d. Aneurysmal bulge of descending aorta
e. Pulmonary overcirculation
f. Pulmonary edema
4. Blood pressure
a. Normal systolic
b. Decreased diastolic
J. Treatment
1. Interventional catheterization: Device implantation (coil, vascular plug, ductal occluder)
2. Surgery. Ligation
3. Medical management
a. CHF
(1) Oxygen
(2) Diuretics
(3) Positive inotropic support
(4) Nitroglycerin ointment
(5) ACE inhibitor
K. Prognosis
1. Small PDA: Favorable, might not develop clinical signs
2. Moderate to large PDA: Develop clinical signs, favorable with ductal occlusion-ligation; shortened life span without treatment
L. Right-to-left shunting PDA
1. Attributed to increased pulmonary vascular resistance
2. Patients develop hypoxemia, exercise intolerance, collapse, tachypnea, dyspnea, ascites
3. Polycythemia results from hypoxemia and is managed with phlebotomy or hydroxyurea
4. PDA closure is contraindicated and will result in severe hypoxemia and death
5. Prognosis is poor
VII. Pulmonic stenosis
A. Valvular pulmonic stenosis is a common congenital heart disease in dogs
B. Severity can increase until a dog reaches mature body weight
C. Occasionally, an aberrant left coronary artery encircles the right ventricular outflow tract and pulmonic valve causing pulmonic stenosis. Occurs most often in the English bulldog and boxer
D. Heritable
E. Common breeds: English bulldog, West Highland white terrier, boxer, Chihuahua, mastiff, beagle
F. Clinical signs: May be normal; exercise intolerance, lethargy, syncope, ascites, sudden death
G. Physical examination
1. Systolic left basilar murmur
2. Diastolic left basilar murmur with significant pulmonic valvular regurgitation
3. Normal pulse quality
4. Ascites
5. Jugular venous distension
6. Positive hepatojugular reflex
H. Diagnosis
1. Echocardiogram
a. Right ventricular hypertrophy
b. Interventricular septal flattening
c. Right atrial enlargement
e. Thickened pulmonic valve leaflets
f. Restricted motion of pulmonic valve leaflets
g. Pulmonic regurgitation
h. Elevated peak transpulmonic velocities
i. Hypoplastic pulmonic valve annulus
j. Aberrant coronary artery
2. Electrocardiography
a. Deep S waves in leads I, II, III, aV f suggestive of right ventricular enlargement
b. Right axis deviation
c. Tall P waves in lead II suggestive of right atrial enlargement
3. Thoracic radiographs (Figure 12-2)
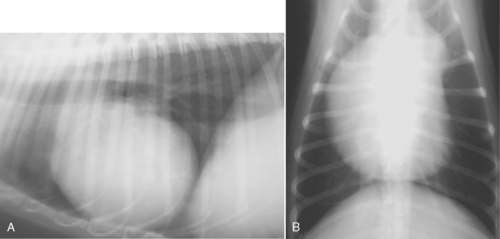 |
| Figure 12-2 Lateral (A) and dorsoventral (B) thoracic radiographs from a dog with pulmonic stenosis. Rounding of the sternal border and a bulge in the cranial waist of the heart can be seen in the lateral view. Right heart enlargement and a bulge in the main pulmonary artery segment are seen in the dorsoventral view. Pulmonary vessels are diminished even in the absence of a right-to-left shunt. (From Ettinger SJ, Feldman EC. Textbook of Veterinary Internal Medicine: 2-Vol Set, 6th ed. Philadelphia, 2004, Saunders.) |
a. Normal in dogs with mild disease
b. Right ventricular enlargement
c. Right atrial enlargement
d. Poststenotic dilation of main pulmonary artery
e. Enlarged caudal vena cava
I. Treatment
1. Balloon valvuloplasty
a. For valvular pulmonic stenosis
b. Prognosis improved if pressure gradient is reduced to mild
2. Surgery
a. Resection of stenotic area and replacement with a patch graft
b. Conduit around stenosis, especially if aberrant coronary artery
c. High degree of difficulty
d. Requires special equipment
e. Costly
f. Not readily available
3. Medical management
a. β-Blocker therapy
b. Congestive right-sided heart failure
(1) Oxygen
(2) Diuretics
(3) ACE inhibitor
(4) Pleurocentesis
(5) Abdominocentesis
J. Prognosis
1. Mild: Favorable; rarely develop clinical signs
2. Moderate: Favorable; may develop clinical signs
3. Severe: Develop clinical signs; shortened life span, risk of sudden death
VIII. Tetralogy of Fallot
A. Characterized by a ventricular septal defect, pulmonic stenosis, overriding aorta and right ventricular hypertrophy
B. Pulmonic stenosis creates an obstruction to blood flow into the pulmonary artery. Deoxygenated blood is delivered to the systemic circulation, resulting in hypoxemia
C. Most common cyanotic congenital heart defect in dogs
D. May result in polycythemia
E. Inherited as a simple autosomal recessive trait
F. Common breeds: Keeshond, English bulldog
G. Clinical signs: May be normal; exercise intolerance, lethargy, syncope, seizures resulting from polycythemia, dyspnea resulting from hypoxemia, ascites
H. Physical examination
1. Cyanosis with and without exercise
2. Systolic left or right basilar murmur of pulmonic stenosis
3. Might not have an audible murmur
4. Normal pulse quality
5. Ascites
6. Jugular venous distension
7. Positive hepatojugular reflex
8. Dyspnea
I. Diagnosis
1. Echocardiogram
a. Right ventricular hypertrophy
b. Interventricular septal flattening
c. Right atrial enlargement
d. Overriding aorta
e. Ventricular septal defect
f. Color flow from right ventricle into aorta
g. Poststenotic dilation of main pulmonary artery
h. Thickened pulmonic valve leaflets
i. Restricted motion of pulmonic valve leaflets
j. Pulmonic regurgitation
k. Elevated peak transpulmonic velocities
2. Electrocardiography
a. Deep S waves in leads I, II, III, aV f suggestive of right ventricular enlargement
b. Right axis deviation
c. Tall P waves in lead II suggestive of right atrial enlargement
3. Thoracic radiographs
a. Right ventricular enlargement
b. Decreased pulmonary vasculature
c. Poststenotic dilation of main pulmonary artery
4. Packed cell volume (PCV): To monitor polycythemia
5. Arterial blood gas: To monitor hypoxemia
J. Treatment
1. Balloon valvuloplasty: For severe or symptomatic valvular pulmonic stenosis
2. Surgery
a. Resection of the pulmonic stenosis and replacement with a patch graft
b. Patch graft of the ventricular septal defect
c. Blalock Taussig shunt: Connects the left subclavian artery to the pulmonary artery to create a communication between the pulmonary and systemic circulation
d. High degree of difficulty
e. Requires special equipment
f. Costly
g. Not readily available
3. Medical management
a. Phlebotomy. PCV should be maintained below 60% to 65%
b. Hydroxyurea. Side effects related to myelosuppression
c. β-Blockers to relieve hypoxemic episodes associated with sympathetic drive
d. CHF
(1) Oxygen
(2) Diuretics
(3) ACE inhibitor
(4) Pleurocentesis
(5) Abdominocentesis
K. Prognosis
1. Mild: Favorable; rarely develop clinical signs
2. Moderate: May develop clinical signs
3. Severe: Develop clinical signs; shortened life span, risk of sudden death
IX. Atrioventricular valvular dysplasia
A. Mitral and tricuspid valve dysplasia
2. Occurs in both dogs and cats
B. Common breeds
1. Tricuspid valve dysplasia: Great Dane, German shepherd, golden retriever, Labrador retriever, Weimaraner
2. Mitral valve dysplasia: Great Dane, German shepherd, golden retriever, bull terriers, numerous cat breeds
C. Clinical signs
1. Tricuspid valve dysplasia
a. May be normal
b. Exercise intolerance
c. Lethargy
d. Syncope
e. Right-sided heart failure, ascites
f. Sudden death
2. Mitral valve dysplasia
a. May be normal
b. Exercise intolerance
c. Lethargy
d. Syncope
e. Left-sided heart failure
(1) Cough
(2) Dyspnea
f. Sudden death
D. Physical examination
1. Tricuspid valve dysplasia
a. Systolic right-sided heart murmur
b. Normal pulse quality
c. Ascites
d. Jugular venous distension
e. Positive hepatojugular reflex
f. Arrhythmias
2. Mitral valve dysplasia
a. Systolic left apical murmur
b. Normal pulse quality
c. Dyspnea
d. Arrhythmias
E. Diagnosis
1. Tricuspid valve dysplasia
a. Echocardiogram
(1) Right atrial enlargement
(2) Right ventricular enlargement
(3) Tricuspid valve displaced toward the right ventricle
(4) Tricuspid valve apparatus
(a) Thickened valve leaflets
(b) Short septal leaflet with restricted motion
(c) Elongated mural leaflet
(d) Atrophy, hypertrophy, or malpositioned papillary muscles
(e) Thickened, short, or elongated chordae tendinae
(5) Tricuspid regurgitation
b. Electrocardiography
(1) Splintered QRS complex
(2) Deep S waves in leads I, II, III, aV f suggestive of right ventricular enlargement
(3) Right axis deviation
(4) Tall P waves in lead II suggestive of right atrial enlargement
(5) Supraventricular premature beats
(6) Atrial fibrillation
c. Thoracic radiographs
(1) Normal with mild disease
(2) Right atrial enlargement
(3) Right ventricular enlargement
(4) Caudal vena cava enlargement
(5) Pleural effusion
2. Mitral valve dysplasia
a. Echocardiogram
(1) Left atrial enlargement
(2) Left ventricular enlargement
(3) Mitral valve apparatus
(a) Thickened valve leaflets
(b) Short or elongated valve leaflets with restricted motion
(c) Atrophy, hypertrophy, or malpositioned papillary muscles
(d) Thickened, short, or elongated chordae tendinae
(4) Mitral regurgitation
b. Electrocardiography
(1) Tall R waves in lead II suggestive of left ventricular enlargement
(2) Wide P waves in lead II suggestive of left atrial enlargement
(3) Supraventricular premature beats
(4) Atrial fibrillation
c. Thoracic radiographs
(1) Normal with mild disease
(2) Left atrial enlargement
(3) Left ventricular enlargement
(4) Pulmonary venous enlargement
(5) Pulmonary edema
F. Treatment
1. Balloon valvuloplasty. Tricuspid valve stenosis
2. Surgery
a. Valvular repair or replacement
b. High degree of difficulty
c. Requires special equipment
d. Costly
e. Not readily available
3. Medical management
a. CHF
(1) Oxygen
(2) Diuretics
(3) Positive inotropic support
(4) Nitroglycerin ointment
(5) ACE inhibitor
(6) Pleurocentesis
(7) Abdominocentesis
b. Antiarrhythmic therapy
G. Prognosis
1. Mild: Favorable; rarely develop clinical signs
2. Moderate: Favorable; may develop clinical signs
3. Severe: Develop clinical signs, shortened life span, risk of sudden death
X. Ventricular septal defect
A. Perimembranous defects occur most often in dogs
C. Typically shunt left to right
D. Common breeds: English springer spaniel, English bulldog
E. Clinical signs: May be normal; exercise intolerance, lethargy, cough, dyspnea
F. Physical examination
1. Systolic right sternal or left basilar murmur. Loud murmurs are associated with small ventricular septal defects
2. Diastolic left basilar murmur associated with aortic regurgitation if aortic valve leaflet prolapses into USD
3. Normal pulse quality
G. Diagnosis
1. Echocardiogram
a. Left ventricular enlargement
b. Left atrial enlargement
c. Ventricular septal defect
d. Aortic insufficiency
2. Electrocardiography
a. Tall R waves in lead II suggestive of left ventricular enlargement
b. Wide P waves in lead II suggestive of left atrial enlargement
3. Thoracic radiographs
a. Normal in dogs with small septal defects
b. Left atrial enlargement
c. Left ventricular enlargement
d. Pulmonary overcirculation
e. Pulmonary edema
H. Treatment
1. Interventional catheterization: Device used to close large ventricular septal defects
2. Surgery
a. Pulmonary artery banding
b. Patch graft
(1) High degree of difficulty
(2) Requires special equipment
(3) Costly
(4) Not readily available
3. Medical management. Congestive left-sided heart failure
a. Oxygen
b. Diuretics
c. Positive inotropic support
d. Nitroglycerin ointment
e. ACE inhibitor
I. Prognosis
1. Small defects: Favorable; rarely develop clinical signs
2. Moderate to large defects: Develop clinical signs; shortened life span without defect closure
XI. Vascular ring anomaly. Persistent right fourth aortic arch
A. The esophagus is surrounded by the pulmonary artery, ligamentum arteriosum, right aortic arch, heart base, and trachea
B. Common breeds: German shepherd, Irish setter, Great Dane
C. Clinical signs of regurgitation are attributed to esophageal obstruction
D. Diagnosed with thoracic radiographs, angiography, or esophageal endoscopy
E. Treatment requires surgical ligation of the ligamentum arteriosum
F. Prognosis is good to guarded. Residual esophageal functional and structural damage may persist
ACQUIRED HEART DISEASE
I. Myocardial disease
A. Dogs
1. Dilated cardiomyopathy
2. Arrhythmogenic right ventricular cardiomyopathy
3. Hypertrophic cardiomyopathy
B. Cats
1. Hypertrophic cardiomyopathy
2. Dilated cardiomyopathy
3. Restrictive cardiomyopathy
4. Arrhythmogenic right ventricular cardiomyopathy
C. Dilated cardiomyopathy in dogs
1. Heritable in some breeds (boxer, Doberman pinscher, Great Dane, Newfoundland)
2. More common in male dogs
3. Preclinical: Denoted by the presence of left ventricular dilation, left ventricular systolic dysfunction, and ventricular arrhythmias in the absence of clinical signs
4. Clinical: Left ventricular dilation, left ventricular systolic dysfunction, and ventricular arrhythmias in the presence of clinical signs
5. Common breeds: Doberman pinscher, Newfoundland, Irish wolfhound, Great Dane, Labrador retriever, cocker spaniel, boxer, Saint Bernard, Old English sheepdog, Dalmatian
6. Causes
a. Tachycardia induced
(1) Myocardial dysfunction resulting from a persistently fast heart rate (>200 beats/min)
(2) Enlargement of all four heart chambers
(3) May resolve with appropriate heart rate control
b. Toxic. Adriamycin (doxorubicin)
(1) Patients present with arrhythmias and myocardial failure
(2) Dose dependent and reversible
(3) Cardiotoxicity occurs at cumulative doses of 250 mg/m 2
c. Infectious myocarditis
(1) Toxoplasma gondii
(2) Trypanosoma cruzi
(a) (Vector is the reduvid bug)
(b) Forms
i. Trypomastigote in blood
ii. Amastigote in host tissue
(c) Presentation
i. Ventricular arrhythmias and atrioventricular block
ii. Systolic dysfunction of primarily the right ventricle
iii. Heart failure
(d) No reliable cure
(e) Treat symptomatically
(3) Parvovirus
(a) Affected puppies during the 1970s and 1980s
(b) Not routinely encountered now that most dogs are appropriately vaccinated
(4) Distemper virus: Uncommon given that most dogs are appropriately vaccinated
d. Endocrine
(1) Hypothyroidism
(a) May contribute
e. Nutritional
(1) Taurine deficiency
(a) Cocker spaniels
(b) Golden retrievers
(2) Carnitine deficiency
(a) Cocker spaniels
(b) Boxers
f. Idiopathic. No identifiable cause
7. Clinical signs
a. May be normal
b. Exercise intolerance
c. Lethargy
d. Left- and right-sided heart failure
(1) Cough
(2) Dyspnea
(3) Ascites
(4) Syncope
(5) Sudden death
(6) Anorexia
(7) Weight loss
8. Physical examination
a. Systolic left or right heart murmur associated with atrioventricular valvular regurgitation
b. Gallop
c. Arrhythmia
d. Normal to decreased pulse quality
e. Pulse deficits
f. Normal to pale mucous membrane color
g. Dyspnea
h. Ascites
i. Hepatosplenomegaly
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


