CHAPTER 11. Routine Management of the Neonatal Foal
OBJECTIVES
While studying the information covered in this chapter, the reader should attempt to:
■ Acquire a working understanding of procedures for evaluation of the newborn foal.
■ Acquire a working understanding of the need for colostrum acquisition by the newborn foal, techniques for administration of colostrum to foals, and techniques for testing for failure of passive antibody transfer to foals.
■ Acquire a working understanding of techniques for caring for the umbilical cord of the foal at the time of parturition and for preventing meconial impaction.
STUDY QUESTIONS
1. Describe the procedure for performing a physical examination of a newborn foal and include expected normal findings.
2. Describe the procedures for testing foals for passive antibody transfer failure and methods for administration of colostrum to foals to avoid this condition.
3. Describe the procedures used for treatment of passive antibody transfer failure in foals.
4. Describe the techniques involved in caring for the umbilical cord of the newborn foal.
5. Describe the clinical signs of meconium impaction in foals, methods used to differentiate meconium impaction from other causes of colic or straining in newborn foals, and methods for administration of enemas to prevent this condition.
The neonatal period is a vulnerable segment of foal development. The transition from a protected, intrauterine existence to a state of relative independence is subject to a myriad of interferences. The vast array of potential inherent defects and environmental assaults can be devastating to the viability of the newborn foal and in turn can lead to significant losses for the horse industry. Equine practitioners should be well versed in all aspects of neonatal care to properly assist broodmare owners in managing newborn foals.
The managerial recommendations described herein are arranged in a chronologic sequence that can be applied to care of foals on a large broodmare farm. The order of events often is altered, especially on smaller farms where a veterinarian is not present during parturition to evaluate foals in the first few hours of life.
The chronologic span of the neonatal period is not defined uniformly; descriptions vary by as much as several weeks. The most critical part of neonatal development occurs within the first 4 days of life, when the newborn foal attempts to establish somatovisceral homeostasis. This chapter discusses general management guidelines for the immediate postnatal period. Application of basic management principles during the immediate neonatal period can prevent many problems that may result from birthing or environmental insults.
EVALUATION OF RESPIRATORY AND CARDIAC FUNCTION
Airway clearance and the establishment of a normal respiratory-cardiac rhythm are crucial. When the amnion envelops the mouth and the nostrils at birth, it should be removed to prevent asphyxiation (see Figures 9-13 and 9-14). Excessive fluid in the nasal cavity can be partially removed by stripping the nostrils with the fingers and thumb. If necessary, gentle suction also can be applied.
Fetal passage through the birth canal promotes thoracic compression and resultant expulsion of fluid from the upper airway. If a cesarean section is performed, the newborn is apt to need additional assistance to remove these contents effectively. The foal can be placed in a lateral recumbent position in a well-bedded location with the forequarters in a lower plane than the hindquarters to facilitate dependent drainage of fluid. Some practitioners hold the foal up by the hind legs for a short period of time to promote better fluid evacuation; this procedure should be brief because abdominal viscera compress the diaphragm, limiting the ability of the foal to expand its lungs. The foal is dried with a towel or blanket and rubbed briskly to stimulate respiratory activity (Figure 11-1). The rate and intensity of the heart beat and peripheral pulse should be evaluated (refer to “Physical Examination” in this chapter).
VIABILITY ASSESSMENT AND RESUSCITATION PROCEDURE
The practitioner should look for signs indicative of a strong, vigorous animal. Weak or immature foals are more vulnerable to stressful influences of the extrauterine environment and thus need more intensive care to maximize their chances for survival. Fetal stress should be suspected when meconial staining of the amniotic fluid, fetal membranes, or foal is observed, which increases the risk of aspirated meconium, predisposing the animal to hypoxia and pneumonia.
The degree of neonatal stress and birth asphyxia can be evaluated in the newborn foal with a modification of the Apgar scoring system used in human neonatology (Table 11-1). The observations listed for the modified Apgar scoring system should be made 1 and 5 minutes after delivery. In infants, the 1-minute score correlates directly with umbilical cord blood pH and is an index of intrauterine asphyxia. The 5-minute Apgar score correlates more with the infant’s eventual neurologic outcome.
| *A value of 0, 1, or 2 is assigned for each of the four observations. Total score: 7 to 8, normal; 4 to 6, mild to moderate asphyxia; 0 to 3, severe asphyxia. | |||
| From Martens RJ: Pediatrics. In Mansmann RA, McAllister ES, Pratt PW, editors: Equine medicine and surgery, ed 3, vol 1, Santa Barbara, CA, 1982, American Veterinary Publications. | |||
| Observation | Assigned Values* | ||
|---|---|---|---|
| 0 | 1 | 2 | |
| Heart and pulse rate | Undetectable | <60 beats/min | >60 beats/min |
| Respiration (rate and pattern) | Undetectable | Slow, irregular | 60 breaths/min, regular |
| Muscle tone | Lateral recumbency, limp | Lateral recumbency, evidence of some muscle tone | Able to maintain sternal recumbency |
| Nasal stimulation (with straw) | Unresponsive | Grimace with mild rejection | Cough or sneeze |
Although the Apgar score has had limited use in equine neonatology, the criteria presented here provide a rational set of guidelines for evaluation of the degree of neonatal asphyxia and for determination of whether resuscitative measures are indicated. Early signs of asphyxia include increased rate and depth of respiration followed by a period of gasping and primary apnea. With severe asphyxia, the respiratory center becomes progressively depressed and is no longer responsive to sensory and chemical stimuli. The gasping episodes become weaker, and bradycardia develops, followed by a stage of secondary apnea.
Although much normal variation in foal adaptive responses occurs in the immediate postnatal period, comparison of foal responses with published values can provide some confidence that the foal is viable. The newborn foal should establish normal respiratory and cardiac rhythm within 1 minute of birth, and righting and suckle reflexes should be apparent within 5 minutes of birth. The suck reflex can be tested by placing a clean finger in the mouth of the foal. Most healthy foals begin attempting to stand within 30 minutes of birth and are able to stand without assistance by 1 to 2 hours of age. The newborn foal should be able to locate the mare’s udder and nurse without assistance within 1 to 3 hours of birth.
Foals with signs of mild to moderate asphyxia (Apgar score 4 to 6) should be given moderate stimulation that includes brisk rubbing of the foal’s back and sides with a dry towel, postural drainage in conjunction with gentle thoracic coupage, limb manipulation, and stimulation of the inside of the nares to elicit a sneeze or a cough. The induced cough helps to move secretions out of the lower airways. The neck should be gently hyperextended and the oropharynx cleared of mucus or amniotic fluid to ensure a patent airway. Suctioning of the oropharynx and the trachea can be performed with a 10F suction catheter (Regu-Vac, Becton Dickinson, Franklin Lakes, NJ). The foal must be preoxygenated (12 L/min through a catheter) before suction is applied to avoid causing respiratory distress, cardiac arrhythmias, or cardiac arrest. Prolonged periods of suction should also be avoided because they result in decreased arterial oxygenation. Suction (vacuum set at 80 to 120 mm Hg) should be applied only during withdrawal of the catheter from the airway.
Placement of the foal in a sternal recumbent position (Figure 11-2) helps decrease dependent lung atelectasis, thus minimizing the ventilation-perfusion inequalities created by prolonged lateral recumbency. Supplemental oxygen (humidified) can be delivered via a nasal cannula or a face mask at a flow rate of 5 to 10 L/min. A nasal cannula should be passed in the ventral meatus to the approximate level of the medial canthus of the eye. A tight-fitting face mask requires a reservoir bag and adequate oxygen flow rates to prevent rebreathing of exhaled gases. Loose-fitting face masks result in lower inspired oxygen concentrations but still require a minimal oxygen flow rate of 10 L/min to prevent build-up of CO 2 in the mask. Sternal recumbent position, tactile and sensory stimulation, a judicious suction technique, and oxygen supplementation are sometimes sufficient therapy for foals with asphyxia or hypoxia.
Foals with severe asphyxia (Apgar score 0 to 3) need rapid, aggressive intervention to stimulate and support ventilation. Manual mouth-to-nose resuscitation can be accomplished with the clinician using both hands to occlude one of the foal’s nostrils and the mouth and then breathing rhythmically into the foal’s patent nostril to expand its lungs. Assisted ventilation is probably best performed with an endotracheal tube directly attached to a ventilator, an oxygen demand valve (Hudson oxygen demand valve II, Hudson Oxygen Therapy Sales, Wadsworth, OH), or a 1-L nonrebreathing resuscitation bag (Lifesaver II manual resuscitator, A. J. Buck and Son, Owings Mills, MD or E-Z Breather Foal Resuscitator, Animal Reproduction Systems, Chino, CA.) (Figure 11-3).
Oral intubation of the trachea can be done in emergency situations if short-term ventilation is all that is necessary. Nasotracheal intubation is better tolerated for prolonged periods. Inert plastic or silicone rubber endotracheal tubes with high-volume, low-pressure cuffs (Aire-Cuf, Biovona Medical Technologies, Gary, IN) are preferred to minimize tracheal mucosal damage. A breathing rate of 20 to 30 breaths/min should be maintained. Excessive ventilatory pressure can result in overinflation with alveolar rupture and pneumothorax. Visual assessment of the foal’s thorax is used to evaluate needed tidal volume.
Because the acidosis associated with terminal apnea usually is metabolic and respiratory in nature, administration of intravenous isotonic (1.3%) sodium bicarbonate solution at an initial dose of 2 mg/kg may help to correct the metabolic component. Administration of alkaline solutions without first ensuring that adequate ventilation is present can worsen the acidosis because sodium bicarbonate is converted to carbon dioxide and retained when poor ventilation-perfusion exists. Large volumes of hypertonic sodium bicarbonate solutions should be avoided; their use has been associated with hypernatremic and hyperosmotic states and with increased incidence of cerebrovascular accidents, especially in infants.
The ultimate outcome of severe, untreated asphyxia is myocardial and cerebral hypoxia, which result in death. Irreversible brain damage usually occurs after approximately 5 minutes of complete asphyxia. Therefore, the recognition and accurate, rapid treatment of asphyxia are vitally important.
INTERPRETATION OF CLINICAL LABORATORY DATA
Analysis of whole blood and serum from all newborn foals is customary on many well-managed broodmare farms. Blood samples for complete blood count (CBC), total protein, and fibrinogen as a component of the routine newborn foal examination provide a baseline for comparison if the foal has problems develop that become apparent later. In addition, despite the appearance of an apparently healthy foal, abnormal hematologic findings alert the veterinarian to the need for closer monitoring, or in some cases, the need to institute treatment (e.g., to control infection). Thus, proper interpretation of the laboratory results is reviewed here.
Normal hematologic, blood gas, and serum chemistry values for the newborn foal are cited in veterinary literature. Hematologic parameters of the newborn foal change during the first 2 weeks of life. Because of the shortened life span of erythrocytes in fetal and neonatal foals, the number of red blood cells peaks at term and then decreases during the next 10 days.
A relatively abrupt decrease in packed cell volume, hemoglobin concentration, and number of erythrocytes occurs within the first 12 to 24 hours post partum. The high hemoglobin concentration and packed cell volume at birth are attributed to the presence of peripheral vasoconstriction in animals immediately after birth, which offers physiologic protection against shock, cold, and excessive blood loss from the umbilicus. After parturition, a gradual release from this vasoconstriction occurs, and circulatory volume increases with a concomitant drop in packed cell volume, number of erythrocytes, and hemoglobin concentration.
An increased leukocyte count during the first 24 hours after birth primarily results from an increase in the number of mature neutrophils, which can continue during the next 3 days. However, the finding of more than 5% to 10% band cells suggests underlying disease (infection). The lymphopenia present at birth might result from immature lymphatic organs or from the response to endogenous steroid release during parturition. Lymphocyte numbers should continue to rise in early postnatal life. Eosinophils, basophils, and monocytes are low in number or absent in the newborn foal. Premature foals tend to have lower numbers of leukocytes and neutrophils. Neutrophil counts of less than 4000/mm 3 or more than 12,000/mm 3, band neutrophil counts of more than 50/mm 3, toxic changes in neutrophils, and fibrinogen concentrations of more than 500 to 600 mg/dL are predictive of sepsis or infection (Brewer and Koterba, 1990).
Concentrations of serum electrolytes remain relatively constant during the postnatal period. Liver enzyme concentrations generally are higher in neonates than in adults. The increased serum liver enzyme activity in foals is attributed to a relative increase in hepatic mass (as a percentage of total body weight) in the newborn and to a higher rate of enzyme production and release. The level of alkaline phosphatase is higher in foals up to 3 to 5 months of age because of osteoblastic activity of bone.
The dark yellow serum of newborn foals reflects increased postpartum bilirubin levels. An increase in the indirect bilirubin concentration accounts for the hyperbilirubinemia. Lower concentrations of glucuronyl transferase in the neonatal liver result in a slower conjugation of bilirubin during the first 5 days after birth. Bilirubin concentrations should approach adult values by 2 weeks of age. The bilirubin concentration is generally increased in foals with neonatal isoerythrolysis and may be of value in diagnosis of this condition when anemia, pallor, and tachypnea are present in newborns.
Serum creatinine concentrations during the neonatal period often are greater than adult values. This difference in creatinine levels probably reflects the initial immaturity of the renal transport and filtration systems. A markedly elevated serum creatinine concentration has been associated with both prematurity and neonatal maladjustment syndrome (NMS). Monitoring of creatinine levels is also necessary when drugs with a potential for renal toxicity, such as aminoglycosides, are administered to foals.
The blood glucose level of presuckle foals usually is lower than that in adults but increases after suckling. Sepsis or insufficient energy intake should be suspected in foals with low blood glucose concentrations, and the clinician should be aware of the need for closer monitoring of nursing activity, the possible presence of agalactia, and the need for additional testing or examination for septicemia. Hypoglycemia can be treated by administering 5% to 10% dextrose solutions intravenously.
Interpretation of clinical laboratory data must be done with an understanding of the normal physiologic and biochemical adaptations that occur in the neonate. A precise history of peripartum events and a careful physical examination always should precede the interpretation of laboratory data.
PHYSICAL EXAMINATION
A thorough, systematic physical examination should be performed on every foal during the first day of life. Before actual physical examination, the clinician should begin by observing the foal from a distance to assess its alertness and behavior, ability to rise, coordination and strength, desire and willingness to nurse, and overall attitude. Rectal temperature should always be determined and is normally 99.5°F to 100.5°F (37.5°C to 38.5°C). When rectal temperature is less than 98.5°F, hypothermia should be suspected. When rectal temperature exceeds 101.5°F, infection should be suspected.
The actual physical examination should be systematic, beginning at the head and progressing to the hindquarters. It should yield prompt recognition of various maladies, including cleft palate, eye abnormalities (e.g., entropion, micropthalmia, cataract), fractured ribs, umbilical problems (e.g., swollen, wet, bleeding, hernia), inguinal hernias, and limb abnormalities (e.g., valgus, varus, contractures, laxaties). The foal should possess a normal respiratory rate, heart rate, and rectal temperature. Its mucous membranes should be pink and moist. The veterinarian should also look for evidence that the foal has passed meconium and is suckling regularly (mare’s udder is not full and turgid).
The foal’s degree of maturity should be assessed. Signs that suggest prematurity include low birth weight, general weakness, inability to stand, decreased ability to suck and maintain body temperature, silky haircoat, floppy ears, soft lips, and increased passive range of limb motion with a decreased pastern slope. A premature foal also can have immature organ systems (e.g., pulmonary, endocrine, gastrointestinal, renal, immune, and hematopoietic system) and therefore need close observation and monitoring with appropriate supportive care.
Examination for Broken Ribs
With the foal standing and gently restrained, the thoracic cage is palpated in its entirety, usually with the practitioner standing over the foal and using both hands simultaneously, with the right hand on the right hemithorax and the left hand on the left hemithorax. Each rib is followed dorsally to ventrally. Any irregularity (displacement) or movement (usually felt as a “popping” or “clicking” sensation) is noted and examined more closely. Fractures can occur anywhere in the ribs but are more common ventrally or near the costochondral junction. Suspected fracture sites should be examined with transcutaneous ultrasound for confirmation of fracture and degree of displacement (Figure 11-4) and for evidence of pleural disruption or hemorrhage. Most commonly, one or perhaps two ribs are involved, but sometimes several are fractured, which places the foal at great risk for puncture or laceration of the pleura, lungs, or heart. In many cases, confining the foal and the mare to a large well-bedded stall for 2 or more weeks is a satisfactory method of management of broken ribs. Certainly, risk of further injury exists for the confined foal and could result in death. However, the goal is to do everything possible to avoid trauma to the foal’s thorax until the rib fracture is stabilized, thereby reducing risk of adverse consequences. Once firm callus formation around the fracture site has developed (confirmed with ultrasound examination and palpation of a stable thorax), the foal can be turned out with its dam in a small paddock for exercise. Separation from other mares and foals is necessary until satisfactory healing occurs, which is often evident within 4 to 6 weeks. Surgical techniques have been developed for fixation of fractured ribs and may be undertaken if chosen; however, even after surgery, accidents leading to pleural, lung, or cardiac puncture have occurred.
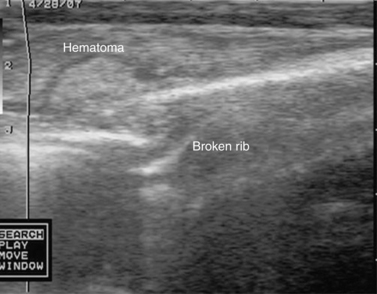 |
| Figure 11-4 (Courtesy Dr. Tom Seahorn, Lexington, KY.) |
Neurologic Examination
A brief neurologic examination should be performed and should include a systematic evaluation of general behavior, mentation, cranial nerve function, posture, gait, coordination, and spinal reflexes. A healthy newborn foal is aware of and responsive to its environment soon after birth and shows close bonding behavior with the dam. Certain physiologic differences between the neonate and the adult should be acknowledged. Equine neonates normally have limb hyperreflexia, resting extensor hypertonia, crossed extensor reflexes, hypermetric gait, base-wide stance, intention movements, and an absence of menace response. Neurologic abnormalities should be recognized, identified as to cause (e.g., developmental, infectious, or from vascular accidents within the central nervous system), and treated accordingly.
Peripartum asphyxia or hypoxia can result in a syndrome (hypoxic ischemic encephalomyelopathy [HIE]), often referred to as maladjusment, with variable clinical signs including abnormal behaviors, mentation (Figure 11-5), or seizures and secondary consequences, such as atelectasis and acidosis; thus, many cases should be managed in a neonatal intensive care hospital ward. The pathogenesis, diagnosis, and treatment of the disorder are discussed thoroughly in equine neonatology texts (e.g., Knottenbelt et al., 2004).
 |
| Figure 11-5 (Courtesy Dr. Tom Seahorn, Lexington, KY.) |
Cardiovascular System Examination
Evaluation of the cardiovascular system begins with examination of the visible mucous membranes, which should be pink and moist with a capillary refill time of 1 to 2 seconds. The jugular veins should not be distended but should fill readily when occluded at the thoracic inlet. Jugular pulsations reflect normal pressure changes within the right atrium and the thorax and should not extend beyond the level of the point of the shoulder. The apex beat, easily palpated over the left fifth intercostal space in the ventral third of the thorax, should be evaluated for intensity and for the presence of murmur-associated thrills.
Arterial pulses should be strong and readily palpable in the extremities, indicating adequate peripheral perfusion. Percussion of the left hemithorax outlines a normal area of cardiac dullness that extends from the fourth intercostal space just below the point of the shoulder to the sternum at the sixth intercostal space. A smaller area of cardiac dullness is found over the right third and fourth intercostal spaces.
Auscultation of the heart base requires a general knowledge of the anatomic location of the four heart valves. Foals generally have loud heart sounds on auscultation because of their thin body wall and small size. The most commonly reported murmur in newborn foals is associated with blood flow through a persistent patent ductus arteriosus and is characterized by a continuous machine-like murmur that is loudest over the left heart base. The diastolic component of the murmur often is localized over the left third or fourth intercostal space, whereas the systolic component may be heard easily over the entire heart base. Continuous murmurs associated with a patent ductus arteriosus disappear in some normal foals by 24 hours of age and are considered abnormal if present beyond 4 days of age. Pulmonary hypertension can reduce the intensity of the diastolic component.
The heart rate of the foal is 40 to 80 regular beats/min initially but increases to 150 beats/min when the foal struggles to rise. It then falls to a rate of 70 to 95 beats/min. Sinus tachycardia can be associated with stress, excitement, fever, hypovolemia, or sepsis. Bradycardia can occur with hyperkalemia, hypertension, or increased intracranial pressure.
Respiratory System Examination
The respiratory rate, effort, and pattern should be examined carefully in the resting foal before handling (because any handling results in excitement of the foal). The rate decreases from a mean of 75 breaths/min at birth, to 50 breaths/min at 1 hour, and to 34 breaths/min at 12 hours of age. Lung sounds in the young foal typically are louder, harsher, and easier to hear than in the adult. The auscultation of moist rales in the neonate can stem from fluid accumulation in the lungs that has not yet dissipated completely. Decreased or absent lung sounds can be associated with lung atelectasis or consolidation related to lung immaturity or pneumonia.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





