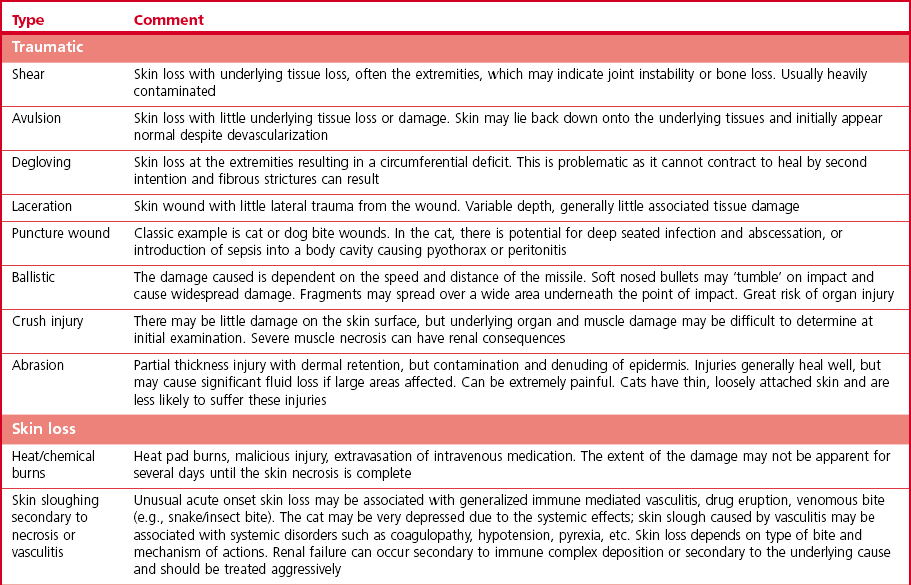
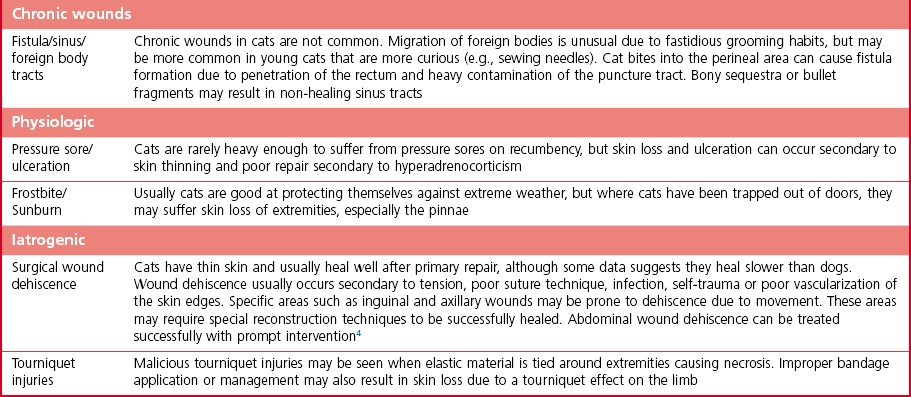
Chapter 18 Wound management has been a developing field for thousands of years, with the earliest records dating from ancient Egypt citing remedies of honey, resin, and grease for open wounds. However, it is only in the last 40 years that the role of moist wound healing and the complex interactions of growth factors and vascular supply have become accepted. Wound healing in the cat has unique characteristics (Chapter 17) and this has implications for wound management.1–3 In general, the principle of more rapid healing in a moist environment is now widely accepted for wound management protocols in all species. The principles of wound management should revolve around a clear understanding of wound healing in cats. The gross appearance of the different stages of wound healing is important in decision making, as is the recognition of an inflamed wound, a chronic wound, or an infected wound. Direct comparison with wounds seen in other species is unhelpful as cats tend to have paler wounds, when compared with dogs, for example, and the skin and granulation tissue layers are thinner and more fragile. Progression of the wound is slower and responses to wound healing stimulants may be less brisk than seen in the dog (Chapter 17). Cats are usually very fastidious about grooming and cautious about investigating objects that could cause harm. However, young cats are more likely to injure themselves in road traffic accidents, fall through trees, or be attacked by dogs or other cats. Occasionally, malicious injury is seen when cats present with burns, elastic band induced necrosis of extremities, or ballistic injury. Owners rarely see the accident and the typical history is that the cat returned to the house with the injury, or was found near the house. Close examination of the cat may provide information as to the type of injury and from there the history can be extrapolated. The etiology of wound types and formation in cats is summarized in Table 18-1. A minimum database would involve thoracic auscultation, abdominal palpation, temperature, pulse, respiration, determination of shock, dehydration and a base line packed cell volume/total protein, electrolytes, blood urea nitrogen (BUN) and creatinine. Cats frequently present some time after the original injury, so are often dehydrated on presentation, making interpretation of blood results and assessment of blood loss or electrolyte disorders such as hypokalemia difficult. A minimum hematology and serum biochemistry database is helpful in order to determine the general condition and ancillary disorders that require treatment as well as the wound. Older cats may have previously unrecognized diseases detected at this time, but this should not necessarily preclude treatment of the wounds/injuries. For example, elevated BUN/creatinine results should be interpreted with caution until it is clear whether this is renal or pre-renal in origin. Neurologic examination is carried out if the cat is unable to stand or has deep injuries over or near the spinal column or major peripheral nerves. This is particularly important when it is expected that distal limbs will be bandaged, as determination of neurologic deficits may be important to the prognosis, but difficult to recognize once the cat is bandaged. Furthermore, as subsequent dressing changes may be carried out under anesthesia or sedation, an accurate determination of neurologic status may be difficult at a later date. Thoracic radiographs should also be taken to rule out diaphragmatic rupture, pulmonary contusion, or pleural hemorrhage. On admission, a record is made of the location of the wound and associated injuries together with an accurate description of the condition of the wound. This enables objective monitoring of wounds that may continue to progress after treatment has started, due to poor vascular supply. A dated photographic record of the wound should be made in the case of suspected malicious or ballistic wounds. Generally, wounds can be assessed in three stages (Fig. 18-1). These stages may all occur within a few hours, or within days, depending on the nature of the wounds and injuries. All cases showing signs of shock that present with a traumatic injury should be treated appropriately (see Chapter 1). Supplemental oxygen should be provided during handling in the dyspneic patient until the possibility of associated thoracic injury has been ruled out. Hypothermia is a common finding on initial presentation, partly due to shock, but also if the cat has been collapsed outside for a period of time. This will need appropriate management and gradual warming by the use of heat pads, water beds, warming IV fluids, wheat bags, bubble wrap, space blankets, and so on (see Chapter 4). Analgesics should be initiated immediately on admission, regardless of patient status. This improves patient handling and prevents further ‘wind up’ of the pain pathways prior to wound management.5 The clinical records should list minimum information regarding the wound at this stage (Box 18-1). Photographs of the wound are a useful addition to the clinical records. Some dressings come with paper templates with centimeter grading so an approximate drawing can be made of the wound shape and size. The presence of other injuries whether or not directly associated with the wound (e.g., a jaw fracture which may affect the cat’s ability to maintain nutrition during the period of treatment) should also be noted in the patient’s record. Sterile instruments are used to investigate the wound, lifting skin flaps and gently probing penetrating injuries. This may prompt further diagnostic procedures such as radiography or ultrasound to determine the involvement of deeper structures. For example, a penetrating injury over the thoracic skin should be carefully assessed to ensure that pleural contamination or injury is not missed. Assessment of the vascular supply to peripheral injuries can be difficult; although angiography is the definitive way to determine the viability of arterial supply to the distal limb, often animals with this level of injury are not suitable candidates for long procedures under anesthesia, and intravenous contrast agents are contraindicated in cats where the systemic circulation is compromised in any way. Thus assessment of vascular supply often relies on clinical acumen and non-invasive techniques: feeling the toes for warmth, palpating distal pulses, using color flow ultrasound or Doppler detection of blood flow. Visual assessment of the color of non-pigmented pads and needle pinpricks can also be used to assess bleeding (Fig. 18-2). However, the clinician should be aware that extremities will appear cold and pale in cats with shock or hypothermia, and clinical examination should be repeated regularly as resuscitation proceeds. Needle pinpricks should also be interpreted with caution in these circumstances and bleeding due to venous stasis or coagulopathy may be misleading. Needle pinpricks can also introduce infection into healthy tissue. Figure 18-2 This cat presented 24 hours after injury and the digital pads were clearly cyanotic, indicating very poor peripheral perfusion. The foot was cold to touch but the cat was normothermic. Following first aid and then the initial management, the wound is managed on a daily or as needed basis. Bandages and dressings are often changed daily in the early stages of wound management and then the frequency of changes is reduced according to the contamination and progression of healing. The biggest challenge with open wound management in cats is maintenance of the bandage. Cats tolerate bandages poorly and frequently shake the affected leg or chew at the dressing to try and remove it. Elizabethan, Buster or ‘tube’ collars may be necessary to maintain the bandage (see Chapter 4), but care should be taken to monitor water and food intake with these collars on. In addition, persistent attempts to remove the bandage may cause it to slip and then it must be replaced in order to avoid risk of a bandage-related ischemic injury.6 Hospitalization of cats with wounds ensures close monitoring, but soiling of the bandage due to use of the litter tray or the confined space of the kennel may bring additional challenges. Sedation or anesthesia for dressing changes is advisable both to reduce the stress and pain for the cat, and also for staff safety. Daily dressing changes can be extremely stressful for both cat and staff if they are done without adequate analgesia. However, this requires careful planning and review of the medications used; regular sedation may result in nausea and inappetence on top of a reluctance to eat in the hospital. Analgesics such as non-steroidal anti-inflammatory drugs (NSAIDs) should not be given on an empty stomach and this makes management of the cat’s analgesic protocol more difficult. Nursing staff must weigh the cat daily (taking the dressings into consideration) to monitor any weight loss, and accurate recording of nutritional intake is essential. The aim of the daily management plan should be that the cat is sedated and the dressing changed as early as possible so as to give nursing staff plenty of time during the day to provide the cat with opportunities to eat or be encouraged to do so (see Chapter 6 and 7). Cats that require prolonged wound management may benefit from a feeding tube such as an esophagostomy tube (see Chapter 12). Most of these cases will also benefit from maintenance intravenous fluids for the duration of their treatment, preventing dehydration due to lack of water intake during this period. A simple mnemonic has been devised by the International Wound Bed Advisory Board,7 which provides a practical working framework that can be used consistently from one dressing change to the next even if there has been a change in staff. This mnemonic enables consistent wound assessment and treatment plans to be recorded at each dressing change (Box 18-3). There are a huge number of primary layer dressings and this makes it confusing for the veterinary surgeon or nurse to know how to apply the principles of wound management to the wound. Nearly all wound dressings have been developed for use in the human market and there is very little objective data on how these dressings perform in cats. Wound dressings can be defined by what they achieve on application to the wound (Table 18-2).8 There is no perfect wound dressing and many products are able to carry out more than one role. Thus a hydrogel may achieve debridement by enabling autolytic separation of necrotic tissue, but also trap exudate and inflammatory mediators, drawing fluid out of the wound and reducing edema. Table 18-2 Summary of contact layer products for wound dressings The single most important step in early wound management is adequate debridement. Not only is this the most effective way to treat infected wounds, but it also prevents infection by removing foreign material and purulent inflammatory exudate, thus preventing the perpetuation of inflammatory responses in the wound and encouraging the development of granulation tissue. The most frequently used debriding dressing is the ‘wet-to-dry’ dressing, where a sterile gauze swab is moistened with sterile isotonic fluid (e.g., Hartmann’s solution) and placed onto the wound for 12–24 hours. When the dressing is removed, it pulls away the surface necrotic material, together with trapped exudate and inflammatory mediators (Fig. 18-5). This is a relatively inexpensive and easy treatment for heavily contaminated wounds, but the swabs are painful to remove and few cats will tolerate this dressing change without adequate sedation/analgesia or anesthesia. Wet-to-dry dressings may also damage tissue that is already healthy and in cats may severely damage the thin fragile granulation tissue. Hydrogels can also be used to debride wounds and may be a ‘gentler’ alternative (Fig. 18-4E). Gels can rehydrate dry necrotic material, enabling autolytic processes to separate them from the underlying tissue, as well as trap fluid within the gel structure allowing it to be removed from the surface of the wound and flushed away during lavage. Hydrogels are usually applied underneath another dressing (e.g., foam backed with semi-permeable membrane; Fig. 18-6) in order to hold the gel in the wound and prevent desiccation. Cat wounds are rarely very productive and using products that keep the wound moist is important. Figure 18-5 A wet-to-dry dressing debrides the wound by pulling exudate and necrotic tissue off the surface at each dressing change. It will also damage healthy granulation tissue.
Wounds and wound management
History
Initial assessment and wound management
Initial treatment of the wounded cat
Definitive wound assessment

Daily wound management
The bandage
Primary layer
Product type
Examples (not comprehensive)
Action/indications
Polyurethane membranes
Melolin (Smith and Nephew)
A sterile protective surface but does not maintain tissue hydration
Polyurethane foam
Allevyn (Smith and Nephew)
Absorption of fluid from wound surface and controlled evaporation maintaining a humid environment
Hydrogels
Intrasite gel Flexigel (sheet form) (Smith and Nephew)
Rehydration of tissue, absorption of fluid and maintaining a moist environment. May be analgesic if applied cold and may be used combined with other products on the wound surface, e.g., antibacterial drugs, alginates
Hydrocolloid
Granuflex (Convatec)
Water is trapped in the colloid and autolytic debridement is promoted. Debris may be trapped in the colloid gel that is produced on interaction with exudate
Alginates
Kaltostat (Convatec) Tegaderm (3M)
Active stimulation of inflammatory processes in wounds. Must be in a moist environment otherwise may be irritant
Collagens
Biosist (Dechra Veterinary Products)
May improve healing by encouraging fluid flow through the wound and providing a ‘scaffold’ for granulation tissue
Silver dressings
Acticoat (Smith and Nephew)
Bactericidal and may also stimulate healing
Acemannan
Aloe Vera creams (various)
Stimulation of healing and reduction of inflammatory responses8
Honey
Activon (Advancis Medical)
Bactericidal, stimulation of healing, draws fluid through the wound, encourages autolysis
Debriding dressings

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Wounds and wound management