Ventricular Premature Complex and Ventricular Tachycardia
Basic Information 
Definition
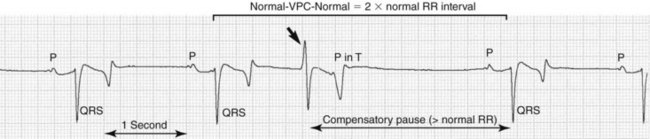
• Ventricular premature complex (VPC): A spontaneous premature ventricular depolarization that originates from the ventricles, resulting in a QRS′ complex and T′ wave on the surface electrocardiogram (ECG) that have a different morphology (and duration) (Figure 1).
• Ventricular tachycardia (VT): More than three consecutive VPCs, resulting in an increased heart rate.
• Idioventricular rhythm: An independent pacemaker in the ventricles discharging at a relatively slow rate, dominating the cardiac rhythm, resulting in a normal or almost normal heart rate.
• Fusion beat: A VPC that originates almost simultaneously with the normal ventricular depolarization. The morphology of this fusion beat is a mixture between the normal QRS and the VPC morphology.
Clinical Presentation
Disease Forms/Subtypes
• Depending on the number of VPCs
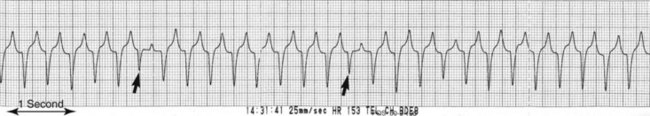
• Depending on the morphology of the QRS′ complex (Figure 2)
 Monomorphic (originating from the same focus; unifocal, uniform) VPCs or VT versus polymorphic (originating from different foci; multifocal, multimorphic, multiform) VPCs or VT
Monomorphic (originating from the same focus; unifocal, uniform) VPCs or VT versus polymorphic (originating from different foci; multifocal, multimorphic, multiform) VPCs or VT• Depending on the duration of VT
Physical Exam Findings
 Irregular rhythm on auscultation. The VPC may have an increased intensity of the first heart sound and is usually followed by a compensatory pause.
Irregular rhythm on auscultation. The VPC may have an increased intensity of the first heart sound and is usually followed by a compensatory pause. An increased heart rate: Generally more than 50 beats/min; sustained monomorphic VT usually results in a heart rate above 100 to 120 beats/min.
An increased heart rate: Generally more than 50 beats/min; sustained monomorphic VT usually results in a heart rate above 100 to 120 beats/min. At excessively high rates, not every QRS′ is associated with semilunar valve opening and heart sounds. Therefore, calculation of heart rate by auscultation may underestimate the actual heart rate.
At excessively high rates, not every QRS′ is associated with semilunar valve opening and heart sounds. Therefore, calculation of heart rate by auscultation may underestimate the actual heart rate. Horses with sustained VT develop jugular pulsation, ventral edema, hydrothorax, or even pulmonary edema, hydropericardium and ascites.
Horses with sustained VT develop jugular pulsation, ventral edema, hydrothorax, or even pulmonary edema, hydropericardium and ascites. Signs of underlying cardiac disease such as congestive heart failure, diastolic murmur, weakness, or (pre)syncope
Signs of underlying cardiac disease such as congestive heart failure, diastolic murmur, weakness, or (pre)syncopeEtiology and Pathophysiology
• Spontaneous impulse formation (by increased automaticity, triggered activity or reentry) occurs in the ventricles usually because of primary cardiac disease.
 Myocardial inflammation, degeneration, or necrosis caused by infection (bacterial, viral, parasitic), intoxication (cardiac glycosides, monensin), or neoplasia
Myocardial inflammation, degeneration, or necrosis caused by infection (bacterial, viral, parasitic), intoxication (cardiac glycosides, monensin), or neoplasia• Underlying systemic disorders may cause or enhance ventricular ectopy
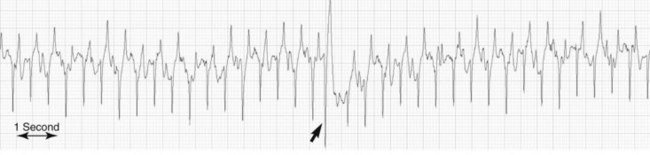
 Maximal exercise: An occasional ectopic beat (usually during recovery) should be considered as normal in maximally exercising horses (Figure 3)
Maximal exercise: An occasional ectopic beat (usually during recovery) should be considered as normal in maximally exercising horses (Figure 3) Iatrogenic: During cardiac catheterization or transvenous electrical cardioversion of atrial fibrillation (AF)
Iatrogenic: During cardiac catheterization or transvenous electrical cardioversion of atrial fibrillation (AF)• The ectopic impulse depolarizes both ventricles but follows a different route through the myocardium, resulting in a QRS′ complex with a different morphology and a longer duration.
• Depending on the site of origin, the QRS′ complex may be completely abnormal or may be difficult to distinguish from the normal complexes (when it originates high in the ventricle near the His-Purkinje system).
• Isolated ectopic beats have limited hemodynamic consequences and may not result in obvious clinical signs.
• VT has an important impact on hemodynamics. Sustained VT at high rates leads to cardiac failure within days.
• VT of less than about 140 beats/min, especially if polymorphic, is usually caused by increased automaticity. Monomorphic VT of more than about 140 beats/min is usually caused by a rapidly firing focus, triggered activity, or reentry.
• Any ventricular ectopic rhythm carries a risk for sudden initiation of high rate VT or flutter (signs of weakness, ataxia, and [pre]syncope) or even ventricular fibrillation (VF; sudden death).
Diagnosis 
Differential Diagnosis
• Supraventricular tachycardia (sinus tachycardia or atrial tachycardia): QRS complexes of normal morphology and duration are preceded by P waves (P waves may be buried in the preceding T waves).
• VF: The ECG shows a bizarre wavy line, and QRS complexes can no longer be identified. VF warrants immediate therapy because it is always fatal within seconds to minutes.
• Aberrant conduction in horses with AF: In AF, sympathetic stimulation or exercise may result in extremely high ventricular rates (up to >400 beats/min). Occasionally, QRS broadening and an R-on-T phenomenon may be found. Although AF and VPC/VT may occur concurrently, these extremely high rates are probably supraventricular in origin (sudden conduction of atrial impulses through the atrioventricular (AV) node because of the change in autonomic tone) whereby an aberrant conduction to the ventricles results in broader QRS complexes and R-on-T.
• Ventricular escape rhythm: Because of the absence of a normal ventricular depolarization, an ectopic beat is generated in the ventricles, resulting in a QRS′ complex that occurs later than normal and has an abnormal morphology and duration.
• Artifacts, especially during muscle twitching, body movement, and exercise. Important criteria for differentiation include
 The normal QRS complex is the fastest depolarization of the ventricles. Sharp deflections of shorter duration are artifacts (eg, muscle twitching).
The normal QRS complex is the fastest depolarization of the ventricles. Sharp deflections of shorter duration are artifacts (eg, muscle twitching).Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree