8 Toxic Exposures
HEALTHY HOMES
The concept of a “healthy home” as promoted by the U.S. Department of Housing and Urban Development (HUD) and other federal agencies involves not only aspects of the built environment (see Chapter 6), but also creating homes that are safe in terms of toxic hazards such as carbon monoxide and pesticides.1 This concept is one in which human health care providers, public health professionals, and veterinarians can actively collaborate because it seems clear that what is good for the human beings in the household in terms of toxic hazard reduction is also good for animals living in the household.
In the early part of the twentieth century, miners in the United States and Great Britain brought caged canaries into mines to provide an early warning of the presence of deadly gases such as carbon monoxide and methane. Studies had shown that the canaries were more sensitive than other species to the effects of these gases,2 and a canary becoming ill and falling from its perch was sufficiently recognizable to warn the miners of the hazard. In the same way, animals living in or near a household can serve as “sentinels” for human health hazards related to toxic exposures in the home and other environments. Much of what is known about the toxic properties of environmental chemicals is based on studies of laboratory animals such as rats and mice. However, pets, other domestic animals, and wildlife can provide both clinically important information to human health as well as useful “animal models” of cancer and other environmentally induced disease.3
Key Points for Clinicians and Public Health Professionals
Public Health Professionals
 Use integrated pest management (IPM) techniques for rodent, weed, and insect control to reduce dependence on toxic substances. (See, for example, http://www.epa.gov/pesticides/factsheets/ipm.htm.) IPM is a commonsense and environmentally sensitive approach to pest management that uses current, comprehensive information on the life cycles of pests and their interaction with the environment.
Use integrated pest management (IPM) techniques for rodent, weed, and insect control to reduce dependence on toxic substances. (See, for example, http://www.epa.gov/pesticides/factsheets/ipm.htm.) IPM is a commonsense and environmentally sensitive approach to pest management that uses current, comprehensive information on the life cycles of pests and their interaction with the environment.Human Health Clinicians
Veterinary Clinicians
PRIMARY PREVENTION OF TOXIC EXPOSURE
Pet Proofing and Child Proofing
Pets and children share the potential for accidentally ingesting toxic substances left around a house or yard. Keep toxic substances such as cleaning solutions, flea and tick preparations, other pesticides, and all medications out of reach of pets and children. Encourage smoking cessation to protect the health of the smoker and human beings and animals exposed to secondhand smoke (Figure 8-1).
ANIMALS AS SENTINELS FOR HUMAN TOXIC EXPOSURE RISK
Six years before the detection of Minamata disease, an outbreak of severe methyl mercury poisoning among families living near Minamata Harbor in Japan, strange clinical signs were seen in local cats that ate diets high in fish from the bay. This “dancing cat disease” included twitching, spasms, abnormal movements, and convulsions. Only later was the association made between the neurological signs in the cats and the devastating signs of mercury poisoning in children and adults (who also ate mercury-contaminated fish from the bay) that included mental retardation, seizures, and other neurological damage.4
The inappropriate use of melamine as a filler substance in pet foods has been blamed for thousands of animal deaths from renal failure.5 Unfortunately, this scandal did not protect against the subsequent unscrupulous use of the “protein booster” in powdered baby formula in China, which led to illness and death in human infants the following year.6
A National Academy of Sciences panel has concluded that domestic animals and wildlife could serve as useful sentinels of human environmental health hazards because they may develop recognizable signs or biomarkers of toxicity in a timely way to provide a warning to human beings and to assist in human risk assessment.7 Animals may function as sentinels when there are differences between animals and human beings regarding exposure, susceptibility, or latency to a particular hazard. At times, an unusual cluster of disease in an animal population may suffice to draw attention to a particular hazard. For example, when horses (and dogs) in Times Beach, Missouri, began to die after their stable area was sprayed with oil to control dust, it was discovered that the oil was contaminated with dioxin.8 The Times Beach incident was the largest community-wide exposure to dioxin in the United States.
Routes of Exposure
Perhaps the most likely opportunity for animals to serve as sentinels of household toxic exposures is by their greater exposure risk. Dogs are well known for their propensity to ingest a wide variety of substances, including lead-containing dusts and household cleaning agents, and therefore may be the first in a household to manifest signs. Household pets also spend more time in the home environment and thus could have a higher exposure risk to a number of substances present in the home. For example, cats and dogs may have increased exposure to dust compared with human beings because they live close to the floor level and often lick their fur during grooming (especially cats). Dust in a household may contain accumulations of chemicals, including flame retardants, lead, mercury, phthalates, and perfluorochemicals (used in nonstick cookware) and can lead to significant toxic exposures in human beings and other animals in the house. A recent study of levels of chemicals in the blood and urine of dogs and cats found levels of flame retardants in cats more than 20 times the average level in human populations, levels of mercury more than five times as high, and levels of perfluorochemicals in dogs more than double that found in the general human population.9 These finding indicate that pets may have increased exposure to many toxicants found in household dust and fumes compared with human beings and therefore may be at risk of showing signs sooner or with greater severity.
Outdoors, dogs and cats may dig in the soil around a house or in adjacent neighborhoods, exposing themselves to lead, pesticides, arsenic, and other toxic chemicals that could be in soil. Some authorities have expressed concern that pets could then track such contaminated soil into a house on their paws and fur, potentially increasing the exposure risk for children and other inhabitants.10 Wildlife and livestock often live continuously in outdoor environments near human beings and may be exposed to toxicants in water, air, soil, and food sources, including vegetation, at much higher levels than human beings.
Metabolic Fate/Susceptibility
Physiological differences in metabolism in some animals may make them more sensitive than human beings to certain toxicants. Canaries were found to be more sensitive than human beings to the toxic effects of carbon monoxide and methane gas in coal mines, allowing them to provide early warning to miners if they began to act sick (Figure 8-2). Dogs lack the metabolizing enzyme rhodanese and therefore may have effects of cyanide poisoning at lower doses than human beings. Birds appear to be more sensitive than human beings to inhalation of fumes from burning polytetrafluoroethylene (PTFE; Teflon [DuPont, Wilmington, Del.]).11

Figure 8-2 Canaries are popular caged birds that are revered for their beauty and singing qualities.
(From Tully TN Jr: Birds. In Mitchell MA, Tully TN Jr (eds): Manual of exotic pet practice, St Louis, 2008, Saunders Elsevier.)
Susceptibility to acute and chronic exposure to toxicants may vary within species according to breed, sex, age, neutering status, or other differences. For example, the risk of nasal cancer in dogs (which has been linked to indoor air pollution; see below) may be higher in long-nosed dogs because of anatomical differences that allow different degrees of contact between carcinogenic air pollutants such as polyaromatic hydrocarbons (PAHs) and the lining of their nasal passages compared with short-nosed dogs.12 An increased risk of bladder cancer has been reported in obese female dogs; the reasons for this are not clear.12
An example of interspecies differences in susceptibility to toxic exposures can be seen in the list of human foods that are toxic to some companion animals (Table 8-1) and common human medications that may be highly toxic to pets at relatively low doses.
Table 8-1 Partial List of Foods Toxic to Companion Animals
| Food (Ingredient) | Toxic Effect in Dogs | Toxic Effect in Cats |
|---|---|---|
| Alcoholic beverages (ethanol) | Ataxia, respiratory depression, cardiac abnormalities, death (acute toxicity with 5-8 mL/kg; oral LD50 5500 mg/kg in dogs) | Ataxia, respiratory depression, cardiac abnormalities, death (acute toxicity with 5-8 mL/kg) |
| Avocado (persin) | Vomiting, diarrhea | None known |
| Chocolate (theobromine) | Vomiting, diarrhea, tremors, seizures, death (250-500 mg/kg LD50 in dogs) | Vomiting, diarrhea, tremors, seizures, death (200 mg/kg LD50 in cats) |
| Coffee (all forms) (caffeine) | Vomiting, diarrhea, tremors, seizures, death (LD50 140-150 mg/kg in dogs) | Vomiting, diarrhea, tremors, seizures, death (LD50 100-150 mg/kg in cats) |
| Fatty foods | Steatorrhea, diarrhea, obesity, pancreatitis | Steatorrhea, diarrhea, obesity |
| Macadamia nuts | Vomiting, depression, ataxia (2.2 g/kg)13 | None known |
| Moldy foods (tremorgenic mycotoxins) | Muscle tremors, seizures | Muscle tremors, seizures |
| Onions, onion powder, garlic, leeks, chives (propyl disulfide)13 | Hemolysis (11 g raw onions/kg) | Hemolysis (28 g raw onion/kg) |
| Raisins and grapes | Acute renal failure (no apparent dose response) | None known |
| Yeast dough (ethanol) | Abdominal distention, ethanol toxicosis | Abdominal distention, ethanol toxicosis |
LD50, Median lethal dose.
Latency
Another way in which animals may be a sentinel for human illness is if they develop signs in a shorter period of time (latency). This may be more important for chronic rather than acute toxic exposures. Most companion animals have a shorter average lifespan than human beings. Therefore chronic disease effects from environmental exposures tend to have a shorter latency. An example is the finding of mesothelioma in dogs whose owners had occupational or hobby exposure to asbestos (which resulted in secondary exposure of the household dog and other human beings in the household) (Color Plate 8-1). The average age of the dogs at time of diagnosis was 8 years (48 “dog years”), whereas mesothelioma in human asbestos exposure has a usual latency (time since asbestos exposure) in excess of 20 years.14
ACUTE TOXIC EXPOSURES
Accidental poisoning is a major cause of acute injury and death in the United States. The national network of poison control centers in the United States provides emergency advice to individuals and health care professionals about human poisonings (800–222–1222).15
Each year more than 2 million cases of acute toxic exposures are reported to regional poison control centers, and many others are treated in emergency departments without formal reporting.16 The majority of human poisonings involve young children, and the most common source of poisoning is from prescription medications. However, other common exposures include cleaning substances and pesticides. Table 8-2 shows the substances most commonly involved in human exposures reported to poison control centers.
Table 8-2 Top 25 Substances Involved in Human Exposures Reported to American Association of Poison Control Centers, 2006
| Substance | No. | %* |
|---|---|---|
| Analgesics | 284,906 | 11.9 |
| Cosmetics/personal care products | 214,780 | 8.9 |
| Cleaning substances (household) | 214,091 | 8.9 |
| Sedative/hypnotics/antipsychotics | 141,150 | 5.9 |
| Foreign bodies/toys/miscellaneous | 120,752 | 5.0 |
| Cold and cough preparations | 114,559 | 4.8 |
| Topical preparations | 108,308 | 4.5 |
| Pesticides | 96,811 | 4.0 |
| Antidepressants | 95,327 | 4.0 |
| Bites and envenomations | 82,133 | 3.4 |
| Cardiovascular drugs | 80,426 | 3.3 |
| Alcohols | 76,531 | 3.2 |
| Antihistamines | 75,070 | 3.1 |
| Food products/food poisoning | 66,115 | 2.8 |
| Antimicrobials | 66,017 | 2.7 |
| Plants | 64,236 | 2.7 |
| Vitamins | 63,331 | 2.6 |
| Hormones and hormone antagonists | 51,875 | 2.2 |
| Gastrointestinal preparations | 50,914 | 2.1 |
| Hydrocarbons | 49,526 | 2.1 |
| Chemicals | 47,557 | 2.0 |
| Stimulants and street drugs | 46,239 | 1.9 |
| Anticonvulsants | 40,476 | 1.7 |
| Fumes/gases/vapors | 39,586 | 1.6 |
| Arts/crafts/office supplies | 37,990 | 1.0 |
* Percentages are based on the total number of human exposures (2,403,539) rather than the total number of substances.
From Bronstein AC, Spyker DA, Cantilena LR Jr et al: 2006 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS), Clin Toxicol (Phil) 45(8):815-917, 2007.
Animals also experience acute poisoning episodes. In fact, a significant number of calls to human poison control centers involve nonhuman animals. As Table 8-3 shows, reported poisoning in dogs is much more frequent than in cats, and poisonings in other species, including livestock and wildlife, are much less likely to be reported.11 In addition to animal reports to human poison control centers, acute poisoning episodes in animals are reported to veterinary practices and a network of animal poison control centers in the United States and other countries. The American Society for the Prevention of Cruelty to Animals (ASPCA) maintains the national Animal Poison Control Center, a 24-hour resource for practitioners managing acute toxic exposures in animals.17 An online information system has been developed in Switzerland for the management of poisoning in large and small animals (http://www.clinitox.ch).18 France also has a national service (http://www.vet-lyon.fr).19
Table 8-3 Nonhuman Exposures by Animal Type Reported to American Association of Poison Control Centers
| Animal | No. | % |
|---|---|---|
| Dog | 114,599 | 89.3 |
| Cat | 12,002 | 9.4 |
| Bird | 482 | 0.4 |
| Rodent/lagomorph | 417 | 0.3 |
| Horse | 264 | 0.2 |
| Sheep/goat | 105 | 0.1 |
| Cow | 41 | 0 |
| Aquatic | 40 | 0 |
| Other | 403 | 0.3 |
| Total | 128,353 | 100 |
From Bronstein AC, Spyker DA, Cantilena LR Jr et al: 2006 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS), Clin Toxicol (Phil) 45(8):815-917, 2007.
Table 8-4 shows the distribution of substances accounting for toxic exposures in animals reported to poison control centers and veterinary practices in 2006. Chocolate ingestion, rodenticide exposure (also a hazard to children in a house), and medications (especially analgesics) account for the majority of animal poisoning reports. Animals can be exposed to pharmaceuticals from ingesting human medications that are left unsecured within a household and from inappropriate administration of human or veterinary medications by human beings. Inappropriate ingestion also accounts for much of exposure to rodenticides, pesticides (including slug bait), poisonous plants, and cleaning products.20,21 An acute toxic poisoning in an animal can therefore be a warning sign of inappropriate access to hazardous products. This situation should alert human health and animal health care providers to take steps to avoid further pet or children’s exposures.
Table 8-4 Exposures of Animals to Various Toxic Agents Reported by Veterinary Clinics and Poison Control Centers
| Agent | Relative Frequency (%) |
|---|---|
| Chocolate | 26 |
| Rodenticides | 26 |
| Pharmaceuticals | 22 |
| Pesticides | 13 |
| Plants | 5 |
| Miscellaneous | 3 |
| Glycols | 1 |
Adapted from Gwaltney-Brandt SM: Epidemiology of animal poisonings. In Gupta RC (ed): Veterinary toxicology: basic and clinical principles, New York, 2007, Academic Press.
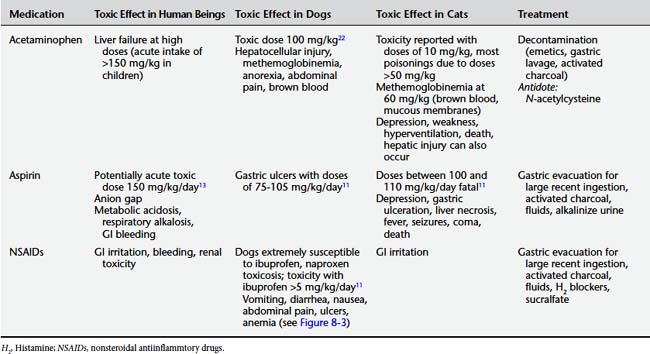
Common Medications and Their Toxicity in Human Beings and Animals
Acetaminophen
Acetaminophen, a principal component of a large number of analgesic medications, is an excellent example of differential interspecies susceptibility to toxic exposures. The drug is metabolized in the liver by uridine diphosphate (UDP)–glucuronyl transferase 1,6 to glucuronide and excreted via the kidneys. Another detoxification pathway is sulfation. Acetaminophen can also be oxidized through the cytochrome P450 (CP450) system to N-acetyl-p-benzoquinone imine, which is toxic to the liver. Cats have only one tenth of the glucuronyl transferase activity compared with dogs and are therefore highly susceptible to acetaminophen toxicity. The clinical signs of toxicity differ somewhat among human beings and dogs and cats; in human beings, the principal complication of overdose is liver toxicity, whereas in cats methemoglobinemia predominates. Both hepatocellular injury and methemoglobinemia develop in dogs.11
Nonsteroidal Antiinflammatory Drugs
Nonsteroidal antiinflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can cause GI irritation and bleeding in human beings, dogs, and cats. Dogs can be highly susceptible to the toxic effects of NSAIDs (Figure 8-3).11Table 8-5 lists the toxic effects in human beings and companion animals of several common analgesics.
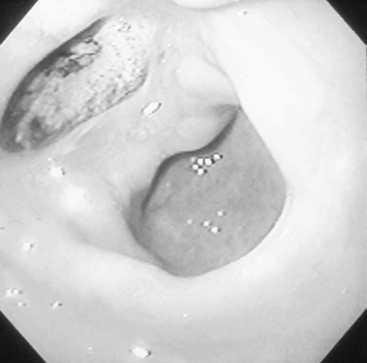
Figure 8-3 Gastric ulcer resulting from NSAID use in a dog.
(From Peterson ME, Talcott PA: Small animal toxicology, ed 2, St Louis, 2006, Saunders Elsevier. Courtesy Dr. M. Kern.)
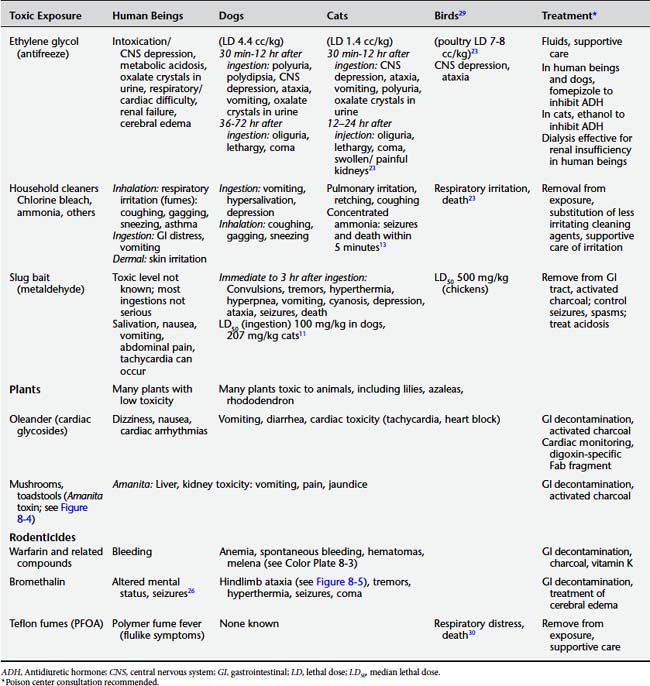
Other Household/Environmental Sources of Acute Toxic Exposures
Ethylene Glycol
Ethylene glycol (EG) toxicosis is relatively common in both human beings and domestic animals, especially dogs and cats. The most common source is antifreeze, which is approximately 95% EG. Its sweet taste is attractive, and EG can be found stored in many households. Exposure is usually by ingestion, although cutaneous exposure has been reported to cause toxicity in cats.22
Acute EG ingestion causes a toxicosis with CNS depression and gastric irritation. EG is metabolized in the liver by enzymes such as alcohol dehydrogenase to metabolites including glycoaldehyde and glyoxylate that can lead to further toxicity, including an anion gap metabolic acidosis, renal failure, and deposition of oxalic acid crystals in the kidney and other tissues.23 Fomepizole (4-methylpyrazole) is an alcohol dehydrogenase inhibitor that is indicated for suspected or confirmed cases of EG (or methanol) toxicity in human beings.24 It is also used in dogs. In cats, fomepizole is ineffective at the canine dosage and ethanol is used. Once renal failure develops in dogs and cats, the prognosis is poor. In contrast, the use of dialysis in human beings is one reason why renal insufficiency in EG poisoning has a relatively good prognosis.
Metaldehyde
Metaldehyde is a bait used to kill slugs, snails, and other garden pests. Baits in pellet form resemble dog food and are flavored with sweeteners such as molasses to attract snails. This can lead to poisoning in dogs, cats, birds, and other wildlife. Human poisoning can also occur, especially in children who accidentally ingest pellets, but such incidents are less common in human beings than in other animals. Human poisonings are usually not serious. Metaldehyde is a neurotoxin and exposure results in vomiting, tachycardia, tremors, seizures, and death.11 Susceptibility varies slightly by species. Treatment involves removal of the agent from the GI tract, use of activated charcoal, and control of medical complications, including seizures and acidosis.
Poisonous Plants
A wide variety of plants used as houseplants or in home landscaping are toxic to human beings and other animals if they are ingested. Exposures to leaves, stems, and berries of poisonous plants are a significant cause of poisoning in animals and can also pose a risk to children. Each year more than 100,000 calls to poison control centers involve plant exposures.25Table 8-6 shows the most common types of plant exposures involved in human poison center calls.
Table 8-6 Top 25 Poisonous Plant Exposures Reported to American Association of Poison Control Centers, 2006
| Botanical (Common) Name | No. |
|---|---|
| Spathiphyllum spp. (peace lily) | 2133 |
| Euphorbia pulcherrima (poinsettia) | 1615 |
| Ilex spp. (holly) | 1572 |
| Philodendron spp. (philodendron) | 1514 |
| Phytolacca americana (American pokeweed) | 1358 |
| Toxicodendron radicans (poison ivy) | 1194 |
| Schlumbergera bridgesii (Christmas cactus) | 705 |
| Ilex opaca (American holly) | 608 |
| Crassula argentea (jade plant) | 604 |
| Plants—cardiac glycosides | 583 |
| Malus spp. (crabapple) | 582 |
| Taraxacum officinale (dandelion) | 581 |
| Pepper mace | 566 |
| Epipremnum aureum (silver vine, money plant) | 566 |
| Plants—cyanogenic glycosides | 555 |
| Plants—pokeweed | 543 |
| Mold | 538 |
| Caladium spp. (elephant ear) | 533 |
| Nandina domestica | 530 |
| Narcissus pseudonarcissus (wild daffodil) | 474 |
| Spinacia oleracea (spinach) | 467 |
| Cactus (unknown type or name) | 460 |
| Rosa spp. (rose) | 450 |
| Quercus spp. (oak) | 447 |
| Hedera helix (common ivy) | 446 |
From Bronstein AC, Spyker DA, Cantilena LR Jr et al: 2006 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS), Clin Toxicol (Phil) 45(8):815-917, 2007.
Most poisonous plant exposures to human beings are non–life-threatening because the quantities ingested by children are usually small. Certain plants, however, have high levels of toxins. An example is poisonous oleander (Nerium oleander) (Color Plate 8-2). The leaves of the oleander plant contain cardiac glycoside chemicals resembling digoxin. The toxicity of oleander in human beings and other animals resembles digoxin toxicity, with GI distress, nausea, and tachycardia and other arrhythmias. Treatment is with the digoxin-specific Fab antibody fragment.25
Ingestion of mushrooms and toadstools is another serious cause of plant poisonings in human beings and animals. The majority of human fatalities and serious dog poisonings as a result of mushroom poisoning involve mushrooms of the genus Amanita that contain Amanita toxin (Figure 8-4). Ingestion by human beings or animals leads to hepatocellular injury and liver and kidney failure. Puppies and children may be at increased risk. Treatment is supportive and involves gastric decontamination and activated charcoal for recent ingestion followed by management of medical complications.
Rodenticides
Rodenticides, used to control rats and mice around dwellings, represent another example of a potent toxic hazard to which animals are more often exposed than human beings. Rodenticides are often placed near places where rodent infestation exists but where pets and wildlife may also have access. The toxic elements in rodenticides are anticoagulants, including warfarin and related compounds, that kill rodents by causing internal bleeding. The symptoms of rodenticide ingestion are bleeding complications, including hematomas (Color Plate 8-3), GI bleeding, hematuria, anemia, and prolongation of the international normalized ratio. Treatment consists of administration of vitamin K to reverse the warfarin effect on the coagulation pathway.
A newer rodenticide agent, bromethalin, is a neurotoxic agent that uncouples oxidative phosphorylation in the mitochondria of the CNS. Animals poisoned with bromethalin develop cerebral edema and neurological signs including ataxia and paralysis (Figure 8-5). Human cases are rare to date, but a fatality has been reported.26 It is anticipated that treatment in human beings will be modeled after treatment in animals, including GI decontamination and treatment of cerebral edema.26
PTFE Fumes
Nonstick cooking pans containing PTFE (Teflon) release fumes (perfluorooctanoic acid [PFOA]) when overheated. These fumes are highly toxic to caged birds, and there are numerous reports of pulmonary hemorrhage and death. A syndrome known as polymer fume fever can develop in human beings exposed to fumes of burning PTFE and Teflon-containing sprays.27,28 Flulike symptoms of fever, chills, and cough have been reported. Treatment for inhalation of PTFE fumes is supportive.
Table 8-7 summarizes the comparative presentation and treatment of common toxic exposures in human beings and other animals. Consultation with a poison control center is recommended for serious acute poisoning exposures.
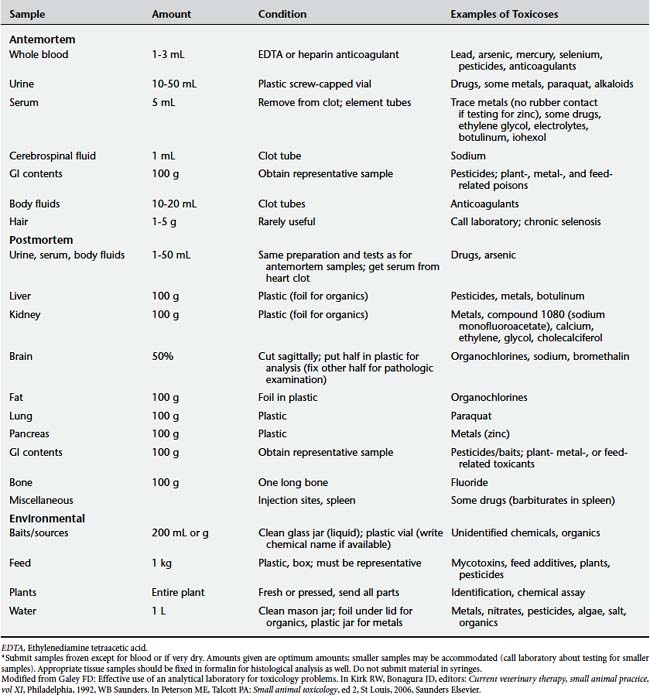
Identification of Exposure
Identification of the toxic exposure can involve checking product labels and searching online or through the distributing company for a copy of the material safety data sheet (MSDS) regarding the suspected chemical exposure (see the Resources section for Web site resources for MSDSs and other toxic hazards). During the medical evaluation of the exposure, specialized toxicologic testing may be indicated. Table 8-8 summarizes analytical toxicologic testing in animals. Similar testing can be performed in human beings.
CHRONIC TOXIC EXPOSURES AND HEALTH EFFECTS
Cancer
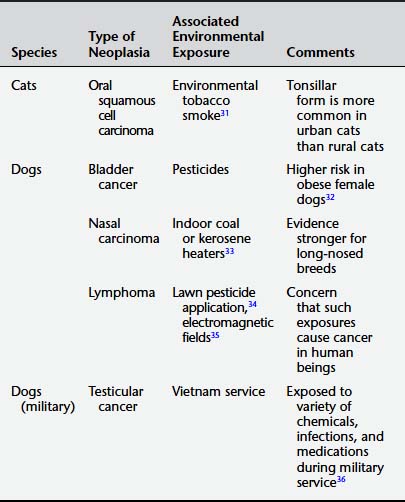
A number of studies have found associations between exposure to chemical and physical hazards and cancer in animals, especially in dogs. Table 8-9 lists some of these reported associations. Many of these associations are based on limited case-control studies or descriptive case reports and remain inconclusive. One obstacle to connecting animal cancers to environmental exposures is the existence of fewer tumor registries for domestic animals compared with human beings. Another is the lack of detailed data on environmental exposures; often data are not obtained for animals diagnosed with cancer. Much remains unknown regarding the linkages between animal risk and human risk of carcinogenesis, including reasons why the most common types and sites of cancer may vary among species and differing biology of particular cancers across species.12 Therefore linking the occurrence of animal cancers to either environmental exposures or human risks remains extremely difficult.
Nevertheless, considering the relationships between human and companion animal cancers may be of both clinical and scientific value. Dogs and human beings are the only animals that naturally develop lethal prostate cancers. Breast cancer in female dogs spreads to bone, just as it does in women. The most frequent tumor in dogs, osteosarcoma, is an important tumor that affects young people. Such observations have led to the development of the field of “comparative oncology.” A growing amount of research is studying similarities and differences between tumors of human beings and domestic animals, and new cancer registries for pet cancers are being established to better understand links between environments and cancers.37 Some studies have attempted to assess human environmental cancer risk by monitoring biomarkers such as lymphocyte micronucleus testing in dogs living near Environmental Protection Agency (EPA) Superfund sites to determine the extent of exposure to mixtures of chemicals that could be carcinogenic.38
Noncancer Outcomes
Just as with cancer, a number of other diseases in animals have been attributed to chronic exposures to toxicants, and there is evidence that animals can serve as sentinels for human beings. Recently an association has been reported between hyperthyroidism in cats and high levels of the flame retardant polybrominated diphenyl ether (PBDE) related to house dust and diet exposures.39 This association is an example of the current scientific controversy regarding the potential of chemicals in the environment to cause alterations in endocrine function (“endocrine disruption”) in animals and possibly human beings.
As previously described, cats were sentinels of methyl mercury poisoning in Minamata, Japan, and the deaths of dogs and horses provided warning of a human health risk from dioxin in oil sprayed for dust control in Times Beach, Missouri. Other examples of animals providing sentinel information about chronic toxic exposures in homes and outdoor environments include horses and deer that develop fluorosis of their bones and teeth while grazing near areas of fluoride-contaminated soil in the vicinity of aluminum smelters and other industrial sources (Figure 8-6).40 In a similar fashion, livestock can develop signs of cadmium toxicity when grazing on cadmium-contaminated soils.41 Dogs have been used to monitor the effects of air pollution on lungs and cardiac function.42Table 8-10 lists some of these reported associations between environmental toxic exposures and noncancer outcomes in animals that have potential sentinel value for human health.
Table 8-10 Noncancer Outcomes in Animals and Implicated Chronic Environmental Exposures
| Species | Type of Disease | Exposure Implicated |
|---|---|---|
| Cat | Hyperthyroidism | Flame-retardant (PBDE) from carpet and furniture43 |
| Mercury poisoning | Fish consumption | |
| Dog | Lung disease | Ambient air pollutants42 |
| Cattle, horses, deer | Fluorosis of bones and teeth | Exposure to fluoride in pastures contaminated from nearby factories |
| Horses, dogs | Sudden death | Exposure to dioxin from contaminated oil used to spray roads, stables8 |
| Cattle | Cadmium-induced renal disease | Cadmium in feed and pastures irrigated with sewage sludge |
WEB RESOURCES
1. U.S. Department of Housing and Urban Development. Healthy Homes Initiative, http://www.hud.gov/offices/lead/hhi/index.cfm. Accessed April 5, 2009
2. Burrell G, Seibert F. Experiments with small animals and carbon monoxide. J Ind Eng Chem. 1914;6(3):241-244.
3. Bukowski JA, Wartenberg D. An alternative approach for investigating the carcinogenicity of indoor air pollution: pets as sentinels of environmental cancer risk. Environ Health Perspect. 1997;105(12):1312-1319.
4. Eto K, Yasutake A, Nakano A, et al. Reappraisal of the historic 1959 cat experiment in Minamata by the Chisso Factory. Tohoku J Exp Med. 2001;194(4):197-203.
5. Thompson ME, Lewin-Smith MR, Kalasinsky VF, et al. Characterization of melamine-containing and calcium oxalate crystals in three dogs with suspected pet food-induced nephrotoxicosis. Vet Pathol. 2008;45(3):417-426.
6. Lattupalli R, Yee J, Kolluru A. Nephrotoxicity of mala fide melamine: modern era milk scandal. Scientific World Journal. 2008;8:949-950.
7. National Research Council. Animals as sentinels of environmental health hazards. Washington DC: National Academies Press, 1991.
8. EPA Superfund Record of Decision. Shenandoah Stables, 2008. http://www.epa.gov/superfund/sites/rods/fulltext/r0790042.pdf. Accessed October 28,
9. Environmental Working Group. Polluted pets: high levels of toxic industrial chemicals contaminate cats and dogs. http://www.ewg.org/book/export/html/26238.
10. Ginsberg G, Toal B. What’s toxic, what’s not. New York: Berkeley Books, 2006.
11. Gupta RC. Veterinary toxicology: basic and clinical principles. New York: Academic Press, 2007.
12. Kelsey JL, Moore AS, Glickman LT. Epidemiologic studies of risk factors for cancer in pet dogs. Epidemiol Rev. 1998;20(2):204-217.
13. Peterson ME, Talcott PA. Small animal toxicology, 2nd ed. St Louis: Saunders Elsevier, 2006.
14. Glickman LT, Domanski LM, MacGuire TG, et al. Mesothelioma in pet dogs with exposure of their owners to asbestos. Environ Res. 1983;32(2):305-313.
15. American Association of Poison Control Centers. Poison Centers Can Help. http://www.aapcc.org/dnn/Home/tabid/36/Default.aspx. Accessed April 5, 2009
16. Bronstein AC, Spyker DA, Cantilena LRJr, et al. 2006 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS). Clin Toxicol (Phila). 2007;45(8):815-917.
17. Khan SA, Schell MM, Trammel HL, et al. Ethylene glycol exposures managed by the ASPCA National Animal Poison Control Center from July 1995 to December 1997. Vet Hum Toxicol. 1999;41(6):403-406.
18. Kupper J, Hellwig B, Demuth D, et al. Computer-based information system (clinitox) for the management of poisoning in small animals [in German]. Schweiz Archiv Tierheilkd. 2004;146(3):127-134.
19. Burgat V, Keck G, Guerre P, et al. Glyphosate toxicosis in domestic animals: a survey from the data of the Centre National d’Informations Toxicologiques Veterinaires (CNITV). Vet Hum Toxicol. 1998;40(6):363-367.
20. Cope RB, White KS, More E, et al. Exposure-to-treatment interval and clinical severity in canine poisoning: a retrospective analysis at a Portland veterinary emergency center. J Vet Pharmacol Ther. 2006;29(3):233-236.
21. Hornfeldt CS, Murphy MJ. American Association of Poison Control Centers report on poisonings of animals, 1993–1994. J Am Vet Med Assoc. 1998;212(3):358-361.
22. Kahn CM, Line S. The Merck veterinary manual, 9th ed. Whitehouse Station, NJ: Merck, 2005.
23. Ford MD, Delaney KA, Ling L, et al. Clinical toxicology. Philadelphia: Saunders, 2001.
24. Holstege CP, Dobmeier SG, Bechtel LK. Critical care toxicology. Emerg Med Clin North Am. 2008;26(3):715-739. viii–ix
25. Froberg B, Ibrahim D, Furbee RB. Plant poisoning. Emerg Med Clin North Am. 2007;25(2):375-433.
26. Pasquale-Styles MA, Sochaski MA, Dorman DC, et al. Fatal bromethalin poisoning. J Forensic Sci. 2006;51(5):1154-1157.
27. Patel MM, Miller MA, Chomchai S. Polymer fume fever after use of a household product. Am J Emerg Med. 2006;24(7):880-881.
28. Son M, Maruyama E, Shindo Y, et al. Case of polymer fume fever with interstitial pneumonia caused by inhalation of polytetrafluoroethylene (Teflon) [in Japanese]. Chudoku Kenkyu. 2006;19(3):279-282.
29. Animal Forum. Animal poison control center offers pet poison safety tips for bird owners, http://www.animalforum.com/birdpoison.htm Accessed April 5 2009
30. Stoltz JH, Galey F, Johnson B. Sudden death in ten psittacine birds associated with the operation of a self-cleaning oven. Vet Hum Toxicol. 1992;34(5):420-421.
31. Snyder LA, Bertone ER, Jakowski RM, et al. P53 expression and environmental tobacco smoke exposure in feline oral squamous cell carcinoma. Vet Pathol. 2004;41(3):209-214.
32. Glickman LT, Raghavan M, Knapp DW, et al. Herbicide exposure and the risk of transitional cell carcinoma of the urinary bladder in Scottish Terriers. J Am Vet Med Assoc. 2004;224(8):1290-1297.
33. Bukowski JA, Wartenberg D, Goldschmidt M. Environmental causes for sinonasal cancers in pet dogs, and their usefulness as sentinels of indoor cancer risk. J Toxicol Environ Health A. 1998;54(7):579-591.
34. Hayes HM, Tarone RE, Cantor KP, et al. Case control study of canine malignant lymphoma: positive association with dog owner’s use of 2,4-dichlorophenoxyacetic acid herbicides. J Natl Cancer Inst. 1991;83(17):1226-1231.
35. Reif JS, Lower KS, Ogilvie GK. Residential exposure to magnetic fields and risk of canine lymphoma. Am J Epidemiol. 1995;141(4):352-359.
36. Hayes HM, Tyrone RE, Casey HW. Excess of seminoma observed in Vietnam service U.S. military working dogs. J Natl Cancer Inst. 1990;82(12):1042-1046.
37. Waters DJ, Wildasin K. Cancer clues from pet dogs. Sci Am. 2006;295(6):94-101.
38. Backer LC, Grindem CB, Corbett WT, et al. Pet dogs as sentinels for environmental contamination. Sci Total Environ. 2001;274(1–3):161-169.
39. Dye JA, Venier M, Zhu L, et al. Elevated PBDE levels in pet cats: sentinels for humans? Environ Sci Technol. 2007;41(18):6350-6356.
40. Vikoren T, Stuve G. Fluoride exposure in cervids inhabiting areas adjacent to aluminum smelters in Norway. II. Fluorosis. J Wildl Dis. 1996;32(2):181-189.
41. Kessels BG, Wensing T, Wentink GH, et al. Clinical, chemical, and hematological parameters in cattle kept in a cadmium-contaminated area. Bull Environ Contam Toxicol. 1990;44(2):339-344.
42. Calderon-Garciduenas L, Mora-Tiscareno A, Fordham LA, et al. Canines as sentinel species for assessing chronic exposures to air pollutants: part 1. Respiratory pathology. Toxicol Sci. 2001;61(2):342-355.
43. American Chemical Society. Cat disease linked to flame retardants in furniture and to pet food. ScienceDaily. 2009. Accessed February 3, http://www.sciencedaily.com/releases/2007/08/070815122354.htm.
CARBON MONOXIDE
(ICD-10 T58.0 Toxic Effect of Carbon Monoxide)
Carbon monoxide (CO) is the most common cause of poisoning-related death.1 Each year in the United States, several thousand individuals die or are hospitalized with CO poisoning related to smoke inhalation, and more than 400 deaths each year are attributed to non–fire-related accidental CO poisoning.2 Because the gas has no warning odor or color and the symptoms are often subtle and nonspecific, the true incidence of CO poisoning in human beings may be much higher. In fact, CO has been termed the “unnoticed poison of the twenty-first century.”3 CO is an example of a toxicant for which companion animals could provide early warning of human exposure risk. However, it is likely that just as in human beings, the diagnosis is often overlooked. The classic animal sentinel for CO poisoning is the canary. Canaries were brought into mines in the United States and Great Britain in the first half of the twentieth century to provide early warning to miners of CO and other toxic gases. Canaries were chosen after experiments on this species, as well as guinea pigs, rabbits, chickens, dogs, mice, and pigeons, revealed that either canaries or mice were most suitable, with canaries more sensitive than mice to the effects of CO.4 Canaries developed recognizable signs of toxicosis sufficiently early to allow the miners to take preventive steps to avoid further exposure. In the home setting as well, dogs and cats may sometimes serve as sentinels. Human cases of CO poisoning have been detected because the family dog and family members were displaying signs of intoxication.5 Additionally, the 2007 ASPCA Cat of the Year award was given to a 2-year-old domestic short-hair cat that scratched at her sleeping owner’s face to arouse her and save her from death from CO intoxication.6
Key Points for Clinicians and Public Health Professionals
Public Health Professionals
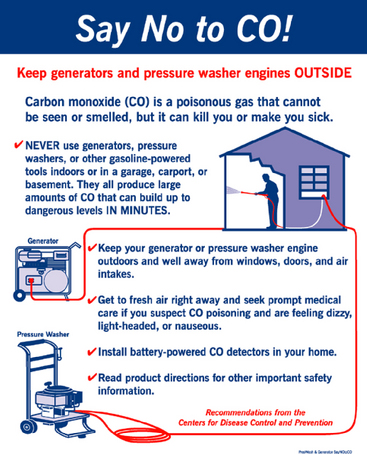
BOX 8-1 You Can Prevent Carbon Monoxide Exposure
Modified from Centers for Disease Control and Prevention: Carbon monoxide poisoning: prevention guidelines. http://www.cdc.gov/co/guidelines.htm.
Human Health Clinicians
Veterinary Clinicians
AGENT
CO is an odorless, colorless, nonirritating gas that is produced by the incomplete combustion of fuels. Common sources include malfunctioning and improperly vented heating furnaces, automobile exhaust, and propane-powered equipment such as forklifts, generators, space heaters, and floor polishers (Figure 8-7).8 CO is also a component of air pollution, leading to population-wide low-level exposures. CO is slightly lighter than air, so it tends to rise through a building.
ROUTES OF EXPOSURE AND METABOLIC FATE
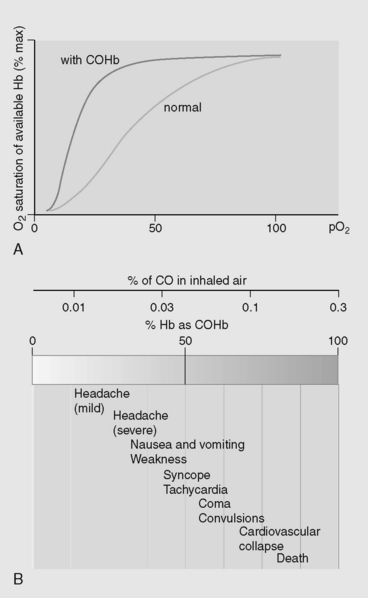
The primary route of CO exposure is inhalation. Levels of CO in ambient air are usually less than 10 ppm but may be higher in urban areas. The Occupational Safety and Health Administration (OSHA)-permissible exposure level for CO exposures in the workplace is 50 ppm. After a gas stove is used for cooking, nearby air levels may exceed 100 ppm.1 CO inhaled into the lungs binds tightly to hemoglobin in red blood cells (RBCs) to form carboxyhemoglobin (COHb). This process displaces oxygen from the hemoglobin-binding sites because it binds to hemoglobin more than 200 times more avidly than oxygen.3 This reduces the oxygen-carrying capacity of the bloodstream, causing tissue hypoxia, particularly of the heart and brain. COHb is bright red in color, which is why tissues of a CO-poisoned individual may be “cherry red.” The half-life of COHb in the human bloodstream is approximately 4 to 5 hours when the person is breathing room air. However, if 100% oxygen is administered, the half-life has been reported to shorten to 47 to 80 minutes9 and is even shorter in a hyperbaric oxygen environment.
The level of COHb in the blood helps determine the degree of toxicity. Smokers may have chronically elevated levels around 7% to 12%. Normal levels in nonsmokers are generally less than 2%.10
GROUPS AT RISK
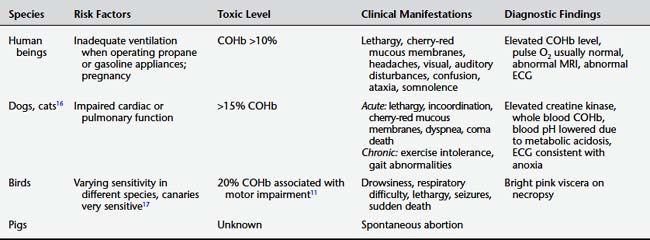
Pets such as dogs may be at increased exposure risk relative to human beings because of their faster breathing rate and smaller volume of distribution. Birds have increased susceptibility relative to human beings because of their efficient gas exchange and higher mass-specific ventilation of tissues.11 Pregnant animals and pets with underlying cardiac disease are at increased risk.
TOXICITY IN HUMAN BEINGS
CO can produce both acute and chronic effects (Figures 8-8 and 8-9).3 Because of their high metabolic activity and oxygen demand, the brain and heart are the organs most affected by exposure. Low-level chronic exposure, as from a slowly leaking furnace, can cause headaches, fatigue, malaise, dizziness, chest pain, and abdominal pain. These nonspecific symptoms can easily be attributed to other causes, and the diagnosis may therefore be overlooked. Elevations in the COHb level to between 5% and 20% may be associated with subtle changes such as headache and behavioral changes. Chronic exposures are believed to predispose human beings to the development of cardiovascular disease and memory loss.
Acute, high-level exposure with COHb levels greater than 20% produces symptoms as described above, as well as ataxia, confusion, slurred speech, disturbances of visual or auditory function and, with increasing intoxication, eventual loss of consciousness. If exposure continues, death can result from respiratory arrest (Color Plate 8-4). The skin color of CO-poisoned individuals usually is normal. The pulse oximetry reading can be falsely elevated because conventional oximeters cannot distinguish between oxyhemoglobin and COHb. There may be electrocardiographic abnormalities including arrhythmias and ischemia. Magnetic resonance imaging (MRI) of the brain may show white matter high-signal intensities resulting from impaired diffusion.3 Low-attenuation lesions in the globus pallidum have been reported.
TOXICITY IN ANIMALS
Dogs appear to be more resistant to COHb than human beings.13 Acute signs include lethargy, incoordination, cherry-red mucous membranes, dyspnea, coma, and death. Tachycardia has been reported in dogs at levels of 15% COHb.14 Chronic exposure in dogs and cats can manifest as decreased exercise tolerance and gait problems.
Birds exhibit drowsiness, difficulty breathing, weakness, ataxia, and seizures.11 Chickens may become exposed in enclosed facilities and during transport in trucks. This can result in high mortality rates, with bright pink coloration of the viscera at necropsy.15 Spontaneous abortion has been noted in sows that have experienced CO intoxication.12Table 8-11 shows key aspects of CO toxicity in human beings and other animals.
DIAGNOSIS
Measurement of air levels of CO in the area where the exposure occurred should also be done as soon as possible. Many fire departments or public health departments are able to obtain such measurements. Although CO standards have yet to be set for indoor air, the U.S. National Ambient Air Quality Standards are 9 ppm for 8 hours and 35 ppm for 1 hour for outdoor air.18
MANAGEMENT OF CO POISONING
Treatment in Human Beings
The principal approach to management of acute CO poisoning is to remove the patient from exposure, ensure adequate oxygenation, and eliminate COHb from the body (Figure 8-10). All patients should receive 100% oxygen. Patients with significant symptoms (such as loss of consciousness with or without neurological deficits) levels of COHb greater than 25% and all pregnant patients are candidates for hyperbaric oxygen therapy, but hyperbaric oxygen therapy should be considered on a case-by case-basis in all patients in consultation with a bariatric medicine specialist.
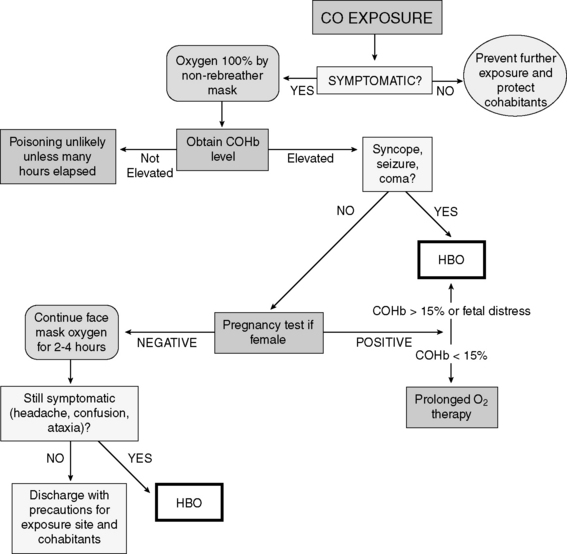
Figure 8-10 Suggested algorithm for the management of carbon monoxide poisoning.
(From Ford MD, Delaney KA, Ling L et al: Clinical toxicology, Philadelphia, 2001, Saunders.) HBO, Hyperbaric oxygen.
1. Kao LW, Nanagas KA. Toxicity associated with carbon monoxide. Clin Lab Med. 2006;26(1):99-125.
2. Centers for Disease Control and Prevention (CDC). Carbon monoxide-related deaths, United States, 1999–2004. MMWR. 2007;56(50):1309-1312.
3. Prockop LD, Chichkova RI. Carbon monoxide intoxication: an updated review. J Neurol Sci. 262(1–2):122–130.
4. Burrell GA. Relative effects of carbon monoxide on small animals. United States Bureau of Mines, 1914.
5. The Boston Channel. Dog helps alert family to carbon monoxide poisoning, 2005. Viewed December 5,
6. Associated Press. Life-saving dog, cat honored for heroic acts: pets feted by ASPCA after rescuing their masters., http://www.msnbc.msn.com/id/21595558/. Accessed November 2, 2007
7. Klein J. All clear: laws, codes expanding to help prevent carbon monoxide tragedies. Occup Health Saf. 2007;76(5):82-84.
8. Washington State Department of Labor and Industries. Carbon monoxide. http://www.lni.wa.gov/Safety/Topics/AtoZ/CarbonMonoxide/default.asp Accessed August 15, 2008
9. Ford MD, Delaney KA, Ling L, et al. Clinical toxicology. Philadelphia: Saunders, 2001.
10. Rosenstock L, Cullen M, Brodkin C, et al. Textbook of clinical occupational and environmental medicine, 2nd ed. Edinburgh: Saunders, 2004.
11. Gupta RC. Veterinary toxicology: basic and clinical principles. New York: Academic Press, 2007.
12. Pejsak Z, Zmudzki J, Wojnicki P. Abortion in sows associated with carbon monoxide intoxication. Vet Rec. 2008;162(13):417.
13. Penney DG. Hemodynamic response to carbon monoxide. Environ Health Perspect. 1988;77:121-130.
14. Farber JP, Schwartz PJ, Vanoli E, et al. Carbon monoxide and lethal arrhythmias. Res Rep Health Eff Inst. 1990(36):1-17. discussion 19–27
15. Kahn CM, Line S. The Merck veterinary manual, 9th ed. Whitehouse Station, NJ: Merck, 2005.
16. Hipwell F. Suspected carbon monoxide poisoning in a dog. Vet Rec. 1995;136(11):275-276.
17. Brown RE, Brain JD, Wang N. The avian respiratory system: a unique model for studies of respiratory toxicosis and for monitoring air quality. Environ Health Perspect. 1997;105(2):188-200.
18. United States Environmental Protection Agency. Carbon monoxide., 2008. http://www.epa.gov/iaq/co.html. Accessed June 1,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree