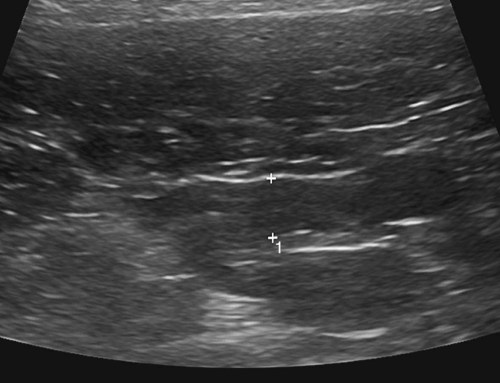
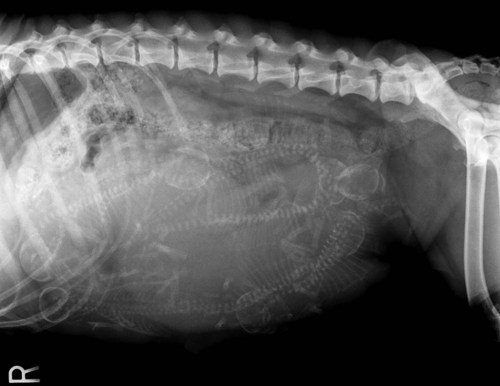
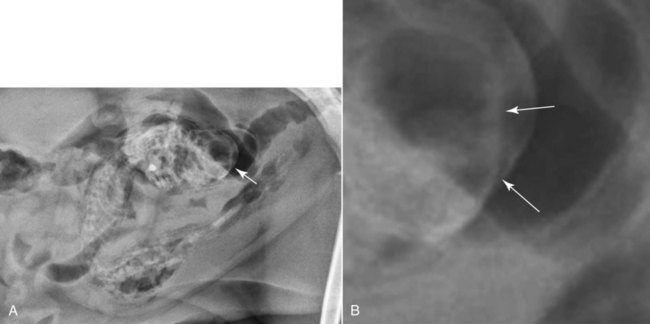
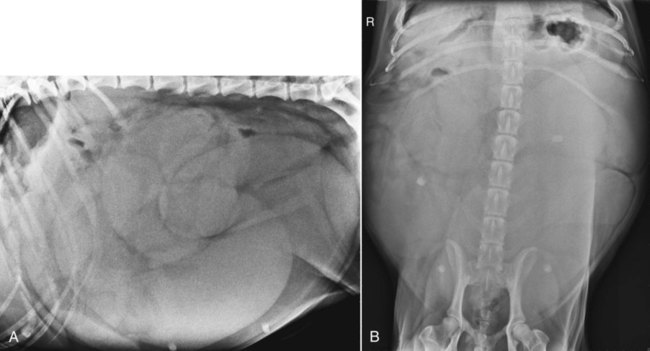
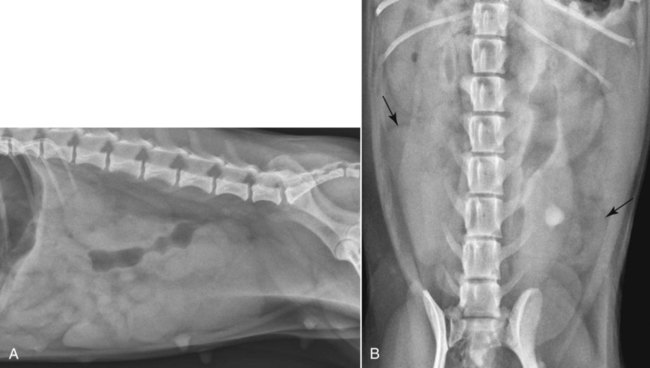
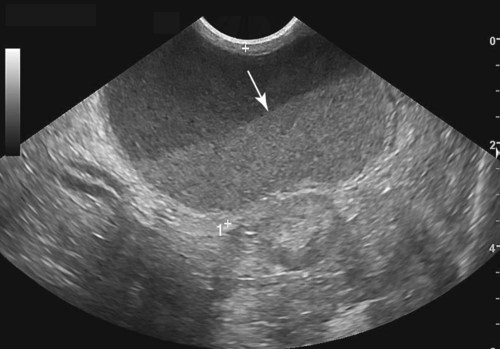
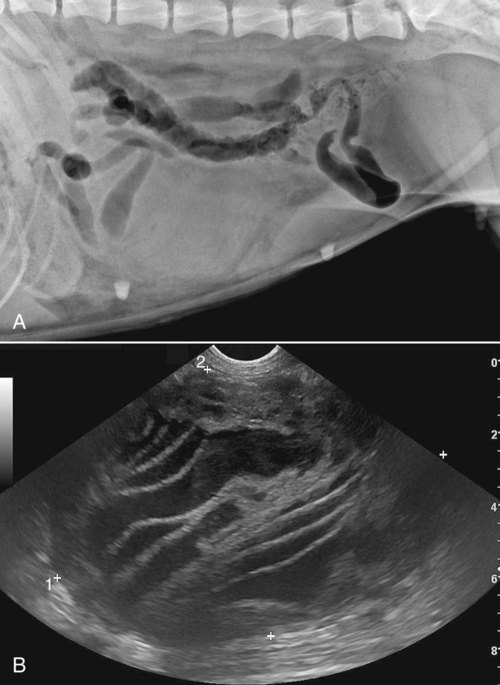
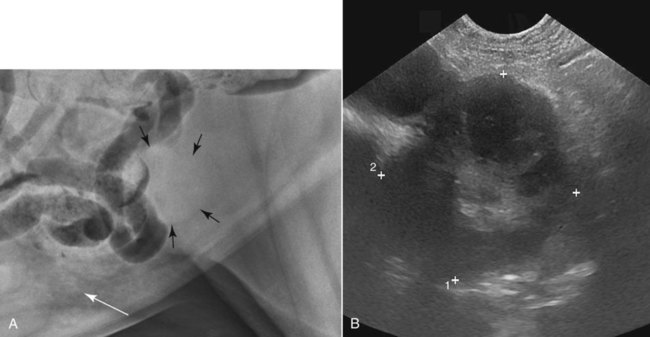
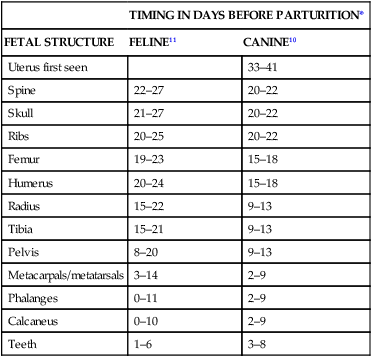
Radiographic visualization of the uterus is limited by image contrast as well as uterine size. Radiographic technique, as for all abdominal imaging, should maximize radiographic contrast. Compression radiography can increase visualization of a mildly enlarged uterus by increasing separation of the uterus from the bladder, colon, and overlying small intestine and by reducing thickness, which will decrease scatter radiation.1 Use of a radiolucent paddle is the most commonly employed technique. The effectiveness of compression radiography is reduced by conformation and obesity in addition to gastrointestinal contents and bladder distention. Where there is indication for elective radiography of the uterus, patient preparation is recommended to increase visualization; a 24-hour fast and enema administration will reduce gastrointestinal superimposition. The uterine body can be located most easily by scanning between the bladder and caudal aspect of the descending colon with the patient in dorsal or lateral recumbency. It appears as a tubular echogenic structure, similar in size to a loop of intestine. It is differentiated from intestine by location and absence of distinct wall layering. A distended urinary bladder acts as an acoustic window to improve imaging of the uterus. The uterine body is smaller in diameter than the cervix, which is visualized caudally as a hyperechoic linear structure.2 The endometrium of the uterine body and horns should be uniform in echogenicity and smoothly marginated (Fig. 42-1). Wall thickness depends on the stage of the estrus cycle. The uterine lumen is not seen typically. If present, intraluminal mucus appears as a hyperechoic central area. In anestrus, the uterine wall is thinnest with no fluid present. A small amount of hypoechoic to anechoic fluid can be present during proestrus and estrus when the endometrium is thickened mildly. During diestrus the endometrium is thickened further because of progesterone-driven glandular hyperplasia. The uterine horns can be traced forward from the bifurcation on each side and they terminate a short distance from the ovary. A normal uterine stump can be visualized occasionally in neutered females, dependent on the length of uterine body removed. Interrogation of this most caudal region of the uterus is important in evaluating for stump pyometra. Palpation likely remains the most common method of pregnancy detection in the bitch, being fairly accurate around 24 to 35 days.3 Ultrasound improves accuracy, allows earlier pregnancy detection, and can be used to evaluate litter size. Definitive sonographic diagnosis of pregnancy can be made in the queen at 15 to 17 days gestation when the chorionic vesicle becomes visible.2 In the bitch, this occurs at 18 to 20 days.4 However, definitive conformation is easier when cardiac motion can be detected after 23 days. Prediction of the timing of parturition is one of the primary reasons for imaging the gravid uterus. The normal gestation length in both dogs and cats is approximately 63 to 66 days. Ultrasonographically, chorionic vesicle diameter, crown rump length, head diameter (biparietal diameter), and body diameter measurements can be used to predict the age of the fetus. Using established growth curves,5 inner chorionic cavity diameter in early gestation, from 18 to 40 days, and biparietal diameter in late gestation are equally accurate predictors of age with approximately 85% of litters likely to be whelped within 2 days of the predicted parturition date using these methods.6 The timing of organ development is also a reliable indicator of fetal age.7 Cardiac motion can be detected consistently from 23 to 25 days, and limb buds and an echogenic fetal skeleton can be identified by day 35 in the dog.4,8 Fetal movement can also be detected from this time.4,9 Radiographic diagnosis of pregnancy is possible after fetal mineralization, which occurs from 43 days in the dog10 and 38 days (25 to 29 days before parturition) in the cat.11 Radiographs obtained late in pregnancy may also be used to predict impending parturition. In cats, fetal mineralization occurs first at 25 to 29 days before parturition11 and in dogs at 20 to 22 days before parturition.10 Table 42-1 shows the radiographic mineralization of fetal structures that can be used to predict parturition. Table • 42-1 Approximate Timing of Mineralization of Fetal Structures in Dogs and Cats *The timings are given as the number of days before parturition. Imaging is also used to predict litter size, for which radiography is more accurate than ultrasonography. Best sonographic estimates of litter size are achieved in early to midgestation,7 whereas radiographic evaluation can be made after fetal mineralization. Radiographic estimates of litter size are best made by counting the number of skulls and spines (Fig. 42-2). Superimposition of fetuses will make accurate radiographic determination of fetal number challenging with large litters, and orthogonal views are always indicated. Radiographic estimations of litter size are more easily achieved at later stages of mineralization. Sonographically, the number of vesicles in early pregnancy or fetal heads in later gestation may be counted. Fetal resorption is relatively common, and evaluation in early pregnancy may therefore provide an overestimate of litter size. Prediction of litter size with an associated error of plus or minus one fetus may be possible sonographically in up to 89.5% of dogs.7 Sonographic evaluation of fetal heartbeat is the most reliable method of fetal viability. Fetal demise is characterized by loss of the heartbeat. With increasing time after death, fetal structures become progressively less recognizable. Early embryonic resorption can also be documented sonographically with a characteristic appearance of echogenic particles within the yolk sac, progressive loss of fluid volume, and hypoechogenicity of the adjacent uterus in addition to eventual loss of the fetal heartbeat and blurring of the fetal margins.8 Delayed embryonic development is a good predictor for embryonic resorption.8 Radiographic signs of fetal demise occur later, at least 24 hours after death, and are less reliable than sonographic indicators. The presence of gas within or around the fetus, overlapping of the bones of the cranium, a tightly curled fetus, and collapse of the fetal skeleton may be evident (Fig. 42-3). The presence of delayed development of a fetus relative to litter mates is also an indication of demise. Dystocia can occur through maternal or fetal causes. Several of these, such as uterine inertia, are undetectable radiographically. However, dystocia caused by fetal malposition, fetomaternal disproportion, or anatomic abnormality of the pelvic canal can be detected radiographically. Lateral and ventrodorsal views are recommended in dystocia patients where any of these are suspected. Fetal malposition is rarely a major problem in species that have large litter sizes. However, caudal, breech, lateral, or downward deviation of the head and transverse presentation (Fig. 42-4, A) can lead to obstruction within the pelvic canal. Occasionally, two fetuses will present simultaneously from each horn, which can also lead to dystocia. Fetomaternal disproportion is difficult to determine accurately. It generally occurs if the bitch has been bred by a much larger breed, if there is a single large fetus (Fig. 42-4, B), or in brachycephalic breeds where the head is large and the maternal pelvis flattened. If the skull or shoulders are wider on the ventrodorsal view than the pelvic canal, disproportion is the likely cause of dystocia. Abnormalities of the pelvic canal are most often traumatic in origin. Healed fractures can lead to pelvic canal narrowing in both canine and feline patients, preventing normal delivery. In breeding animals with a known history of trauma, prebreeding radiographs may be indicated to determine the likelihood of complication. Radiographs can also be used after whelping if there is clinical concern that a retained fetus may be present. Anomalous lesions of the uterus are rare, occurring in less than 0.1% of canine and feline patients undergoing ovariohysterectomy.12 Uterus unicornis, uterine horn aplasia, and uterine horn hypoplasia are reported. Segmental aplasia, with absence of a uterine body resulting in dilated fluid-filled uterine horns, has also been described.13 Renal agenesis is common in association with uterine anomalies,12 and in some patients, this will be the only abnormality recognized radiographically. Fluid accumulation occurs commonly in the affected horn proximal to the occlusion and may be visible sonographically or, in some instances, radiographically. Clinically, the majority of uterine anomalies will be incidental unless they are the cause of unsuccessful attempts to breed or if pyometra develops. Cystic endometrial hyperplasia-pyometra complex is the most common uterine disorder in bitches. Cystic endometrial hyperplasia occurs as a result of an abnormal response of the endometrium to progesterone during the luteal phase of the cycle. Fluid accumulates in the endometrial glands and lumen of the uterus, and pyometra results if bacteria are present. Mucometra or hydrometra occur if the uterus becomes distended with mucus but remains sterile; these patients are often asymptomatic. The uterine enlargement associated with chronic endometrial hyperplasia is not recognized radiographically. Pyometra and mucometra or hydrometra result in generalized uterine distention, the degree of which will depend on patency of the cervix. Radiographically, the typical appearance of uterine enlargement is of a soft tissue tubular structure within the caudal and ventral aspects of the abdomen (Figs. 42-5, A and B, and 42-6, A and B). On lateral views, enlargement of the uterine body is seen characteristically as a soft tissue structure between the bladder and colon. However, this is not always easy to identify; a lateral compression radiograph may facilitate identification of enlargement of the uterine body. Enlargement of the uterine horns leads to tubular structures of homogeneous opacity in the caudal and ventral aspects of the abdomen. In early enlargement, it may not be possible to differentiate the enlarged uterine horns from jejunum. On the ventrodorsal view, the enlarged uterus will appear as a soft tissue tubular structure lateral to the descending colon on the left and along the peripheral abdominal wall on the right. Ultrasonographically, cystic endometrial hyperplasia results in endometrial thickening with multifocal anechoic dilated cystic glands and glandular ducts. Fluid accumulation within the uterine lumen is not definitive for pyometra, because both mucometra and hydrometra can have this appearance, although they can progress to pyometra. Increasing cellularity from infection results in more echogenic fluid (Fig. 42-7). Increased serum progesterone levels, indicating diestrus, can be used to support a diagnosis of pyometra. Rarely, infection of the uterus can occur for etiologies other than progesterone-related disease. Infection postwhelping or after caesarian section are possible (Fig. 42-8). Following ovariohysterectomy, the uterine stump and cervix is accessible sonographically by imaging lateral to the caudal aspect of the urinary bladder. The uterine stump will rarely be visualized sonographically when normal. Progesterone-related stump pyometra can occur only if the ovaries have been left in situ, permitting ongoing estrus cycling (Fig. 42-9, A and B). However, stump granuloma and abscessation can occur secondary to local inflammation and infection independent of the presence of progesterone and can occur as a reaction to nonabsorbable suture material. The sonographic appearance of granuloma is of a focal echogenic mass, typically mildly heterogeneous, adjacent to the bladder neck. A stump hematoma occurs most often as a consequence of surgery and may be associated with underlying coagulopathy. The early sonographic appearance is of an echogenic fluid-filled structure that becomes progressively solid in appearance and will eventually decrease in size.
The Uterus, Ovaries, and Testes
Uterus
Imaging Procedures and Normal Imaging Findings
Survey Radiographs
Ultrasound
Pregnancy
Normal Imaging Findings in Pregnancy
TIMING IN DAYS BEFORE PARTURITION*
FETAL STRUCTURE
FELINE11
CANINE10
Uterus first seen
33–41
Spine
22–27
20–22
Skull
21–27
20–22
Ribs
20–25
20–22
Femur
19–23
15–18
Humerus
20–24
15–18
Radius
15–22
9–13
Tibia
15–21
9–13
Pelvis
8–20
9–13
Metacarpals/metatarsals
3–14
2–9
Phalanges
0–11
2–9
Calcaneus
0–10
2–9
Teeth
1–6
3–8
Abnormal Imaging Findings in Pregnancy
Fetal Demise
Dystocia
Abnormal Imaging Findings in Uterine Disease
Uterine Anomalies
Cystic Endometrial Hyperplasia and Pyometra
Uterine Stump Disease