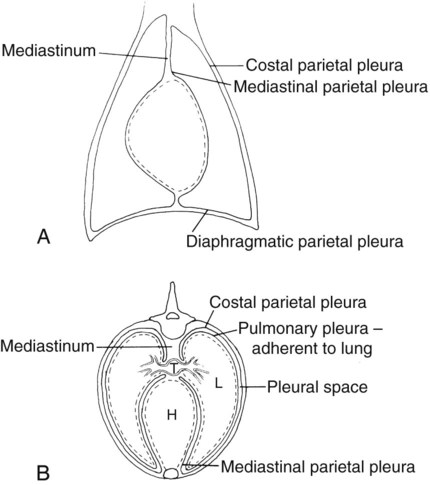
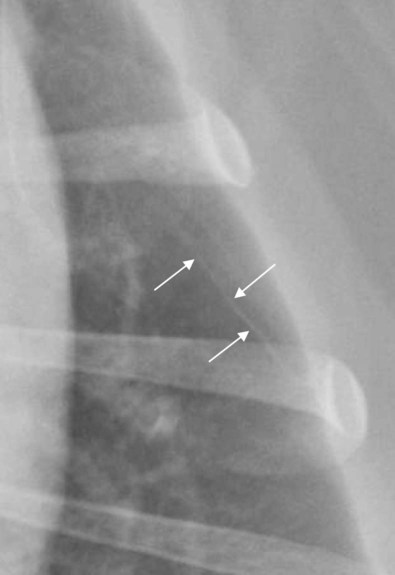
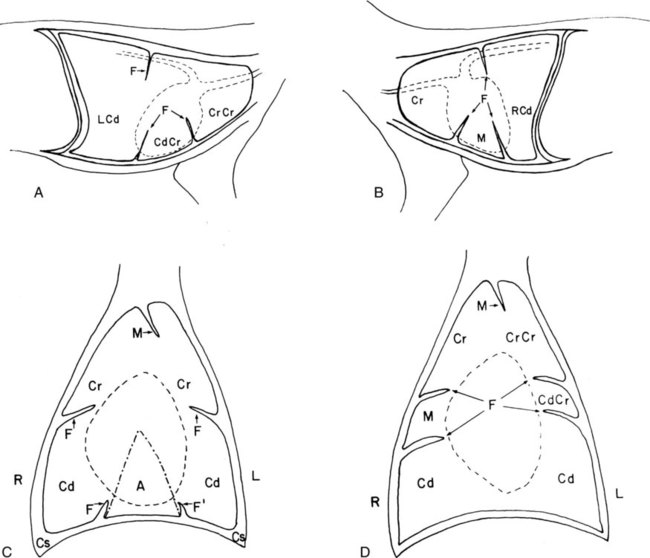
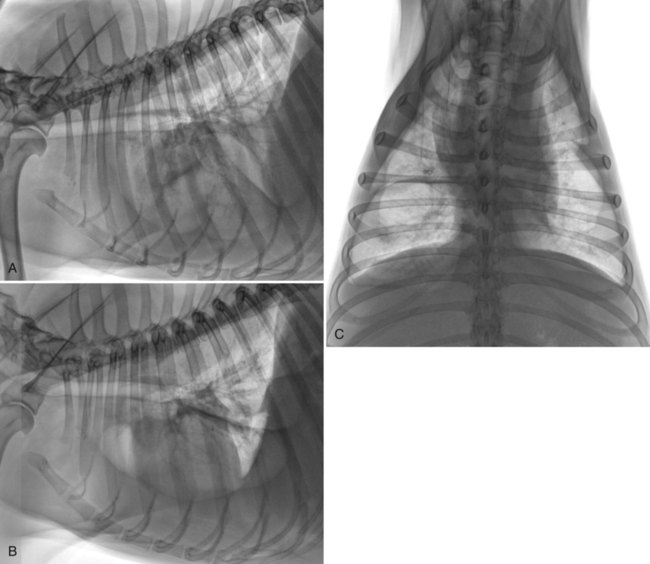
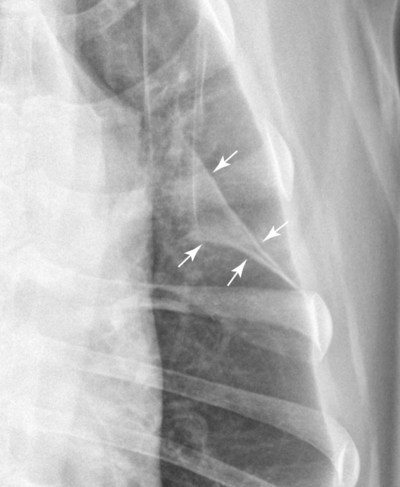
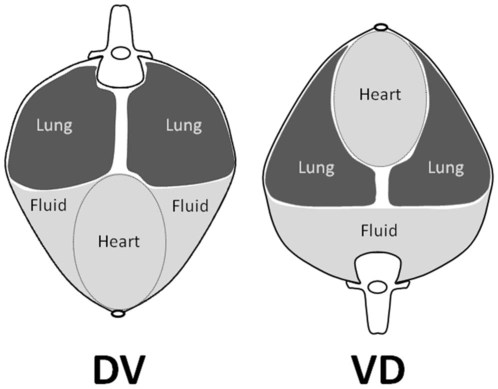
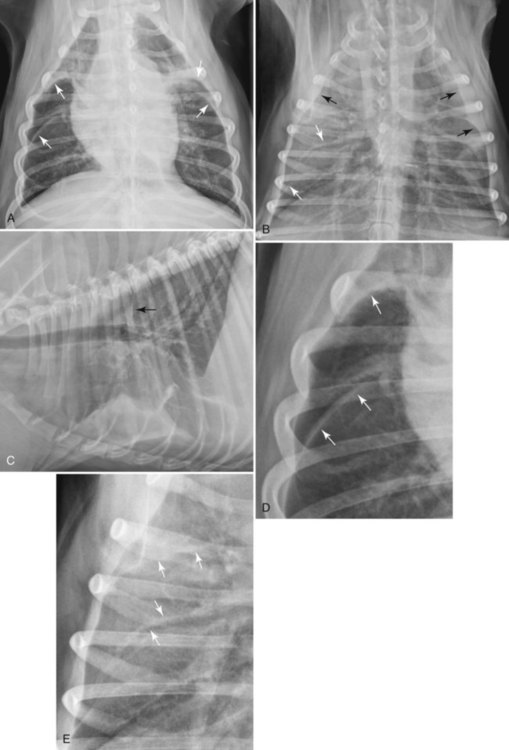
As described in Chapter 30, there are two pleural sacs, one on the right and one on the left. Each pleural sac has parietal (mediastinal, diaphragmatic, costal) and visceral components. The visceral pleura covers the lung parenchyma. Of the parietal pleural layers, costal parietal pleura lines the inside of the thoracic cage, diaphragmatic parietal pleura covers the diaphragm, and mediastinal parietal pleura forms the boundaries of the mediastinal space, dividing the thorax into left and right halves. The left and right pleural sacs are distinct entities (Fig. 31-1; see also Figs. 30-1 and 30-2). The pleural space is a potential space in normal subjects. It lies between the costal parietal pleura and visceral pleura, between the diaphragmatic parietal pleura and visceral pleura, and between the mediastinal parietal pleura and visceral pleura. The pleural space also lies between visceral pleural layers in interlobar fissures. The normal pleural space is a potential space because it contains only a small volume of fluid, which serves as a lubricant, but it can become a real space if it contains air, tissue, or an increased volume of fluid. Normal pleura is usually not visible radiographically. Pleura is very thin and also silhouettes with adjacent soft tissue everywhere except in interlobar fissures, where it is in contact only with lung. Thin pleural lines between lobes are sometimes visible radiographically. These thin pleural lines may be because of the x-ray beam striking normal interlobar pleura exactly head-on, resulting in absorption of a sufficient number of x-rays for the pleura to be seen, or to slightly thickened pleura (Fig. 31-2). Radiographic determination of whether isolated, thin pleural lines are normal or are caused by mild thickening is impossible. In either instance, this finding is usually of no clinical significance. When pleural thickening is advanced, wider pleural lines between lung lobes may be seen (Fig. 31-3). With pleural fibrosis, the specific interlobar fissures seen radiographically depend on which fissures are struck tangentially by the x-ray beam. This varies with the position of the patient relative to the x-ray beam. Fluid in the pleural space can be an exudate, transudate, or modified transudate and can result from many causes (Table 31-1). The radiographic changes associated with pleural fluid depend on the volume of fluid, the position of the animal in relation to the x-ray beam, the distribution of the fluid, and whether the fluid is free or loculated. There are no radiographic criteria that allow differentiation of an exudate from a transudate. Thus, the radiographic changes associated with pleural fluid are the same, regardless of fluid type, because neither the distribution of pleural fluid nor its opacity is reliably related to the cause, although an exudate may be more asymmetrically distributed. This is discussed in more detail later. Table • 31-1 E, Exudate; M, modified transudate; T, transudate. Pleural fluid distributes itself according to gravity and the ability of the lung to expand—that is, lung compliance.1 It is important to realize that the radiographic appearance of pleural fluid in ventrodorsal (VD) versus dorsoventral (DV) radiographs can be quite different. In DV radiographs, fluid gravitates ventrally and causes border effacement of the heart. In VD radiographs, pleural fluid usually does not obscure the heart because the fluid is in the dorsal aspect of the thorax, where it does not make contact with the heart and cause border effacement (Fig. 31-4). Also, the overall opacity of the thorax will be greater in DV radiographs in patients with pleural fluid because the fluid depth is greater (see Fig. 31-4). Radiographic signs of free pleural fluid are listed in Box 31-1. The thickness and number of interlobar fissures seen with pleural fluid depend on the amount of fluid and the relative position of the patient and the x-ray beam (Fig. 31-5, p. 574). Approximately 100 mL of fluid must be present in the pleural space of a medium-sized dog before widened interlobar fissures become visible.2 Thus, any radiographic evidence of pleural fluid signifies a relatively large fluid volume, and one that can be sampled by thoracocentesis. Visualization of fluid-containing interlobar fissures results when the x-ray beam strikes the fissure head-on. Some fluid-containing fissures may not be seen because their relation to the x-ray beam is not head-on. With a small amount of fluid, interlobar fissures are more likely to be seen on VD rather than DV radiographs because when in dorsal recumbency there is a tendency for fluid to enter interlobar fissures (see Fig. 31-3). This is opposed to sternal recumbency where the fluid collects dorsal to the sternum.2,3 A small amount of pleural fluid also usually results in visualization of interlobar fissures in lateral views as well. With moderate or pronounced pleural fluid, the number and thickness of interlobar fissures increase, and fluid also collects between the thoracic wall and the lung, resulting in lung retraction (Figs. 31-6 and 31-7, p. 576).
The Pleural Space
Pleural Anatomy
Normal Radiographic Appearance of Pleura and Pleural Thickening
Pleural Fluid
CAUSE
FLUID TYPE
Congestive heart failure
M
Pyothorax
E
Malignancy
M
Pneumonia
M, E
Trauma
M
Coagulation defect
M
Hypoproteinemia
T
Mediastinitis
M, E
Chylothorax
M
Diaphragmatic hernia
M
Interlobar Fissures, Retraction of Lung Margins, and Retrosternal Opacification
The Pleural Space