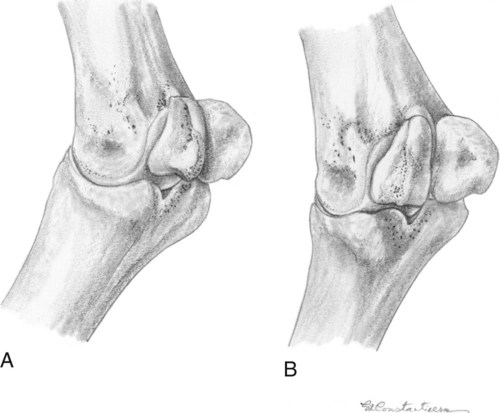
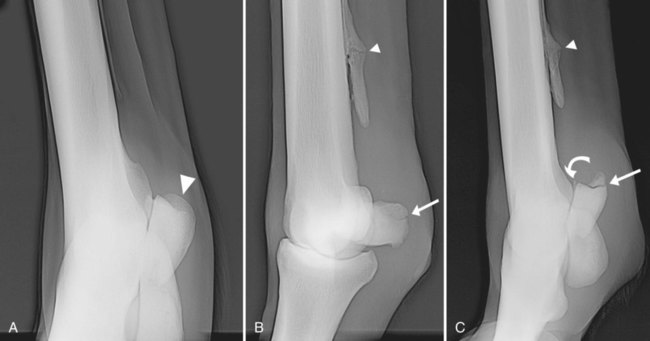
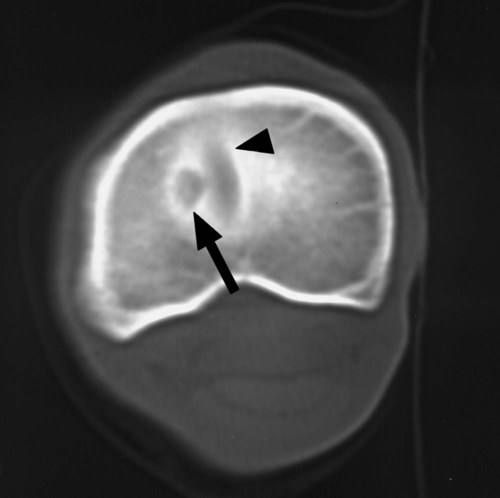
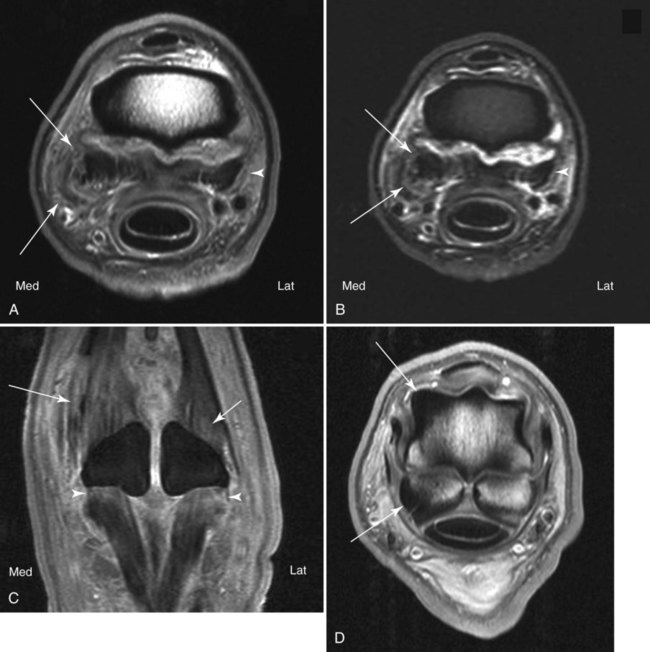
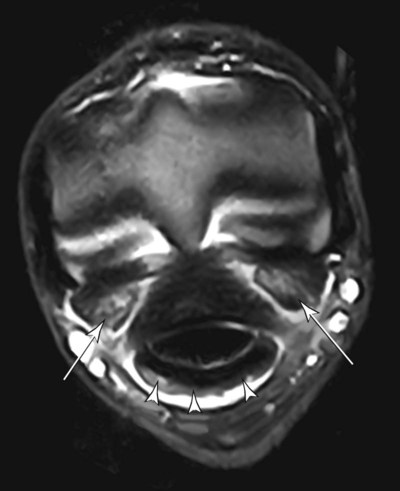
The anatomic structures of the metacarpophalangeal (MCP) and metatarsophalangeal (MTP) articulations are so similar that differentiating the right from the left or the forelimb from the hindlimb on unlabeled radiographs cannot be done reliably. The MCP or MTP articulations are hinge joints, formed by the distal end of the metacarpal (or metatarsal) bone and the proximal end of the proximal phalanx. The articular surface of the proximal phalanx is concave and has a sagittal groove opposing the sagittal ridge at the distal end of the third metacarpal (MC III) or the third metatarsal (MT III) bone. This ridge and groove divide the weight-bearing surface into two unequal parts. The largest surface is on the medial (or axial) side, where loading is greatest. The sagittal ridge of MC III or MT III is received into a depression at the palmar* surface that is created by the proximal sesamoid bones and the intersesamoidean ligament. The joint has two radii of articulation. The dorsal radius serves the weight-bearing portion, and the palmar radius conforms to the articulation with the proximal sesamoid bones.1 The junction of these radii of articulation often appears flat in lateral radiographs and may be confused with a lesion of the articular surface and subchondral bone. The joint capsule attachments at the proximal end of the proximal phalanx are immediately periarticular, with no redundant capsule or recesses. The capsule attaches to the distal end of MC III or MT III at the periarticular margins. Dorsally, a large recess extends proximally and forms a pouch that allows full extension of the joint. A bursa is interposed between the extensor tendons and the dorsal joint pouch. The palmar joint capsule extends proximal to the sesamoid bones between the suspensory ligament and MC III or MT III.1 Ligaments associated with the MCP and MTP articulations are described elsewhere.2 The intent of the radiographic examination is to visualize the articular and periarticular skeletal structures and the adjoining soft tissues adequately. The examination should include the proximal interphalangeal joint and the distal ends of the metacarpal or metatarsal bones. Identification markers are essential in radiographic examination of the MCP or MTP articulation; right versus left and front versus hind should be designated clearly. If oblique views are obtained, the direction the x-ray beam travels designates the name of the projection from entrance to exit. Markers should be placed to the lateral surface on all views, with the exception of the lateromedial view, for which markers should be placed dorsally.3 Survey radiographic examination of the joint should include a lateromedial, a dorsopalmar, and two oblique projections (dorsal 45-degree lateral-palmaromedial and dorsal 45-degree medial-palmarolateral), with the limb bearing weight if possible. The survey examination should precede any special radiographic projections or contrast studies of the joint. The lateromedial projection should be made with the primary beam centered at the articulation and directed parallel to an imaginary line connecting the collateral fossae at the distal end of MC III or MT III. A true lateromedial projection is essential for proper assessment of the sagittal ridge of distal MC III or MT III.4 The dorsopalmar projection warrants thoughtful positioning. Because the plane of the joint is at an angle to the solar surface of the hoof, the primary beam is directed from dorsoproximal to palmarodistal at approximately 30 to 40 degrees (dorsal 35-degree proximal-palmarodistal view). This should result in the projection of the proximal sesamoid bones over the distal aspect of MC III or MT III and the joint space projected with maximal width.5,6 The dorsal 45-degree lateral-palmaromedial and dorsal 45-degree medial-palmarolateral projections should be a routine part of the survey examination. These oblique views are necessary to view the abaxial aspects of the articular surfaces, the periarticular margins, and the proximal sesamoid bones. Oblique views made in a dorsal 60-degree lateral-palmaromedial or dorsal 60-degree medial-palmarolateral direction allow the best visualization of the dorsal eminence of the proximal phalanx, which is located near midline, and the axial aspect of the proximal sesamoid bones. Some prefer using the 60-degree oblique view as the routine oblique view rather than the oblique views made at 45 degrees because axial lesions may be common (Fig. 22-1).7 Additional projections of the joint may be indicated according to the information gained from survey radiographs.4 The lateromedial projection during flexion is performed while the foot is held off the ground as if the sole of the hoof were being inspected visually. Alternate positions include variations in the degree of flexion and flexed oblique views. These projections may provide better visualization of subarticular surfaces at the dorsal aspect of distal MC III or MT III, the proximal part of the proximal phalanx, and the articular margins of the proximal sesamoid bones.6 The dorsodistal-palmaroproximal projection is made while the limb is not bearing weight. In this study, a tangential view of the articular margin of the distal aspect of MC III or MT III is created. The foot is elevated on a block, and the limb extended. The primary beam direction is approximately 125 degrees to the axis of the metacarpal or metatarsal bone.8 The degree of flexion and the angle of the primary beam determine the tangent of the joint surface that is visualized. The palmaroproximal-palmarodistal projection is used to visualize the palmar articular surface of MC III or MT III and the proximal sesamoid bones. Positioning of the patient requires that the x-ray tube be placed close to the horse’s body. The limb should be positioned as far caudal as possible, and the foot is placed on a supporting tunnel containing a cassette.6 Inherent magnification results from the use of this projection because of the distance between the proximal sesamoid bones and the film cassette. The abaxial surfaces of the proximal sesamoids may be examined further by placing a cassette medial or lateral to the joint on the affected side. The x-ray beam is then directed in a dorsal 50-degree proximal, 45-degree lateral-distopalmaromedial or dorsal 50-degree proximal, 45-degree medial-distopalmarolateral direction, respectively, to create a tangential view of the proximal sesamoid bones.9 This positioning results in the x-ray beam being directed downward at the sesamoid bones at an angle of 50 degrees from horizontal. This tangential projection is beneficial in assessing whether articular involvement is present with sesamoid lesions and thus directs the surgical approach (Fig. 22-2, A and C). Ultrasound offers many advantages in evaluation of soft tissues surrounding the MCP or MTP joint and is used frequently to complement the radiographic examination. Portable ultrasound machines can be used to image the extensor and flexor tendons, the suspensory and distal sesamoidean ligaments, the synovial lining and joint recesses, collateral ligaments, and cortical margins. The normal sonographic features of the MCP and MTP joints have been described.10 In addition to conventional radiography, computed tomography (CT) may be useful in selected patients to image the MCP or MTP joint. CT excels in the evaluation of bones and is useful in imaging complex fractures and subchondral lesions in the MCP and MTP joints (Fig. 22-3). More recently, magnetic resonance (MR) imaging has been used to evaluate the distal limbs in horses, including the MCP or MTP joints.11–18 A distinct advantage of MR is the exceptional soft tissue contrast resolution (Figs. 22-4, 22-5, and 22-6). Additionally, MR imaging is multiplanar. MR examinations are commonly performed by using several types of acquisition sequences to demonstrate different anatomic and pathologic features. MR systems usually require that horses be under general anesthesia. There are MR systems available for imaging the limbs of standing horses. However, volume averaging and motion artifact remain limitations of these, especially proximal to the distal phalanx, although motion correction techniques improve resolution.19 Joint disease in many horses is often associated with repeated trauma, and the pathologic changes may be characteristic of the joint or function of the horse. A study of racetrack injuries has provided an overview of pathologic findings and pathogenesis of MCP or MTP joint disease.20 Lameness and distention of a joint are the initial clinical signs that typically precede the request for radiographic examination. The earliest signs of joint disease may remain obscure on radiographs because wear lines in the articular cartilage or synovial hypertrophy are usually not recognized. Radiographs of the contralateral joint may be obtained for comparison. Although pathologic change is often bilateral, it is usually in different stages of development between limbs, allowing for detection of changes. Joint effusion is usually a result of trauma, with degenerative changes in the articular surfaces and joint capsule. Radiographic signs include soft tissue swelling and joint distention. With chronic insults, dystrophic calcification of the periarticular soft tissues may also be present.21 Villonodular synovitis leads to a firm, nonfluctuating swelling at the dorsal aspect of the joint. The villonodular masses arise from enlargement of the synovial villi of the joint capsule and are associated with repetitive trauma. The condition is usually diagnosed by clinical signs, history, palpation, and ultrasound. With time, the radiographic signs will include mild to severe erosion of distal MC III or MT III at the region just distal to the dorsal joint capsule attachment.22–24 Periarticular bony proliferation may be present (Fig. 22-7).With arthrography, radiolucent, space-occupying masses of the synovial villus hypertrophy can usually be identified in the dorsal recess of the joint (Fig. 22-8).
The Equine Metacarpophalangeal and Metatarsophalangeal Articulation
Anatomy
Radiographic Examination
Alternative Imaging Modalities
Radiographic Interpretation of Diseases of the Metacarpophalangeal/Metatarsophalangeal Articulation
Joint Effusion
Villonodular Synovitis
The Equine Metacarpophalangeal and Metatarsophalangeal Articulation