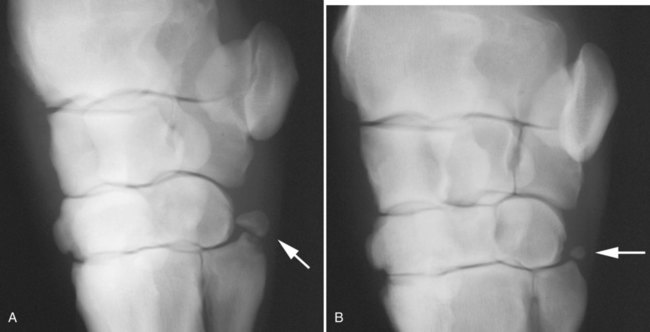
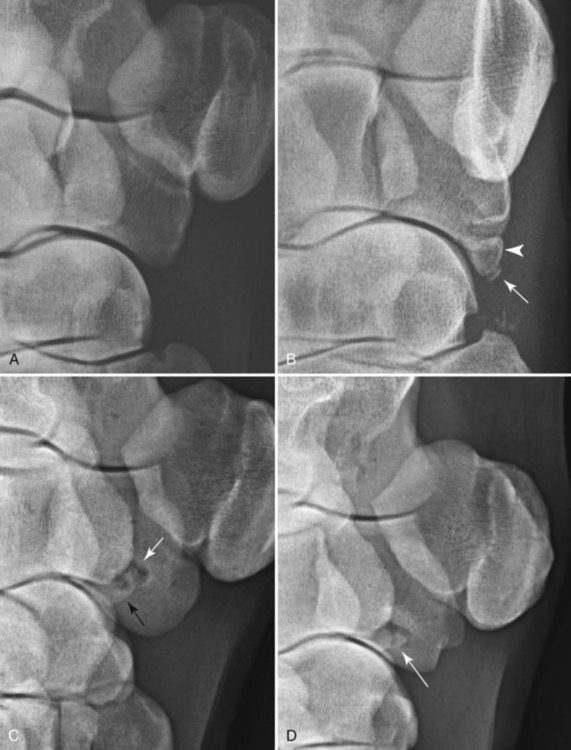
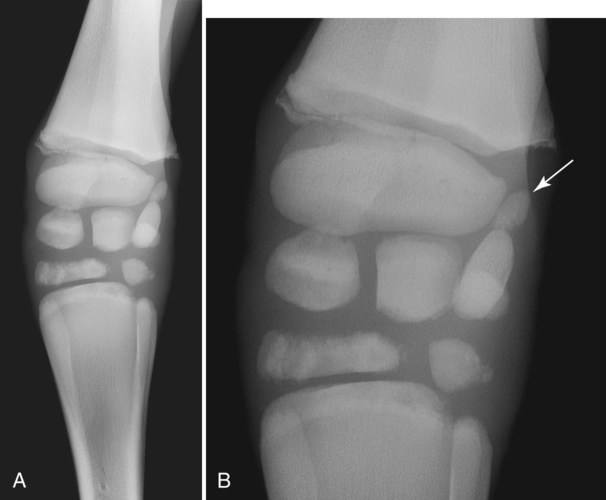
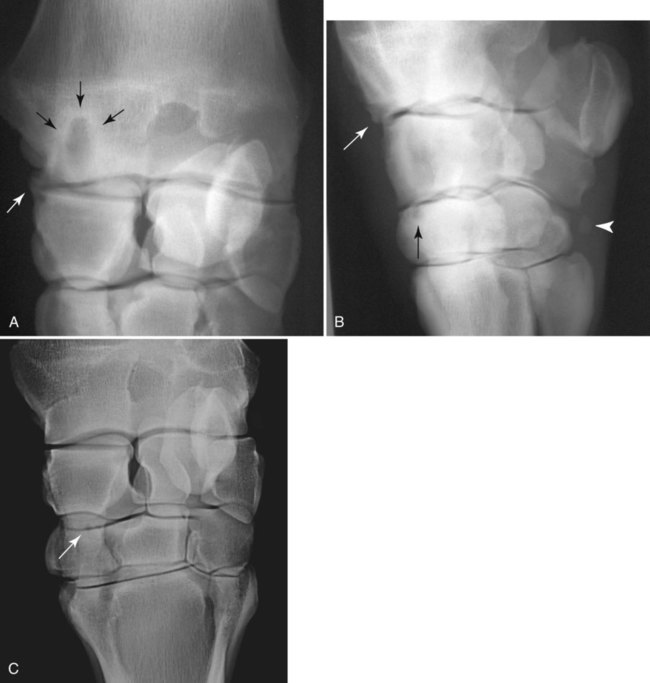
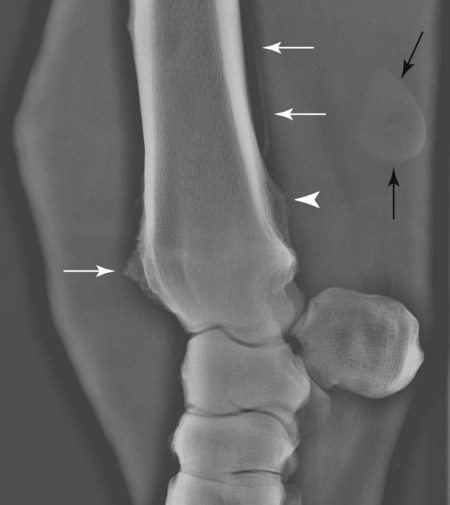
The equine carpus is composed of three main articulations: the antebrachiocarpal joint; the middle carpal joint, and the carpometacarpal joint. There are two rows of cuboidal bones interposed between the radius and metacarpus.1 The antebrachiocarpal joint is formed by the distal aspect of the radius proximally and the proximal row of carpal bones (radial, intermediate, ulnar, and accessory carpal bones) distally. The middle carpal joint is the articulation formed between the proximal (radial, intermediate, and ulnar carpal bones) and distal (second, third, and fourth carpal bones) rows of carpal bones. The carpometacarpal joint is the articulation between the distal row of carpal bones and the second, third, and fourth metacarpal bones. Vertically oriented joints between adjacent cuboidal carpal bones within each row are referred to as intercarpal joints. The antebrachiocarpal and middle carpal joints provide flexion and extension for the carpus, whereas the carpometacarpal joint is capable of only minimal motion. Within each row, the cuboidal carpal bones are connected by two interosseous ligaments, described as intercarpal ligaments, and two transverse dorsal ligaments.1 Within the middle carpal joint are two palmar ligaments, which attach the proximal and distal row of carpal bones. The medial palmar intercarpal ligament joins the radial with the second and third carpal bones, and the lateral palmar intercarpal ligament joins the ulnar with the third and fourth carpal bones. When the carpus is flexed, the radial carpal bone moves distally relative to the intermediate and ulnar carpal bones. The accessory carpal bone, situated on the palmar aspect of the carpus, articulates with the distal lateral aspect of the radius and the ulnar carpal bone.2,3 The presence of the first and fifth carpal bones is variable, as is their shape and size and proximity to adjacent bones (Figs. 20-1 and 20-2). These bones should not be confused with osteochondral fragments. The first carpal bone occurs in approximately 30% of horses but varies widely in size and may articulate with one or both of the second carpal and metacarpal bones.3,4 The fifth carpal bone occurs rarely, reported as an incidence of 1.4%.4 Lucent zones in the fourth carpal bone at the site of articulation of the fifth carpal bone, and in the second carpal bone and the proximal aspect of the second metacarpal bone at the site of articulation of the first carpal bone (see Fig. 20-1), are a normal feature of these articulations and should not be misinterpreted as a lytic lesion. The first and fifth carpal bones are more likely to be present bilaterally, whereas radiolucent areas in the second carpal and metacarpal bones are more commonly unilateral.4 The accessory carpal bone may occasionally develop from more than one center of ossification. Fusion usually occurs, but radiographic separation may be identified during the first 6 months of age.3,5 Incidental findings in the distal aspect of the radius include medial and lateral protrusions of the cortex at the distal radial physis in a mature horse (Fig. 20-3, A), noted particularly on oblique projections. The caudal aspect of the radius may be slightly irregular immediately proximal to the physis.6 Until fusion of the distal radial and distal ulnar epiphyses occurs, a radiolucent line or rounded radiolucency may remain in the distal radial epiphysis (Fig. 20-3, B), possibly with a notch in the articular surface at this location. Vestigial remnants of the ulna may occur in some horses and are visible radiographically when ossification of a fibrous remnant occurs (Fig. 20-3, C).3 Small radiolucent zones may occur within any carpal bone, but especially within the ulnar and second carpal bones, the majority of which are of no clinical significance. The palmar aspect of the ulnar carpal bone can be of variable shape; the distopalmar aspect of the bone could be bilobed, rounded, pointed, or fragmented, in addition to having a simple shape (Fig. 20-4).4 One or more osseous fragments on the palmar aspect of the ulnar carpal bone can also be seen as an incidental finding, usually in association with a lucent area in the ulnar carpal bone (see Fig. 20-4). Occasionally, separate centers of ossification are also identified on the palmaromedial or palmarolateral aspect of the proximal row of carpal bones. The articulations between the carpal bones should not be confused with sagittal plane fractures of the third carpal bone.7 For example, in dorsoproximal-dorsodistal (skyline) views of the distal row of carpal bones, the articulation between the third and fourth carpal bones should not be confused with a parasagittal fracture of the lateral aspect of the third carpal bone (Fig. 20-5). On the dorsomedial-palmarolateral oblique view, the articulation between the second and third carpal bones should not be confused with a parasagittal fracture of the medial aspect of the third carpal bone. Variations in carpal bone shape and structure can depend on the training history of the horse. For example, in horses that have raced or undergone strenuous galloping training, smooth enlargement or modeling of the dorsal aspect of carpal bones is found frequently, and entheseous new bone on the dorsal surface of the carpal bones as the only radiologic abnormality may be insignificant clinically.3 Training also has an effect on subchondral and cancellous bone density and mineralization. Therefore horses worked on a soft surface with low training intensity are likely to have thinner subchondral bone at the carpal articular surfaces and less dense cancellous bone than horses with a history of strenuous galloping exercise.8 This should be taken into account when evaluating radiographs and be differentiated from the severe subchondral bone sclerosis in the third carpal bone that may be associated with osteochondral and slab fractures.9 Interpretation of the clinical significance of sclerosis of the radial facet of the third carpal in both Thoroughbred and Standardbred racehorses may require nuclear scintigraphy to distinguish between adaptational versus pathologic changes. Increased radiopacity of the third carpal bone can also be recognized in sport horses undergoing high-intensity exercise, including eventing, show-jumping, and endurance horses. Distal radial physitis is seen most commonly in horses from 4 to 12 months of age,10 although the distal radial physis in horses up to 2 years old that have recently entered training may also be affected.11,12 Physitis occurs when endochondral ossification in the metaphyseal growth cartilage is disrupted.11 Standard views are recommended, although the dorsopalmar may be most useful. The physis appears wider with irregular margins as a result of remodeling of the surrounding metaphysis (Fig. 20-6). The physis appears flared at the edges from periosteal new bone formation, with the edges of the physis appearing to protrude from the surface of the cortex on both proximal and distal aspects of the physis.3,11 Associated soft tissue swelling may be present at the site. Premature or dysmature foals may have incomplete ossification of the carpal bones at birth (Fig. 20-7). This may lead to secondary angular limb deformity resulting from collapse of the poorly ossified carpal bones being unable to withstand the forces of normal weight bearing.13,14 Although a dorsopalmar view is the most useful for assessing the degree of deformity,13,14 obtaining a full radiographic series is recommended because carpal bone deformity exists in a variety of configurations. The carpal bones appear small and rounded, without their normal cuboidal shape (Fig. 20-8).3,15 Relative enlargement of intercarpal joint spaces is therefore present. Angular limb deformity may be noted on radiographs, with the deformity at the level of the carpal bones and not the distal radial physis.3,13,13 Collapse and malformation of one or more carpal bones may be observed in severe cases. Angular limb deformities can arise from congenital, developmental, or acquired conditions.13,14,16–18 Congenital problems relate to in utero factors such as positioning, infective or chemical insult, nutrition, and skeletal maturity at birth. Developmental abnormalities have been attributed to a variety of factors associated with developmental orthopedic disease, including nutrition, exercise, and overloading, although damage to one side of the joint, epiphysis, or physis leading to asymmetric growth will be exaggerated in a developing horse. Acquired deformities may be the result of trauma, including fracture, or infection. Extended dorsopalmar views, including as much as possible of the distal aspect of the radius and the proximal aspect of the metacarpal region, are the most useful images in the majority of horses (Fig. 20-9).3,16 Standard radiographic views are required for assessing severe deformity, if onset is acute or swelling or lameness is present. On dorsopalmar views, the long axis of the radius is out of line with the long axis of the third metacarpal bone. At the level of carpus, valgus deformity (lateral deviation of the distal aspect of the limb) is observed most frequently, but varus deformity (medial deviation) does occur. The location of the abnormality is usually at the level at which maximal deviation occurs. By drawing lines bisecting the long axis of radius and the long axis of the third metacarpal bone, the level of deviation can be determined (see Fig. 20-8). When an angular limb deformity is not present, the lines drawn through the long bones should be continuous. However, when a deviation is present, these lines intersect at the level of maximal deviation, giving a guide to the structures involved. This technique can also be useful for measuring the degree of deformity and monitoring response to treatment. Variation in obliquity of sequential radiographs can alter the degree of deviation assessed from the intersecting lines. Another guide to normal alignment is the positioning of the joint surfaces. When no abnormality is present, the articular surfaces of the antebrachiocarpal, middle carpal, and carpometacarpal joints should be parallel and perpendicular to the long axis of the limb. With joint-based abnormalities, a loss of articular surface alignment in the affected joint(s) may occur.3,14,14 Abnormalities that can be observed include the following, which can be targeted on the basis of the level of maximal deviation.3,13,14,16–18 Diaphyseal deformity: This occurs only rarely. The site of maximal deviation is at the level of the diaphysis, making a straight line bisecting the affected long bone impossible to draw. Distal radial physis abnormality: On dorsopalmar radiographs, the physis may be wider on the medial or lateral aspect and narrower or fused on the opposite side. This is associated with deviation away from the wider side, because metaphyseal growth continues on that side but is restricted on the contralateral closed aspect of the physis. Location of maximal deviation is at the level of the distal radial physis. Epiphyseal growth imbalance: The distal radial epiphysis may appear wedge-shaped on dorsopalmar radiographs. This may result from dysplasia of the distal radial epiphysis. The lateral styloid process may also be characterized by delayed development. Fusion of the distal radial and distal ulnar epiphyses should occur between 3 and 6 months of age. Altered development of the distal ulnar epiphysis can be seen as lack of growth on the lateral aspect of the distal radius. Location of maximal deviation is at the level of the epiphysis, and the distal radial physis and antebrachiocarpal articular surfaces are no longer parallel. Incomplete ossification of carpal bones: In severe ossification defects, collapse or deformity of one or more incompletely ossified carpal bones may occur, resulting in angular limb deformity. Location of maximal deviation is at the level of the carpal bones where the collapse or deformity occurs. Lines through the joint spaces may no longer be parallel. Flaccidity or damage to periarticular structures: Location of maximal deviation may be variable, although it is often at the distal articular surface of the radius. Widening of joint space(s) on one side may occur, although the degree of deformity can vary if medial or lateral stresses are applied. Subchondral or osseous cystlike lesions occur in the carpal bones, the proximal aspect of the second or fourth metacarpal bones, and the distal aspect of the radius, with or without an articular component.3,19 The most commonly reported site is the ulnar carpal bone. Osseous cystlike lesions in the proximal aspect of the second metacarpal bone seem to occur most frequently when a first carpal bone is present (see Fig. 20-1) and may occur in conjunction with a cystlike lesion in the first carpal bone. Osseous cystlike lesions are noted frequently as an incidental finding, but some are associated with lameness.20 Generally, those situated deep in the bone, particularly in the first, second, and ulnar carpal bones, and proximal aspect of the second metacarpal bone, are unlikely to be associated with lameness. However, lesions associated with articular margins and subchondral cystlike lesions in the distal medial aspect of the radius are more likely to be clinically significant (Fig. 20-10).21 Lameness can vary in severity and progression, and clinical progression may not closely relate to radiological signs. Scintigraphic imaging can give guidance about the current activity of the bone around the cystic lesion. Osseous cystlike lesions are generally considered developmental abnormalities, but trauma to the articular cartilage and subchondral bone can potentially lead to formation of these cystlike lesions.22 Osseous cystlike lesions in the ulnar carpal bone with or without an adjacent osseous fragment have been linked to tearing of the attachment of the lateral palmar intercarpal ligament and associated with lameness.22 Occasionally an osseous cystlike lesion is seen in association with injury of a transverse intercarpal ligament (Fig. 20-10, C). If cystlike lesions are observed in a foal, then osteomyelitis should be considered and other procedures used to investigate the presence of septic foci. Subchondral or osseous cystlike lesions are well-circumscribed circular or semicircular lucent areas within the carpal bones, the distal aspect of the radius, or in the proximal aspect of the second or fourth metacarpal bones. An area of opacity may surround the lucent zone. For articular lesions, clear communication with the articular surface may be present, although more frequently the lesions are adjacent to the articular surface and a clear communication cannot be established radiographically. Radiographic evidence of secondary osteoarthritis may be visible (Fig. 20-10, A and B). The following conditions are associated with swelling on the dorsal aspect of the carpal region. A carpal hygroma is a subcutaneous sac or acquired bursa usually positioned over the dorsal aspect of the carpal region.7 A hygroma usually occurs as a result of blunt trauma at the site and is generally nonpainful, although it may have been painful at the site when the inciting event occurred. Gait alteration is not generally observed unless the hygroma is so large that carpal flexion is restricted. Rupture of the extensor carpi radialis tendon should be considered in neonatal or young foals with distention of the tendon sheath of the extensor carpi radialis, particularly if flexural deformity is also present.23,24 In horses of any age, traumatic or septic damage to an extensor tendon sheath may occur, potentially with coexisting tendon damage. Ultrasonographic examination is often more useful in assessment of these injuries than is radiographic examination, although the use of radiography with contrast-medium injection adds information about communication between synovial cavities. To determine if communication exists between the carpal joints and tendon sheath(s), double-contrast techniques may also be useful. Contrast-medium injection can also be used to identify filling defects associated with adhesion formation or synovial proliferation. Radiographs are characterized by soft tissue swelling over the dorsal aspect of the carpus. Swelling may be more defined in the region of the tendon sheath. Chronic synovitis may be associated with periosteal new bone formation on adjacent structures. In particular, extensor carpi radialis synovitis may be associated with periosteal new bone on the cranial distal aspect of the radius (Fig. 20-11).24
The Equine Carpus
Anatomy
Normal Variations
Abnormalities
Developmental
Distal Radial Physitis/Epiphysitis
Incomplete Ossification of Carpal Bones
Angular Limb Deformities
Osseous or Subchondral Cystlike Lesions
Soft Tissue Problems
Periarticular Soft Tissues
Carpal Hygroma.
Distention/Synovitis of Extensor Carpi Radialis, Common Digital Extensor, or Long Digital Extensor Tendon Sheaths.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree